Overview
Healthcare clearinghouses are pivotal in the healthcare system, facilitating the electronic exchange of information between providers and payers. This process significantly enhances the accuracy and efficiency of claims processing.
These entities standardize data formats to minimize errors and denials, which is crucial in maintaining operational integrity. Furthermore, they offer essential services such as:
- Eligibility verification
- Electronic remittance advice
These services are vital for ensuring financial stability within medical practices. By streamlining these processes, healthcare clearinghouses not only improve operational efficiency but also foster trust and transparency in the healthcare ecosystem.
Introduction
In the complex realm of healthcare, clearinghouses have emerged as a critical pillar of efficiency and accuracy in claims processing. These organizations serve as essential intermediaries, effectively bridging the divide between healthcare providers and payers, thereby ensuring a seamless and error-free flow of information.
As the healthcare landscape continues to evolve, particularly in 2025, the importance of clearinghouses is set to escalate. Their capacity to standardize data formats and enhance compliance with regulatory standards is proving to be indispensable. Given the intricacies of medical coding and the growing demand for timely reimbursements, it is vital for providers and pharmaceutical professionals to grasp the operations, benefits, and selection criteria of healthcare clearinghouses.
This article explores the multifaceted roles these entities play, emphasizing their influence on operational efficiency and the overall financial health of healthcare organizations.
Define Healthcare Clearinghouses and Their Role in the Healthcare System
Healthcare clearinghouses are essential entities that facilitate the electronic transfer of healthcare information between providers, such as hospitals and clinics, and payers, including insurance companies. Serving as mediators, they guarantee that requests are handled precisely and effectively. By transforming non-standard data formats into standardized ones, organizations simplify the submission process, greatly decreasing the chances of mistakes and rejections.
In 2025, the function of medical processing centers has become increasingly essential as the medical system continues to advance. They not only improve the efficiency of processing requests but also aid in adhering to regulatory standards, such as HIPAA. Recent statistics suggest that the utilization of intermediary organizations can result in a decrease in denial rates by as much as 30%, highlighting their significance in preserving the flow of information within the medical ecosystem. Furthermore, with ICD-10 containing over 68,000 codes for various diagnoses and treatments, including conditions like diabetes, hypertension, and cancer, the intricacy of processing requires the proficiency of intermediaries to handle such information efficiently.
The significance of healthcare clearinghouses goes beyond simple processing of requests; they also offer vital services like eligibility verification and electronic remittance advice. These services assist in guaranteeing that providers obtain prompt reimbursements for their offerings, which is essential for sustaining financial stability in medical practices. As mentioned by Steve Alder, Editor-in-Chief of The HIPAA Journal, “However, while it’s not a requirement, many healthcare providers opt to use healthcare clearinghouses due to the advantages they provide – including eligibility verification, electronic remittance advice, and the capability to manage various medical submissions.”
In the context of Medicare, intermediary organizations play a critical role in assisting providers in navigating the complexities of patient treatment pathways. They aid in overseeing requests associated with different Medicare benefits, ensuring that providers can efficiently monitor interventions from diagnosis through lines-of-therapy. For instance, Medicare Part D Plans have specific approval processes for treatments, and intermediaries assist in facilitating these claims, ensuring that providers can navigate the requirements efficiently. Specialist views emphasize the importance of intermediaries in the current medical environment. Many healthcare professionals support the use of healthcare clearinghouses, noting that while not mandatory, these entities provide significant advantages that improve operational efficiency. For example, a case study on the adjudication of medical requests illustrates how intermediaries assist the review process by payors, determining whether submissions will be accepted for reimbursement or denied due to insufficient coverage or lack of pre-authorization. In instances of denial, patients may need to appeal for coverage, while rejected requests can be resubmitted after correcting any errors, ensuring that providers can still seek payment for services rendered.
Overall, medical billing entities play a crucial role in the medical system, influencing claims processing efficiency and supporting the financial well-being of providers. Their ability to adapt to the complexities of medical data exchange positions them as essential partners in the ongoing effort to enhance patient care and operational effectiveness. Furthermore, the connections among HCPCS, ICD, DRGs, and NCDs are essential for comprehending the treatment pathways and interventions that providers employ, highlighting the necessity for intermediaries in managing these complex relationships.

Explain How Healthcare Clearinghouses Operate in Claims Processing
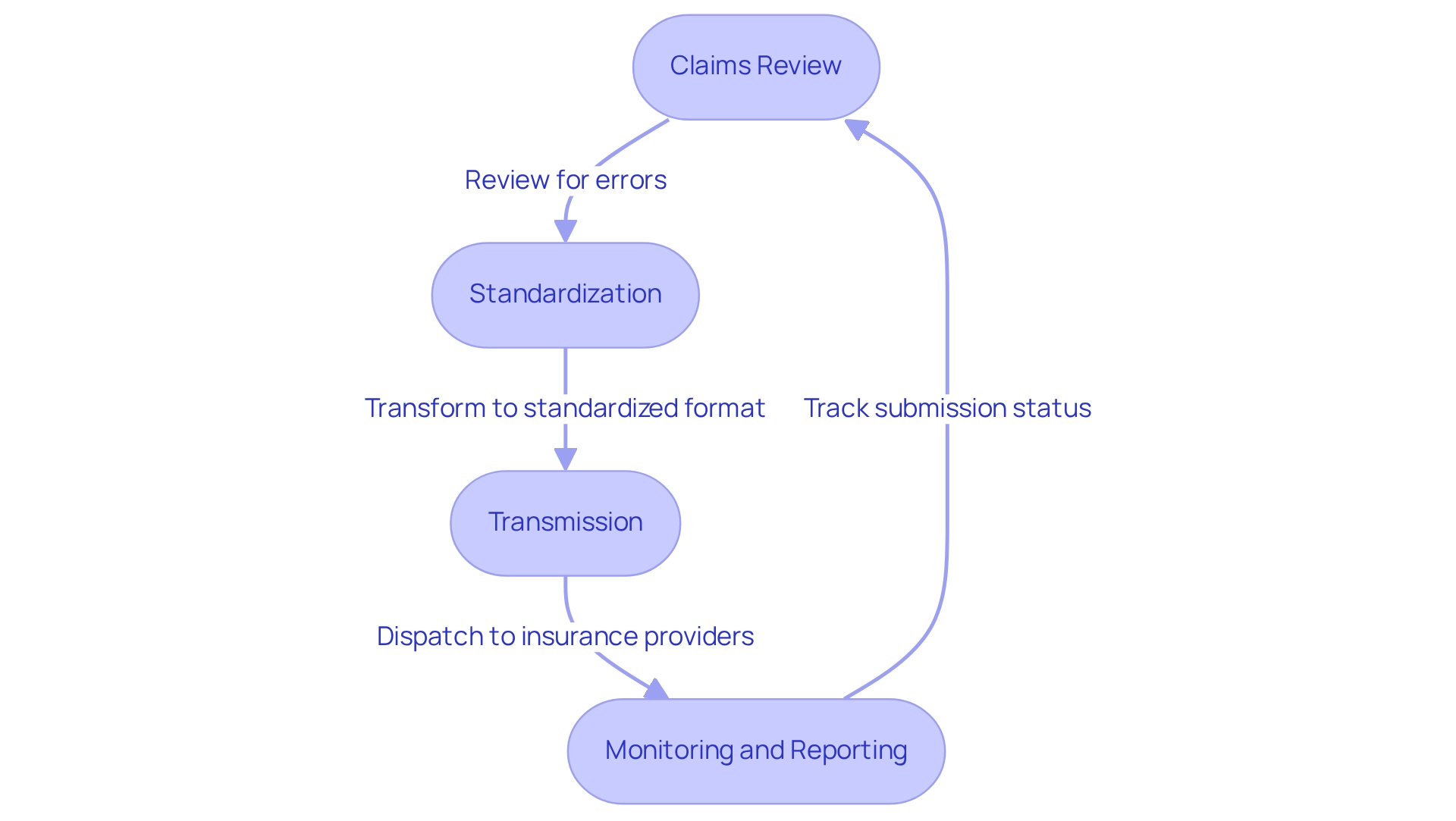
Healthcare clearinghouses are pivotal in the processing system, adeptly managing the exchange of information between healthcare providers and payers. Their operations encompass several essential functions:
-
Claims Review: Clearinghouses meticulously scrutinize submissions for errors, ensuring that all required details are correctly formatted. This scrubbing process is crucial for identifying potential issues that could result in denials, thereby significantly enhancing submission accuracy.
-
Standardization: Claims are transformed into a standardized format that aligns with various payer systems. This standardization streamlines communication and diminishes the likelihood of errors during transmission.
-
Transmission: After review and standardization, data processors dispatch requests to the appropriate insurance providers for processing. This step is vital for ensuring timely payments and minimizing delays.
-
Monitoring and Reporting: Many intermediaries offer tracking services that enable providers to monitor the status of their submissions. This transparency provides valuable insights into any challenges that may arise during processing, facilitating prompt resolution.
The operational framework of healthcare clearinghouses not only enhances submission precision but also significantly reduces the time required for providers to receive payments. Clients utilizing clearinghouse services experience, on average, a 15% enhancement in cash flow and a 40% decrease in denials within just 60 days, as highlighted by Lori Zindl. This efficiency is further bolstered by emerging trends in 2025, where advancements in AI are being harnessed to simulate financial scenarios, supporting revenue forecasting and financial planning.
Moreover, case studies underscore the efficacy of AI in bolstering processing integrity by detecting unusual patterns and ensuring compliance with medical regulations. For instance, the case study titled “Fraud Detection and Compliance in AI Systems” illustrates how AI systems can enhance the integrity of processing requests. By focusing on denial prevention, healthcare clearinghouses improve operational efficiency and enhance patient care outcomes, solidifying their role as a crucial component of the revenue cycle in healthcare. Additionally, CareSet’s integration of over 100 external data sources enriches data management and amplifies processing efficiency, ensuring that clients gain comprehensive insights into treatment pathways and approval processes across Medicare A, B, and D benefits.
Highlight the Benefits of Utilizing Healthcare Clearinghouses for Pharmaceutical Professionals
Highlight the Benefits of Utilizing Healthcare Clearinghouses for Pharmaceutical Professionals
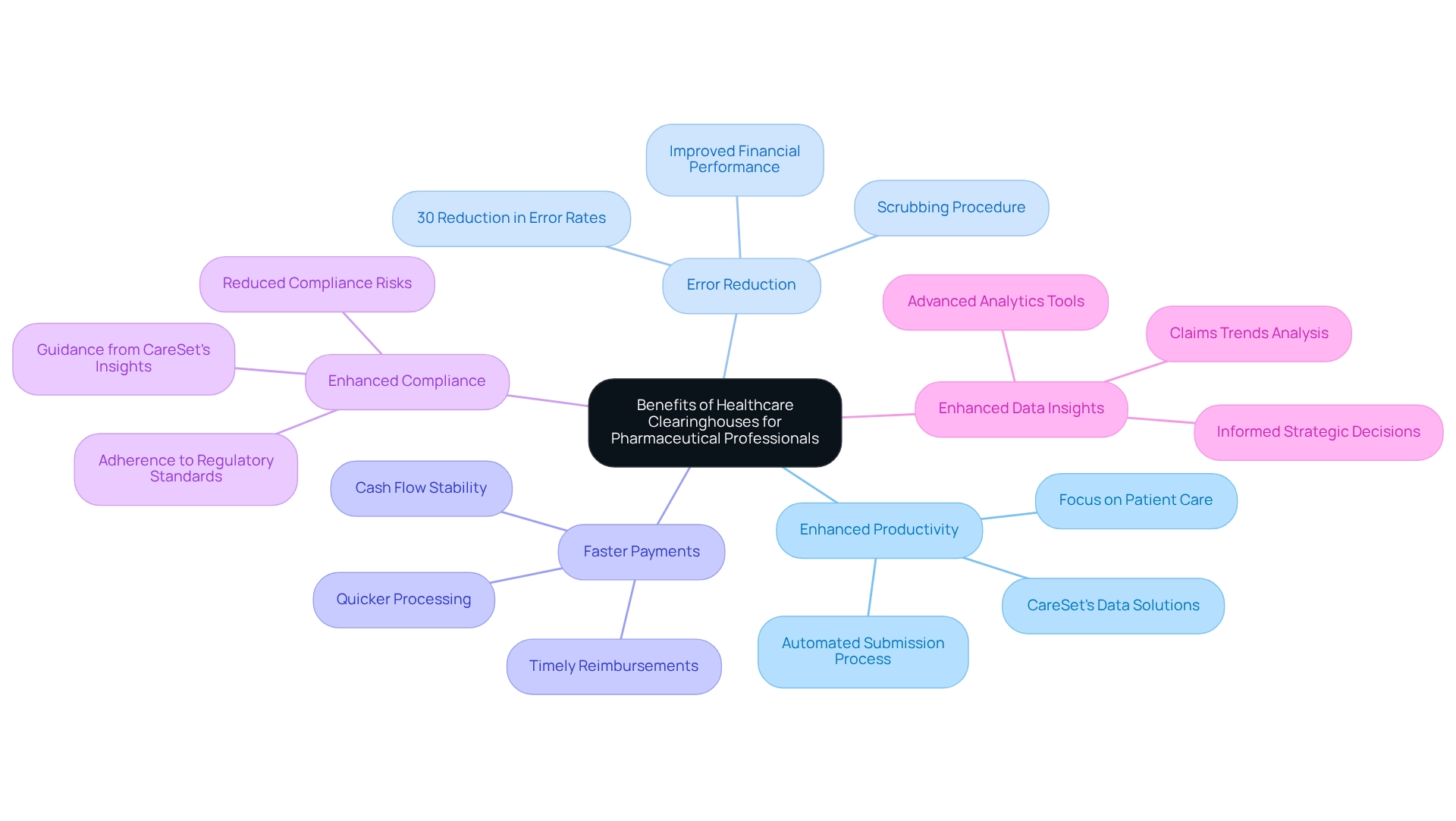
Utilizing healthcare clearinghouses offers numerous advantages for pharmaceutical professionals, including enhanced productivity, error reduction, faster payments, enhanced compliance, and improved data insights.
-
Enhanced Productivity: Automating the submission process substantially alleviates the administrative burden on medical providers, enabling them to concentrate more on patient care. This efficiency is crucial in a landscape where healthcare organizations face challenges such as lack of standardization and diverse systems in electronic processing. CareSet’s comprehensive data solutions further augment this efficiency by providing actionable insights that streamline operations.
-
Error Reduction: The scrubbing procedure employed by financial intermediaries minimizes the likelihood of requests being rejected due to errors, which can cause delays in reimbursement. Data reveals that submissions processed through healthcare clearinghouses experience a significant reduction in error rates, with studies indicating reductions of up to 30%. This enhancement in accuracy contributes to improved overall financial performance, aligning with CareSet’s commitment to delivering precise Medicare insights.
-
Faster Payments: Streamlined procedures result in quicker processing, leading to faster payments to providers. This is particularly advantageous for pharmaceutical companies that depend on timely reimbursements to sustain cash flow and operational stability. CareSet’s data solutions can assist in identifying trends that promote quicker payment cycles.
-
Enhanced Compliance: Healthcare clearinghouses play a vital role in ensuring that submissions adhere to regulatory standards, thereby reducing the risk of compliance issues that may result in penalties. This compliance support is essential for pharmaceutical professionals navigating complex healthcare regulations, and CareSet’s insights can guide companies in effectively maintaining compliance.
-
Enhanced Data Insights: Numerous data repositories offer advanced analytics and reporting tools that empower pharmaceutical companies to glean insights into claims trends and patient demographics. These insights are invaluable for informing strategic decisions and optimizing market access strategies. CareSet’s Medicare insights specifically provide a deeper understanding of patient needs and pharmaceutical utilization, enhancing decision-making capabilities.
As we look towards 2025, the role of intermediaries continues to evolve, with an increasing emphasis on their ability to enhance data insights and operational efficiency. Industry experts highlight that investing in outsourced services like healthcare clearinghouses allows internal teams to focus on critical aspects of maintenance and patient experience. Srivalli Harihara, Senior Manager of Coding Education, states, “Investing in the support of outsourced services can also allow internal teams more time to concentrate on other aspects of maintenance and patient experience.” This ultimately drives better outcomes in the pharmaceutical sector. A well-chosen healthcare clearinghouse not only streamlines revenue cycles but also strengthens relationships with insurance carriers, positively influencing the financial health of pharmaceutical companies. Furthermore, medical organizations should consider potential cost reductions when selecting claim adjudication service providers, as these savings can significantly impact the bottom line.
Guide on Choosing the Right Healthcare Clearinghouse for Your Needs
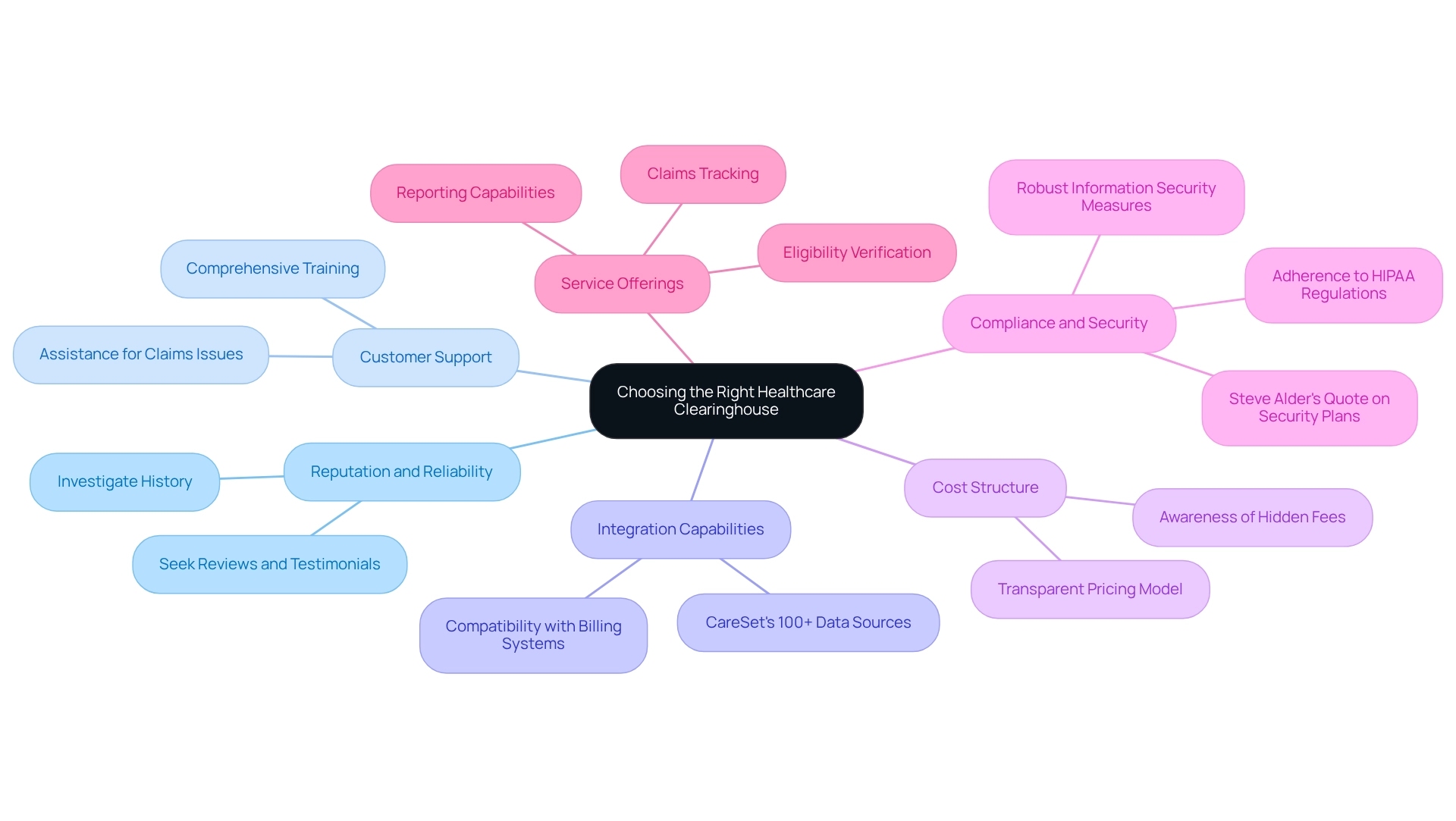
When selecting healthcare clearinghouses, it is essential to evaluate several key factors to ensure optimal performance and alignment with your organizational needs.
- Reputation and Reliability: Investigate the clearinghouse’s history and industry standing. Seek out reviews and testimonials from other healthcare providers to gauge their experiences. This foundational knowledge establishes a baseline for trust and reliability.
- Customer Support: Robust customer support is crucial. Confirm that the clearinghouse offers comprehensive training and assistance for resolving claims issues, which can significantly impact operational efficiency. Effective support not only enhances user experience but also fosters long-term partnerships.
- Integration Capabilities: Assess whether the clearinghouse can seamlessly integrate with your existing billing systems and electronic health records (EHR). This compatibility is vital for streamlining workflows and minimizing disruptions. For instance, CareSet incorporates over 100 external information sources for its analysis, emphasizing the significance of compatibility with diverse data sources. CareSet’s comprehensive Medicare information solutions enable healthcare organizations to leverage these integrations for improved decision-making and strategic growth.
- Cost Structure: Understand the clearinghouse’s pricing model, including any potential hidden fees. A transparent cost structure is essential for budgeting and financial planning within healthcare clearinghouses, allowing organizations to allocate resources effectively.
- Compliance and Security: Ensure that the clearinghouse adheres to HIPAA regulations and implements robust information security measures to protect sensitive patient details. This is increasingly important in light of recent incidents, such as GoodRx Holdings Inc. being fined $1.5 million for failing to notify consumers about impermissible disclosures of personal health information. As Steve Alder, Editor-in-Chief, notes, “The requirements to implement and test a data backup plan, an emergency mode operations plan, and a disaster recovery plan fall within the contingency plan standard of the Security Rule.”
- Service Offerings: Evaluate the range of services provided, such as eligibility verification, claims tracking, and reporting capabilities. These services should align with your specific operational needs to enhance overall efficiency.
In 2025, customer satisfaction ratings for healthcare intermediaries will be a critical metric to consider, reflecting the effectiveness and reliability of these services. Additionally, expert advice emphasizes the importance of compliance and the classification of clearinghouses, which can significantly influence operational success. A case study titled ‘Long-Term Strategic Growth for Healthcare Partners’ demonstrates how CareSet’s comprehensive approach not only meets urgent information needs but also promotes long-term strategic development and improves patient outcomes. By carefully considering these factors, healthcare organizations can make informed decisions that not only meet immediate data needs but also support long-term strategic growth.
Conclusion
The role of healthcare clearinghouses within the healthcare ecosystem is undeniably crucial, particularly as the industry navigates the complexities of claims processing and regulatory compliance. These entities streamline the exchange of information between providers and payers, significantly reducing errors and enhancing the efficiency of claims submissions. By converting non-standard data into standardized formats, clearinghouses facilitate smoother transactions and play an essential role in ensuring timely reimbursements, which are vital for the financial health of healthcare organizations.
Moreover, the benefits of utilizing healthcare clearinghouses extend beyond operational efficiency. They contribute to improved compliance with regulations, faster payments, and reduced error rates, ultimately supporting pharmaceutical professionals in maintaining cash flow and enhancing strategic decision-making. The integration of advanced technologies, including AI, further bolsters their capabilities, allowing for more accurate claims processing and insightful data analytics.
As the healthcare landscape evolves, particularly in 2025, the significance of selecting the right clearinghouse cannot be overstated. Organizations must consider factors such as reputation, customer support, integration capabilities, and compliance standards to ensure that their chosen clearinghouse aligns with their operational needs. By making informed decisions, healthcare providers and pharmaceutical professionals can leverage the full potential of clearinghouses to drive efficiency, enhance patient care, and secure their financial future in a competitive marketplace.


