Overview
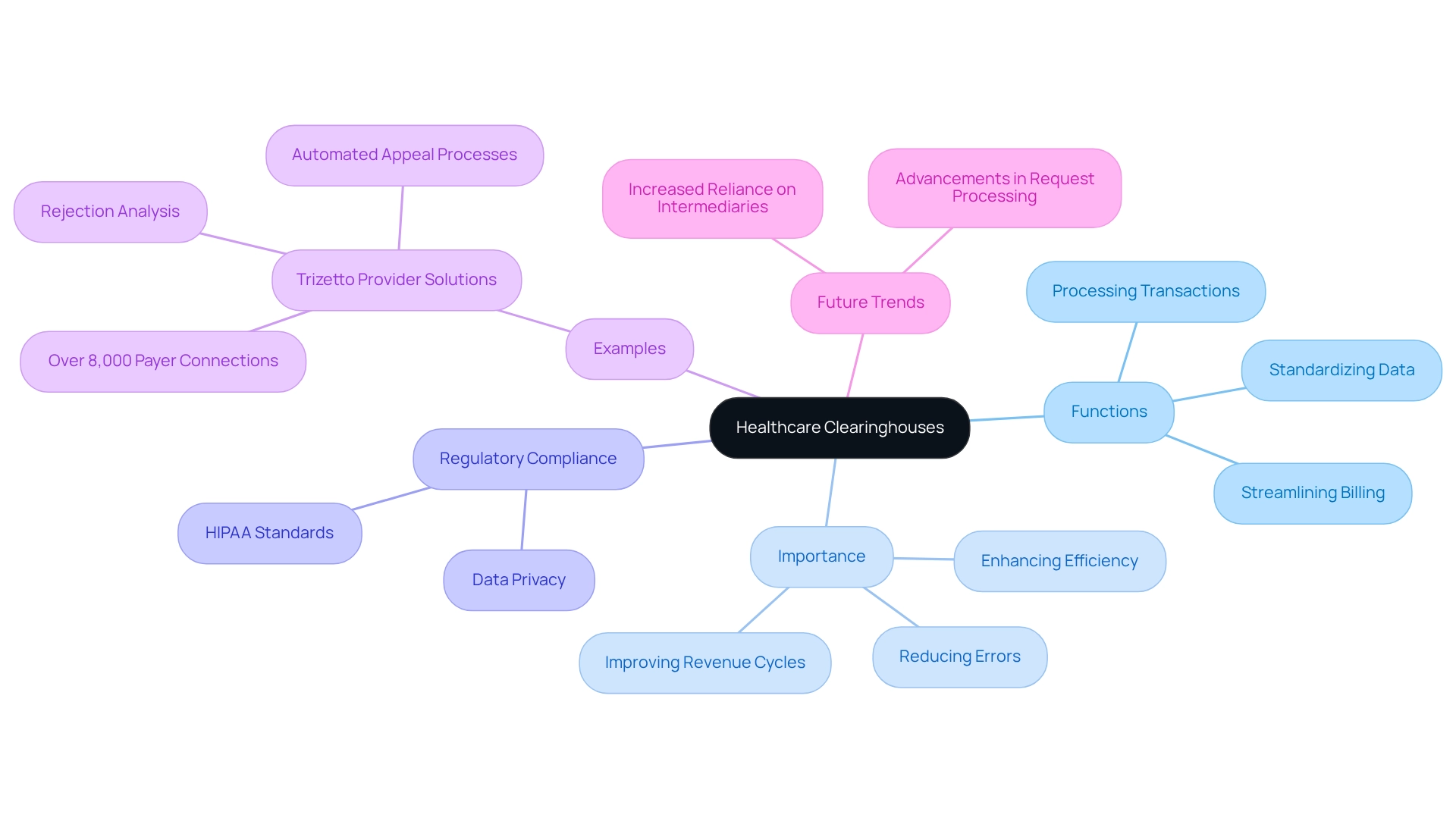
Healthcare clearinghouses function as pivotal intermediaries that streamline the processing of electronic medical transactions. They convert nonstandard information into standardized formats, thereby enhancing efficiency and minimizing errors in claims processing. This role is crucial as it not only validates claims but also ensures compliance with regulations such as HIPAA. Ultimately, these processes contribute to the financial health of healthcare providers by expediting payment cycles and alleviating administrative burdens.
Introduction
In the intricate world of healthcare, clearinghouses emerge as pivotal players that facilitate seamless communication between providers and payers. These essential intermediaries transform nonstandard health information into standardized formats, ensuring that claims are processed with accuracy and efficiency.
As the healthcare landscape grows increasingly complex, the significance of clearinghouses becomes even more pronounced, especially with the rise of advanced technologies and regulatory demands.
The advantages of utilizing a healthcare clearinghouse are numerous, ranging from minimizing errors to enhancing compliance and improving cash flow.
This article explores the fundamental functions of clearinghouses, their operational mechanisms, and the critical factors that healthcare providers should consider when selecting the appropriate clearinghouse to optimize their claims processing and overall financial health.
Define Healthcare Clearinghouses and Their Role in Healthcare
Medical intermediaries, often referred to as health care clearinghouses, are essential third-party organizations that facilitate the processing of electronic medical transactions among providers, payers, and other entities. They act as connectors, transforming nonstandard health information into standardized formats, ensuring precise transmission and processing of requests.
By bridging the gap between medical service providers and insurance firms, the health care clearinghouse streamlines the billing process, significantly reduces errors, and enhances the overall efficiency of request management. The role of the health care clearinghouse is particularly critical in maintaining compliance with regulatory standards, such as HIPAA, which governs the privacy and security of patient data.
As of 2025, the increasing reliance on intermediaries underscores their growing importance in the healthcare landscape, particularly concerning Medicare data solutions that leverage insights from over 62 million beneficiaries and 6 million providers, facilitated by health care clearinghouses, to improve healthcare strategies. Recent advancements highlight the necessity for effective request processing and improved billing practices to optimize revenue cycles.
For instance, Trizetto Provider Solutions exemplifies the effectiveness of transaction facilitators, managing various types of submissions with direct payer connections across the U.S., Puerto Rico, and Guam. With over 8,000 payer connections, Trizetto offers features such as rejection analysis and automated appeal processes, aiding clients in streamlining submission management and minimizing errors.
These features specifically address the challenges providers face in efficiently managing claims as they navigate patient treatment pathways from diagnosis through lines-of-therapy, and the health care clearinghouse is pivotal in electronic transactions, ensuring all parties adhere to standardized protocols, which enhances the speed and accuracy of claims processing.
As Steve Alder, Editor-in-Chief of The HIPAA Journal, emphasizes, integrating intermediaries into the medical system is vital for improving transaction efficiency and compliance. As the healthcare sector continues to evolve, the roles of health care clearinghouses as data exchange organizations will remain crucial for enhancing operational efficiencies and improving patient care outcomes, particularly regarding Medicare treatment approvals and provider interventions.
Explain How Healthcare Clearinghouses Operate in Claims Processing
Health care clearinghouses are pivotal in the processing ecosystem, as they receive requests from healthcare providers, validate information, and transmit documents to the appropriate payers. The process encompasses several essential steps:
- Claims Submission: Providers electronically send requests to the intermediary, initiating the processing workflow.
- Claims Scrubbing: The processing center meticulously examines each submission for errors, ensuring all required details are present and properly arranged. This step is crucial, as it significantly reduces average error rates in submissions, which can reach as high as 30% before utilizing clearinghouses.
- Eligibility Verification: Prior to submitting requests to payers, the intermediary verifies patient insurance coverage and eligibility. This proactive measure mitigates the likelihood of costly denials for providers.
- Transmission to Payers: Once validated, the health care clearinghouse transmits the submissions to the respective insurance companies in the required format, ensuring compliance with payer specifications.
- Tracking and Reporting: Many clearinghouses offer tracking services, enabling providers to monitor the status of their requests and obtain comprehensive reports on submission outcomes. This transparency is vital, as 61% of organizations assess ROI based on the time invested in appealing or submitting requests, while 52% evaluate the time spent appealing in relation to reimbursement totals.
This operational framework not only accelerates the request process but also substantially decreases the likelihood of errors that can lead to payment delays. Recent advancements in medical clearinghouse technology indicate that organizations enhancing their processing systems can achieve improved operational efficiency and revenue recovery. Indeed, over 75% of companies are considering replacements for current solutions if enhanced ROI can be demonstrated. As Jessica Glenn, Senior Product Owner, notes, “Prompt resubmission of denied requests guarantees that providers obtain payment for services rendered in a timely manner.” By optimizing the processing workflow, medical clearinghouses bolster the overall financial health of providers. Furthermore, services like MBI Lookup and retroactive clearinghouse offerings from firms such as ZOLL AR Boost exemplify the competitive landscape and the range of services available within the clearinghouse sector. The proactive measures taken by medical organizations in response to denial issues, as highlighted in the case study ‘Medical Organizations’ Response to Denial Issues,’ further underscore the importance of effective processing in mitigating financial repercussions.
![]()
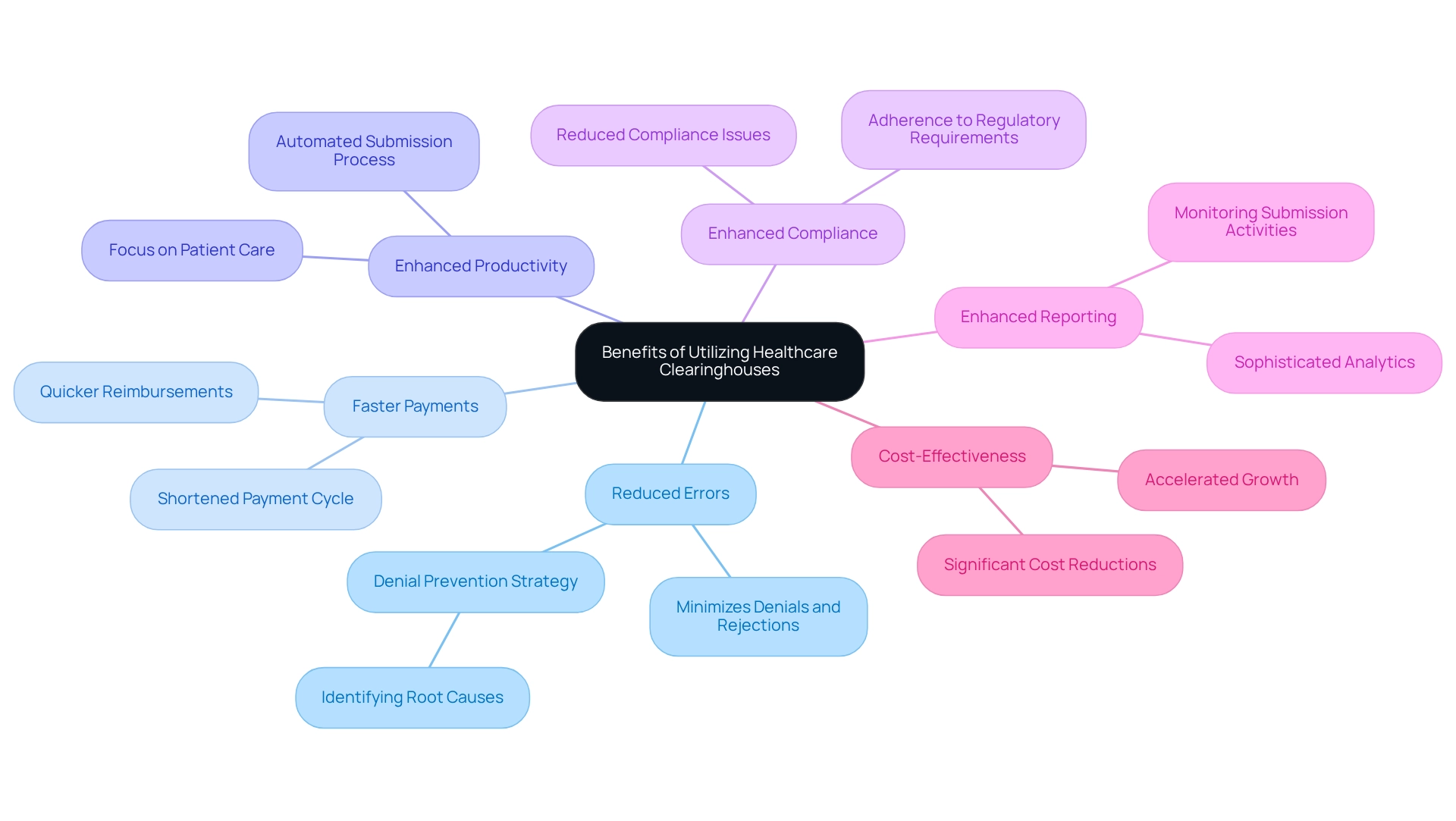
Outline the Benefits of Utilizing Healthcare Clearinghouses
Utilizing a health care clearinghouse offers numerous benefits that significantly enhance operational efficiency and financial performance for healthcare providers.
-
Reduced Errors: Clearinghouses meticulously scrub claims for inaccuracies prior to submission, effectively minimizing the risk of denials and rejections. As noted by eMEDIX Reimbursement Solutions, “Healthcare intermediaries can support your ability to accomplish this task by identifying the root causes of your denials and can create a denial prevention strategy for the future.” This proactive approach is crucial in maintaining a smooth revenue cycle.
-
Faster Payments: The efficient processing capabilities of financial intermediaries lead to quicker reimbursements from payers, which is essential for enhancing cash flow. Submissions handled through intermediaries typically experience an average time to payment that is considerably shorter than those sent directly, often shortening the payment cycle by several days.
-
Enhanced Productivity: By automating the submission process, intermediaries reduce administrative loads, enabling healthcare personnel to focus on patient care instead of documentation. This shift not only enhances productivity but also improves overall patient satisfaction.
-
Enhanced compliance is achieved as health care clearinghouses ensure that submissions adhere to regulatory requirements, thereby reducing the risk of compliance issues that can lead to costly penalties and delays in payment.
-
Enhanced Reporting: Numerous intermediaries provide sophisticated analytics and reporting resources, allowing providers to monitor submission activities and recognize patterns in billing practices. This data-driven insight is invaluable for optimizing revenue cycle management.
-
Cost-Effectiveness: By reducing the time and resources dedicated to claims management, processing centers can lead to significant cost reductions for medical organizations. This financial efficiency is particularly beneficial in an environment where the cost of care can be high and reimbursements may not always cover expenses. Effective use of intermediaries can accelerate growth and enhance patient flow, emphasizing the significance of customer relationships and adaptability.
In 2025, the effect of medical clearing organizations on payment speed and accuracy remains a focal point for analysts, who highlight their role in improving the financial well-being of practices. Real-world examples illustrate that organizations utilizing a health care clearinghouse encounter quicker payments and lower error rates, underscoring the health care clearinghouse’s significance in the contemporary medical environment.
Guide on Selecting the Right Healthcare Clearinghouse for Your Needs
When selecting a health care clearinghouse, it is essential to consider several key factors to ensure optimal claims processing and compliance.
- Reputation and Experience: Investigate the organization’s history and client feedback to assess its reliability and effectiveness in the industry. Understanding the reputation of a health care clearinghouse can significantly impact your operational success.
- Services Offered: Confirm that the organization provides essential services such as submission refinement, eligibility verification, and extensive reporting features customized to your requirements. For instance, CareSet combines over 100 external data sources for its analysis, highlighting the importance of strong data integration in processing. This capability can enhance your operational efficiency and decision-making processes.
- Compliance and Security: Ensure the organization adheres to HIPAA regulations and implements robust security measures to safeguard patient data. As Marc Haskelson, President and CEO, emphasizes, “Customers must be able to adapt their cybersecurity policies to apply to an array of threats. Cybersecurity is an ongoing issue that should be monitored closely…” This underscores the critical nature of adherence to security standards in today’s regulatory environment.
- Customer Support: Choose an organization that provides responsive and knowledgeable customer service to tackle any problems that may occur during the claims process, thus improving operational efficiency. A strong support system can make a significant difference in navigating challenges effectively.
- Cost Structure: Analyze the pricing model to ensure it fits within your budget while delivering value for the services provided, as average costs for healthcare clearinghouses in 2025 are projected to vary significantly based on service offerings. Understanding the financial implications is crucial for sustainable operations.
- Integration Capabilities: Evaluate whether the platform can seamlessly connect with your current billing systems, which is essential for streamlining operations and enhancing overall financial performance. A well-integrated system can lead to improved accuracy and efficiency in claims processing.
Additionally, consider the significance of preparedness in choosing a settlement organization. As illustrated by Dan Erwin, Security Officer at Dow Chemical Co., a significant incident can serve as a wake-up call for management regarding the importance of disaster planning. By thoughtfully evaluating these factors, healthcare providers can select a health care clearinghouse that not only enhances claims processing efficiency but also supports compliance and security, ultimately contributing to better patient care outcomes.

Conclusion
The role of healthcare clearinghouses in the claims processing landscape is undeniably critical. As intermediaries, they ensure the accurate transmission of claims between providers and payers, streamlining the entire billing process. The meticulous steps involved in claims submission, scrubbing, eligibility verification, and tracking significantly reduce errors and enhance operational efficiency, ultimately leading to faster payments and improved cash flow for healthcare providers.
Utilizing a healthcare clearinghouse offers a multitude of benefits, such as:
- Reduced error rates
- Increased efficiency
- Enhanced compliance
- Valuable reporting capabilities
These advantages foster a smoother revenue cycle and allow healthcare staff to concentrate more on patient care rather than administrative tasks. As the healthcare landscape evolves, the importance of clearinghouses in managing the complexities of claims processing and regulatory compliance cannot be overstated.
When selecting the right clearinghouse, it is essential for healthcare providers to evaluate factors such as:
- Reputation
- Services offered
- Compliance with security standards
- Customer support
- Cost structures
- Integration capabilities
A thoughtful approach to this selection process will pave the way for optimized claims processing and contribute to improved patient care outcomes. In an era where financial health is paramount, leveraging the strengths of healthcare clearinghouses is a strategic move that can yield significant benefits for providers and their patients alike.


