Overview
Diagnosis-Related Groups (DRGs) represent a pivotal classification system within healthcare, categorizing hospitalization costs and determining reimbursement for services. This system plays a significant role in the financial management and quality of care in medical facilities.
DRGs not only promote efficient resource utilization and standardized payments but also present challenges, including coding errors and potential compromises in patient care quality. Therefore, it is essential to ensure careful oversight as this system continues to evolve.
Introduction
In the complex realm of healthcare financing, Diagnosis-Related Groups (DRGs) stand as a pivotal mechanism for categorizing hospital costs and streamlining reimbursement processes. Developed in the late 1960s and mandated by Congress in the early 1980s, this classification system has undergone significant evolution, adapting to the ever-changing landscape of patient care and resource management. By grouping patients with similar clinical conditions, DRGs not only enhance operational efficiency for hospitals but also play a crucial role in influencing the quality of care delivered.
As the healthcare industry grapples with the challenges of cost control and transparency, understanding the multifaceted implications of DRGs becomes essential for stakeholders. This understanding is vital for navigating the intricacies of patient treatment pathways and reimbursement strategies.
Define Diagnosis-Related Group (DRG)
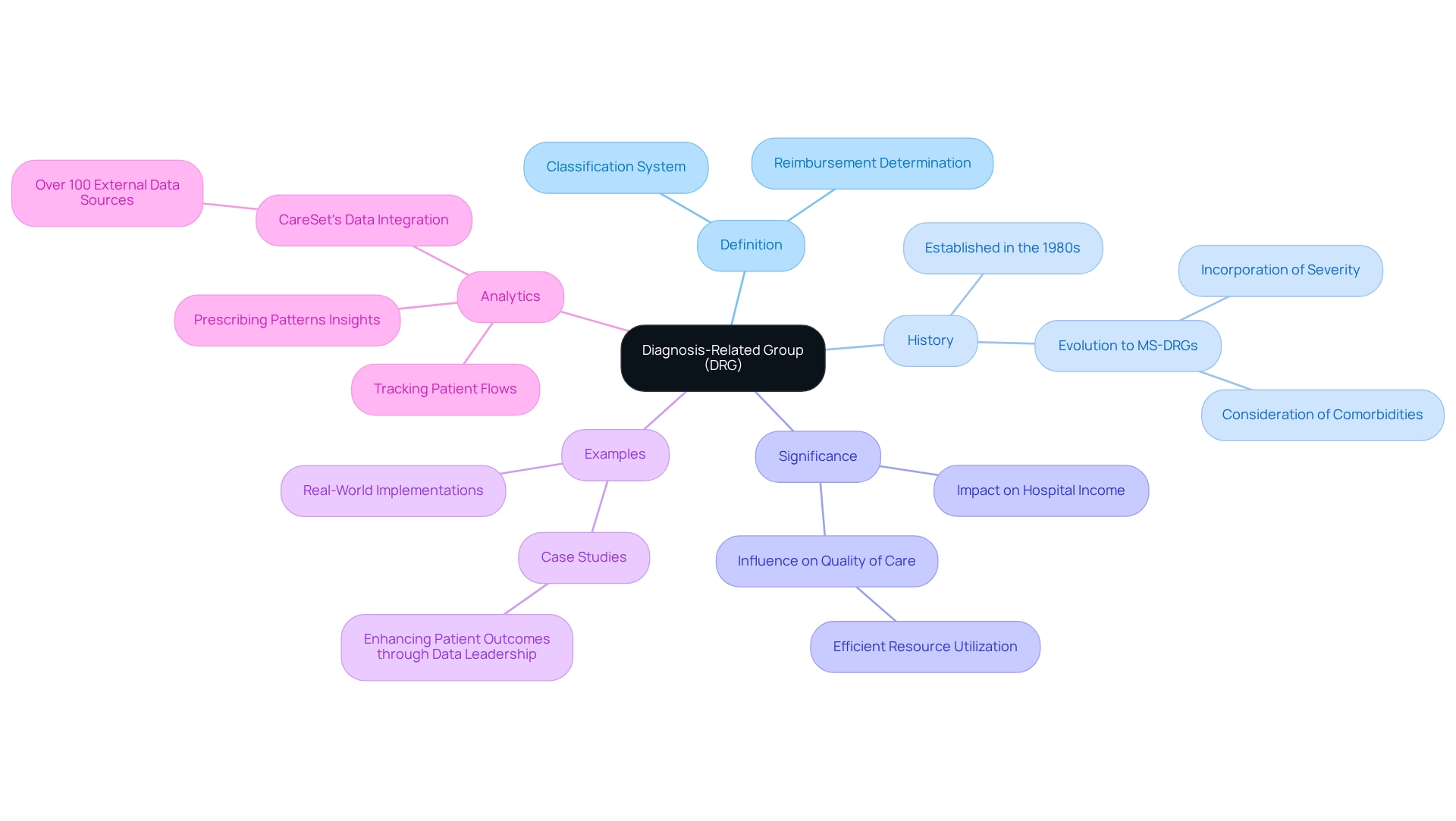
A Diagnosis-Related Group (DRG in healthcare) represents a vital classification system that categorizes hospitalization costs and determines reimbursement amounts from Medicare and other health insurance providers. Each DRG corresponds to specific diagnoses and treatments, grouping individuals with similar clinical conditions and resource needs. Established in the early 1980s, the DRG in healthcare system was initially designed to manage medical expenses by standardizing payments based on anticipated resource usage for various diagnoses. Over time, it has evolved to include subcategories such as Medicare Severity Diagnosis Related Groups (MS-DRGs), which take into account the severity of patients’ conditions and comorbidities, thereby improving the accuracy of the reimbursement process.
As of 2025, the importance of DRG in healthcare remains significant, with numerous medical facilities adopting this classification system to enhance their billing processes. Current statistics reveal that a majority of healthcare facilities utilize DRG in healthcare classifications, underscoring their essential role in reimbursement strategies. Experts in medical economics emphasize that the DRG in healthcare not only impacts hospital income but also influences the quality of care by promoting efficient resource utilization. Real-world examples demonstrate that facilities implementing DRG in healthcare systems have seen improvements in financial performance and patient outcomes, illustrating the system’s effectiveness in the evolving medical landscape.
At CareSet, we leverage our extensive Medicare data analytics to address critical healthcare questions related to diagnosis-related groups, such as understanding provider networks and treatment pathways. Our analytics track patient flows and prescribing patterns, offering insights that directly affect patient care and decision-making processes. According to Ty J. Gluckman, MD, ‘Most CMS quality and cost measures use a broader array of International Classification of Diseases, Ninth Revision and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision diagnosis codes for both identification and risk adjustment,’ highlighting the broader implications of DRG in healthcare on medical facility reimbursement. Moreover, the costs associated with diagnosis-related groups reflect actual expenses incurred in medical services and are adjusted for inflation, providing a more accurate financial overview for providers.
Explore the Role of DRGs in Healthcare Management
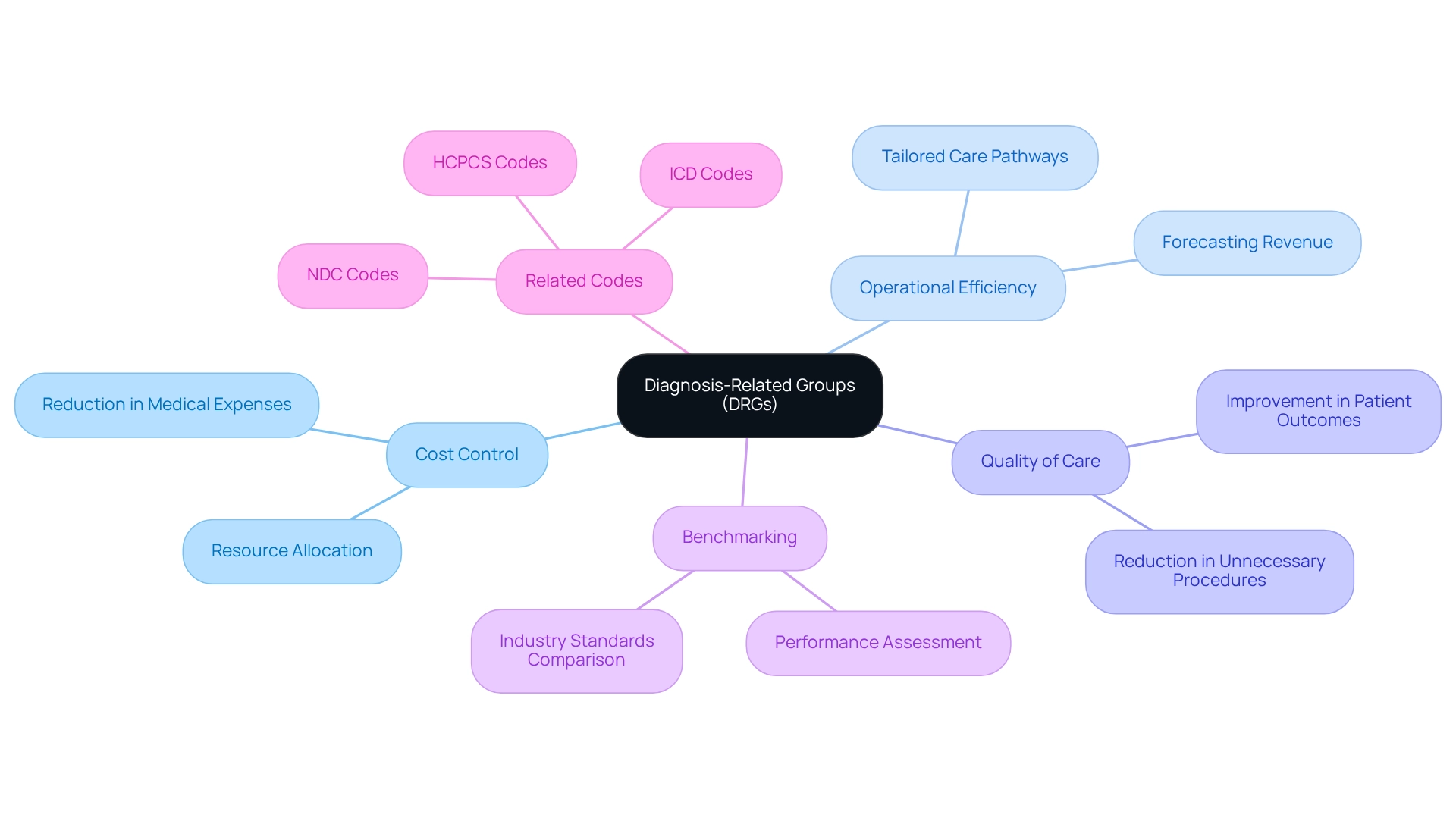
Diagnosis-Related Groups (DRGs in healthcare) play a crucial role in management, offering a systematic approach for facilities to control expenses and enhance operational efficiency. By categorizing patients based on their conditions and anticipated treatment costs, medical facilities can accurately forecast revenue and allocate resources effectively. This framework not only motivates healthcare providers to refine their operations but also leads to a reduction in unnecessary procedures and an improvement in the quality of care delivered to patients.
For example, hospitals often adopt tailored care pathways linked to specific diagnosis-related groups, optimizing treatment processes and improving patient outcomes. Furthermore, DRGs enable benchmarking and performance assessment, allowing providers to evaluate their efficiency and effectiveness against established industry standards.
As the landscape of healthcare management continues to evolve, the strategic utilization of DRGs in healthcare remains a pivotal trend, underscoring their significance in enhancing healthcare delivery and resource allocation. Understanding the interplay between DRGs, ICD, NDC, and HCPCS codes is essential for navigating Medicare treatment pathways, as these frameworks assist providers in guiding patients from diagnosis through various lines of therapy, ultimately elevating patient care and treatment approvals.
Analyze Benefits and Drawbacks of DRG Implementation
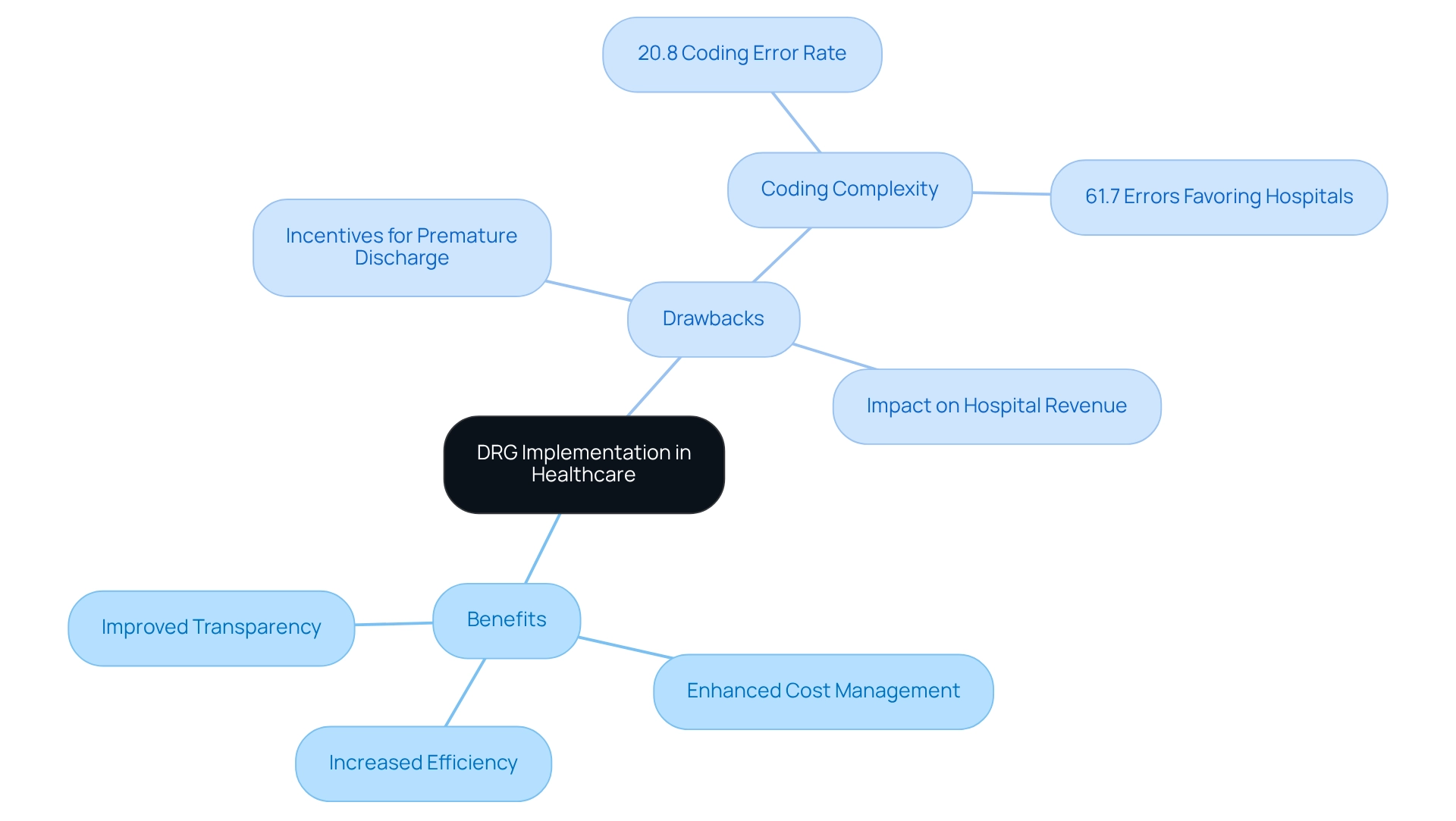
The application of DRG in healthcare presents numerous advantages, including increased efficiency, enhanced cost management, and improved transparency in medical billing practices. By standardizing payments, diagnosis-related groups (DRG in healthcare) significantly reduce variability in healthcare charges, encouraging providers to prioritize high-quality care while effectively managing expenses.
A notable study revealed that DRG coding errors occur at a rate of 20.8%, with 61.7% of these mistakes benefiting medical facilities, underscoring the critical importance of precise coding for equitable reimbursement.
However, the fixed payment structure associated with DRG in healthcare carries significant drawbacks. A primary concern is that it may incentivize medical facilities to discharge patients prematurely or avoid high-cost cases, potentially compromising the quality of care. Additionally, the complexity of accurately coding diagnoses can lead to inconsistencies in reimbursement, adversely affecting hospital revenue, particularly when considering the implications of DRG in healthcare.
Case studies, such as one examining medical expense variability and provider behavior in treating malignant tumors under the DRG payment system, illustrate how provider actions significantly influence cost disparities. This highlights the necessity for efficient management strategies to uphold service quality while controlling expenses.
As we approach 2025, the ongoing discourse surrounding DRG in healthcare emphasizes the need for tailored systems that reflect the economic and clinical realities of patients. While DRG in healthcare has undoubtedly transformed medical financing, it also presents challenges that necessitate vigilant oversight to ensure fair patient care and optimal outcomes.
Historical Context and Evolution of DRGs
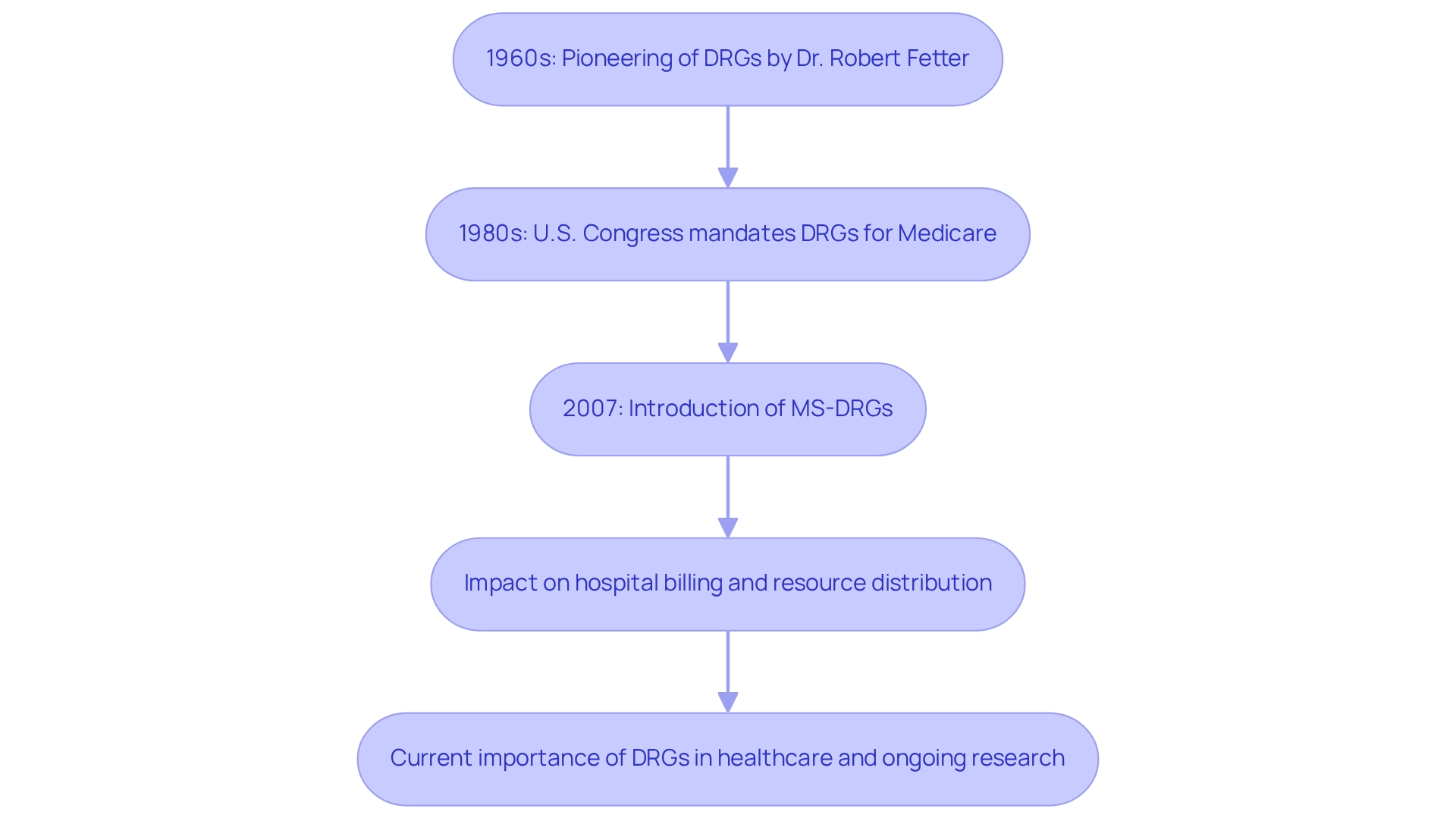
The concept of DRG in healthcare was pioneered in the late 1960s by Dr. Robert Fetter and his team at Yale University, designed specifically to categorize hospital cases for payment purposes. This system gained momentum in the early 1980s when the U.S. Congress mandated the use of DRGs in healthcare for Medicare reimbursement, a strategic move aimed at curbing escalating healthcare costs.
Since then, the DRG system has undergone significant changes, particularly with the introduction of Medicare Severity Diagnosis-Related Groups (MS-DRGs) in 2007, which consider the severity of individuals’ conditions. This evolution underscores a continuous commitment to improving reimbursement accuracy and enhancing the quality of patient care.
Currently, the DRG in healthcare is essential to medical financing in the United States, influencing comparable systems worldwide. Historical statistics indicate that the adoption of DRG in healthcare has greatly impacted hospital billing methods, resulting in enhanced cost management and resource distribution.
Furthermore, recent research emphasizes the necessity for robust monitoring systems to assess the effect of DRGs, ensuring that policy changes can be implemented to enhance medical outcomes. As the landscape of healthcare continues to evolve, ongoing research into DRG systems, including case studies from various countries, highlights the importance of adapting these frameworks to meet contemporary healthcare challenges.
Conclusion
The Diagnosis-Related Group (DRG) system is pivotal in the realm of healthcare financing, providing a structured approach to categorizing hospital costs and streamlining reimbursement processes. By grouping patients with similar diagnoses and treatment needs, DRGs enhance operational efficiency for healthcare providers while significantly influencing the quality of care delivered. As more hospitals adopt this classification system, the impact of DRGs on financial performance and patient outcomes becomes increasingly apparent.
While the advantages of DRGs encompass improved cost control and transparency, challenges persist. The fixed payment model can inadvertently incentivize premature discharges and may result in discrepancies in reimbursement due to coding errors. Thus, a careful balance must be maintained to ensure that implementing DRGs does not compromise the quality of patient care. Ongoing research and case studies are crucial for understanding these dynamics and refining the system for better outcomes.
In summary, the evolution of DRGs signifies a commitment to enhancing healthcare delivery while managing costs. As the healthcare industry continues to navigate its complexities, the strategic application of DRGs remains essential for optimizing resource management and improving patient care. Stakeholders must remain informed and actively participate in discussions surrounding DRGs to cultivate an environment that prioritizes both efficiency and patient well-being.


