Overview
The article examines how leading hospitals in North Carolina are revolutionizing patient care in 2025 through innovative practices, advanced technologies, and community-focused strategies. Noteworthy examples include:
- Duke University Hospital’s integration of genomics for personalized medicine
- UNC Health’s enhancements in technology aimed at improving patient experiences
- Atrium Health’s community wellness initiatives
These efforts collectively illustrate a comprehensive approach to enhancing healthcare outcomes across diverse patient needs, underscoring the importance of adapting to the evolving landscape of healthcare.
Introduction
In the evolving landscape of healthcare, several institutions are pioneering innovative approaches that redefine patient care and outcomes. Notably, Duke University Hospital is leading the way with groundbreaking treatment protocols in oncology and cardiology. Similarly, UNC Health has made significant strides by integrating technology to enhance patient experiences.
These organizations exemplify the transformative power of modern medicine. Furthermore, Atrium Health’s community-focused initiatives and Children’s Hospital of North Carolina’s advancements in pediatric care underscore a commitment to addressing diverse health needs.
Meanwhile, Mission Health’s emphasis on behavioral health and Caldwell Memorial Hospital’s integrated care model highlight the critical importance of comprehensive strategies in managing both physical and mental health. As these healthcare leaders harness data analytics and cutting-edge technologies, they are not only enhancing patient experiences but also setting new standards for excellence in care.
This article delves into the remarkable advancements made by these institutions, showcasing their dedication to innovation and their significant impact on the future of healthcare.
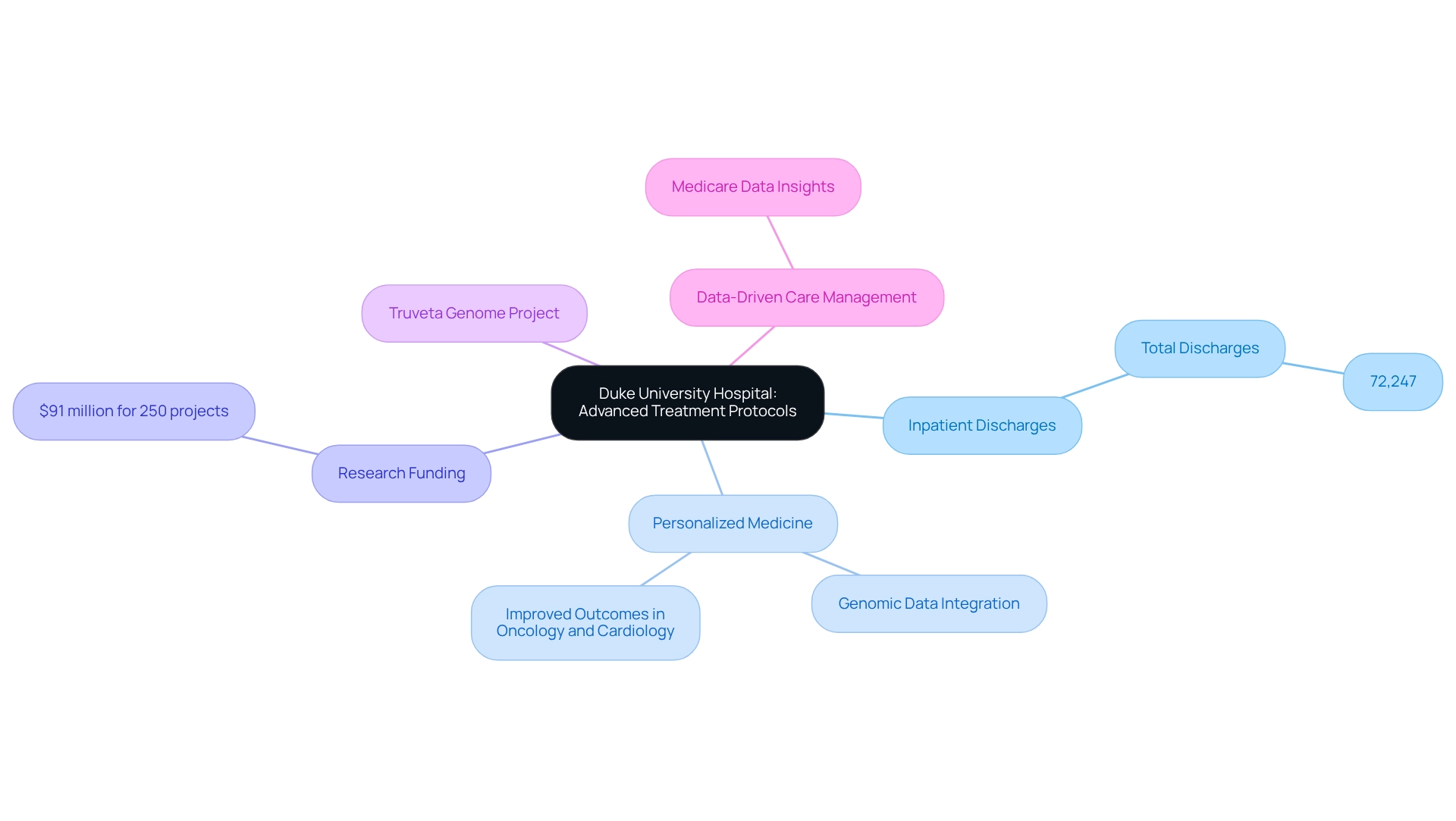
Duke University Hospital: Pioneering Advanced Treatment Protocols
Duke University Hospital stands at the forefront of medical innovation, pioneering advanced treatment protocols that harness cutting-edge research and technology. In FY24, the Duke University Health System reported a total of 72,247 inpatient discharges, underscoring its critical role in delivering healthcare to a vast population and highlighting its capacity to manage complex cases effectively. With a strong emphasis on personalized medicine and evidence-based practices, the hospital has achieved remarkable improvements in outcomes, particularly in oncology and cardiology.
The integration of genomic data into treatment plans has been transformative, enabling tailored therapies that enhance efficacy while minimizing side effects. This innovative method exemplifies Duke’s dedication to excellence in healthcare and serves as a benchmark for other institutions striving to elevate their standards. Current research efforts, including those supported by Duke faculty—amounting to over $91 million across 250 active projects—highlight the hospital’s commitment to enhancing global health and refining treatment protocols.
As part of its dedication to genomic advancements, Duke is engaged in the Truveta Genome Project, which aims to establish the world’s largest and most diverse database to uncover the science behind healthcare. This initiative further solidifies Duke’s leadership in personalized medicine, demonstrating the profound impact of genomic data on cancer treatment outcomes. Additionally, creative methods in managing stroke patients, such as circumventing unnecessary operations, illustrate Duke’s progressive strategies in care management.
Insights derived from Medicare data, as emphasized in recent case studies, improve provider involvement, especially concerning treatment alternatives like Qinlock for Gastrointestinal Stromal Tumor (GIST). CareSet’s data leadership plays a crucial role in this context, providing the necessary insights that empower medical providers to make informed decisions. This commitment to integrating advanced treatment protocols and leveraging data-driven insights positions Duke as a model for healthcare organizations aiming to enhance individual support and outcomes.
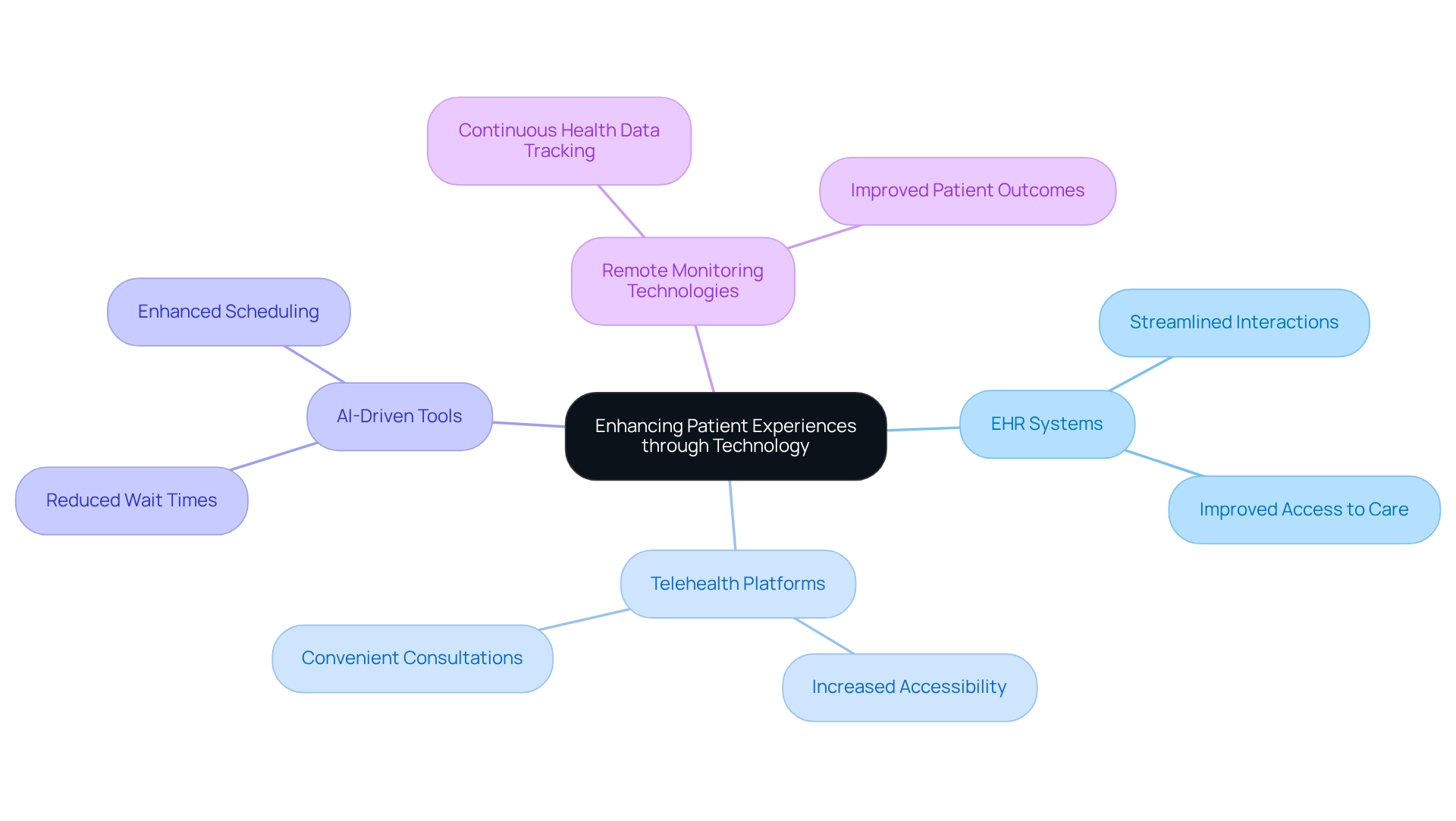
UNC Health: Integrating Technology for Enhanced Patient Experiences
UNC Health has made remarkable strides in harnessing technology to enhance the experiences of individuals receiving care. The implementation of advanced electronic health records (EHR) systems and telehealth platforms has streamlined interactions and improved access to care. Notably, the surge in venture capital interest in EHR startups, totaling $2.3 billion in 2023, underscores the growing investment and significance of EHR technologies within the medical field.
The integration of AI-driven tools for scheduling and follow-ups has significantly diminished wait times, leading to heightened satisfaction among individuals. For instance, the anticipated incorporation of remote monitoring technologies promises to further enhance outcomes through continuous health data tracking, reflecting a broader trend in medical technology. Additionally, initiatives like Abridge technology for clinical documentation enable healthcare providers to concentrate more on patient care rather than administrative duties, fostering a more care-centered approach.
This commitment to leveraging technology not only improves operational efficiency but also greatly enriches the overall experience for individuals receiving care. However, it is crucial to recognize the concerns raised by Steven Keating regarding patients’ access to their own medical data, illuminating the challenges that accompany these technological advancements. As Trishita Deb highlighted, this ongoing expansion signifies the increasing importance and adoption of eHealth technologies and solutions within the global healthcare landscape.
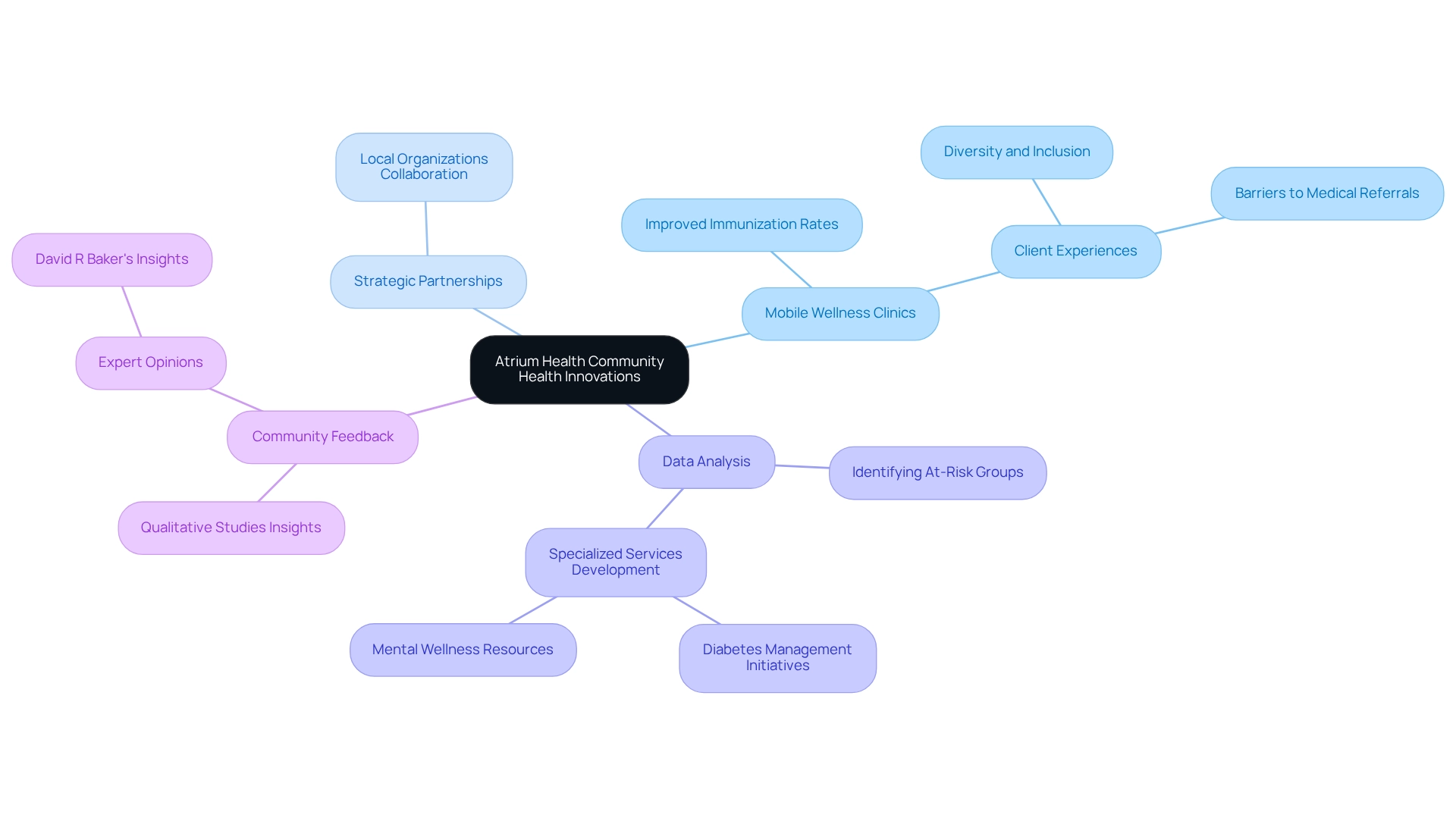
Atrium Health: Leading the Way in Community Health Innovations
Atrium Health distinguishes itself through its unwavering commitment to community wellness innovations aimed at reducing local wellbeing disparities. Their initiatives encompass mobile wellness clinics and strategic partnerships with local organizations, delivering preventive care and education tailored to community needs. By leveraging data analysis, Atrium Health effectively identifies at-risk groups, facilitating the development of specialized services such as diabetes management initiatives and mental wellness resources.
This proactive strategy not only enhances wellness outcomes but also fortifies community relationships and cultivates trust in the medical system.
Recent statistics reveal that mobile medical clinics have significantly improved immunization rates for influenza, pneumonia, and tetanus among participants in rural wellness projects, underscoring the effectiveness of these initiatives. Furthermore, qualitative studies illuminate the experiences of clients utilizing mobile medical clinics, emphasizing the importance of diversity and inclusion in service delivery. For instance, a study focused on a mobile community wellness clinic serving sexual and gender minorities in rural South Carolina identified substantial barriers to medical referrals, including lack of awareness and accessibility, while also highlighting opportunities for enhancing service provision to marginalized groups.
Atrium Health’s commitment to addressing inequalities is further evidenced by expert opinions, including David R Baker’s assertion that this service delivery model can mitigate disparities by improving access to essential services, particularly for communities at risk of medical issues. This comprehensive approach not only addresses immediate healthcare needs but also promotes long-term enhancements in community health, positioning Atrium Health as a leader in innovative healthcare solutions.
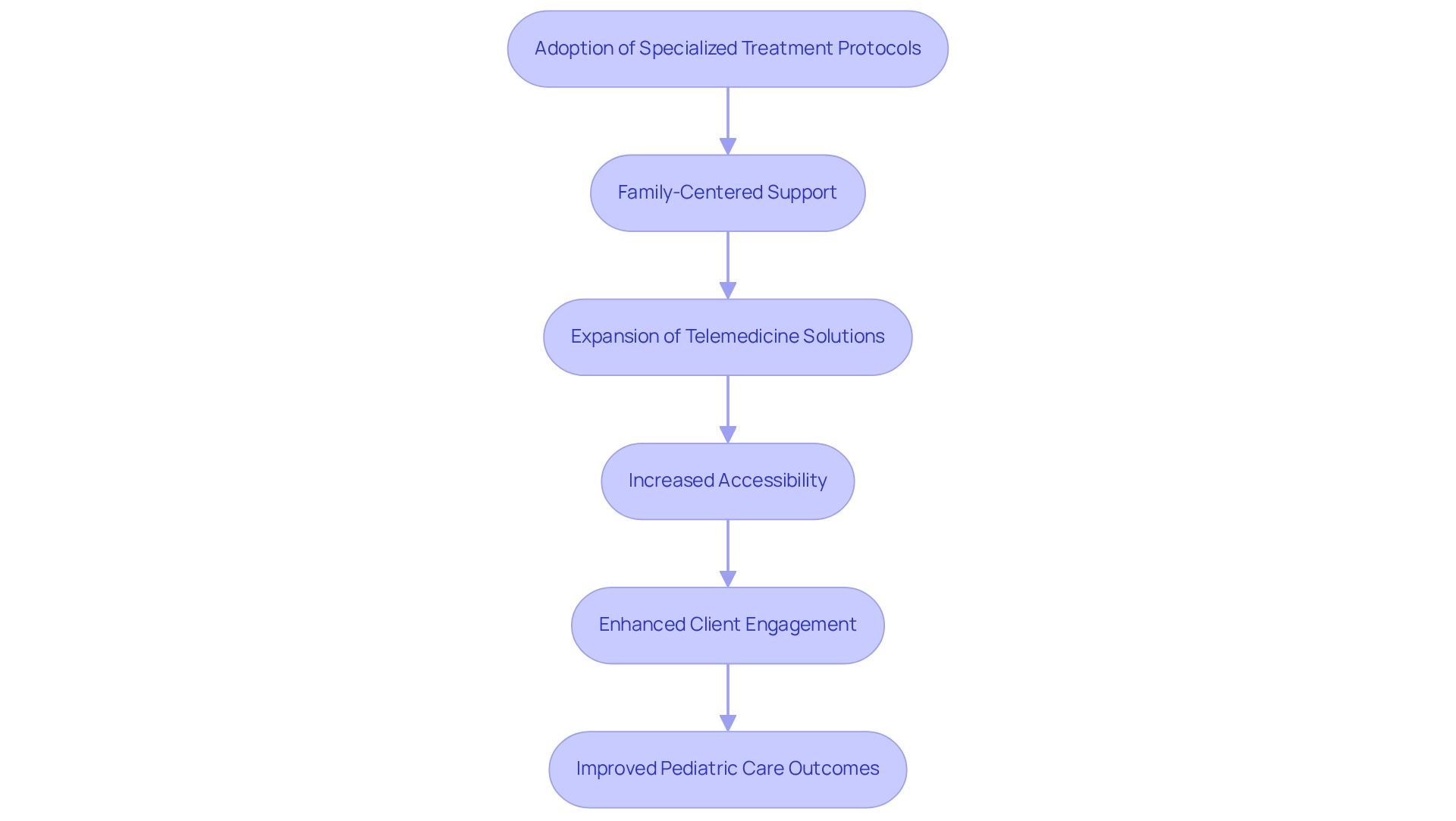
Children’s Hospital of North Carolina: Revolutionizing Pediatric Care
Hospitals in North Carolina, particularly the Children’s Hospital of North Carolina, are at the forefront of transforming pediatric services through the adoption of specialized treatment protocols and advanced technologies designed specifically for children. Their commitment to family-focused support actively involves both patients and their families in the healing process, fostering a nurturing environment that enhances recovery and wellness. In 2025, the hospital significantly expanded its telemedicine solutions, facilitating remote consultations that address the unique needs of young patients and their families.
This innovative approach not only improves accessibility but also ensures that children receive timely and appropriate care, irrespective of their geographical location. Notably, the hospital’s telemedicine initiatives have shown a remarkable increase in client engagement, with 91.7% of in-person follow-up visits occurring more than 24 hours after initial consultations, underscoring the effectiveness of their remote care strategies. As Steven Zauderer noted, the telehealth sector was valued at $49.9 billion in 2019, highlighting the growing importance of telemedicine in healthcare services.
Moreover, case studies reveal that telehealth provides enhanced access, efficiency, and cost savings, especially for patients in North Carolina hospitals or those in rural areas with limited mobility. Experts assert that such family-centered approaches in pediatrics lead to improved well-being, positioning the Children’s Hospital of North Carolina as a benchmark for future healthcare delivery.
Mission Health: Advancing Behavioral Health Services for Patients
Mission Health is at the forefront of enhancing behavioral wellness services, addressing the pressing need for mental well-being support within the community. Their comprehensive strategy prioritizes the integration of mental assessments into primary consultations, significantly improving access to essential outpatient services. By leveraging data analytics, Mission Health effectively tracks individual outcomes and identifies service gaps, facilitating the development of targeted programs that directly address prevalent mental wellness challenges, such as anxiety and depression.
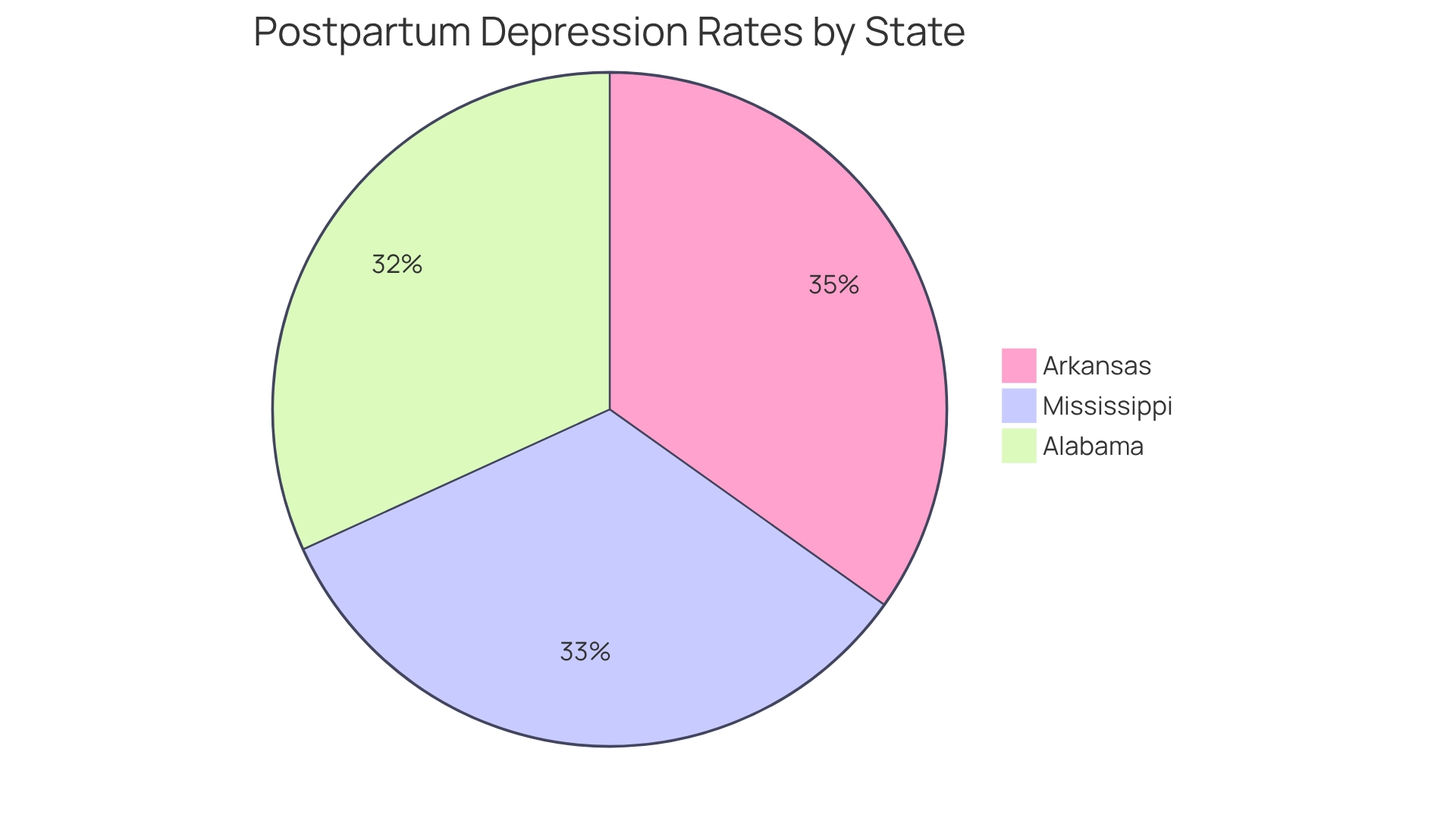
This holistic approach not only enhances individual outcomes but also plays a crucial role in reducing the stigma associated with mental health. Notably, by 2025, the implementation of mental wellness assessments has shown a marked positive impact on patient support. Data indicates that individuals with mental disorders face a 50% increased risk of diabetes and a 60% heightened risk of obesity. Additionally, postpartum depression rates are alarmingly above the national average in several rural states, with figures reaching:
- 21% in Alabama
- 22% in Mississippi
- 23% in Arkansas
This highlights the urgent need for intervention.
The WNC Healthy Impact Community Wellness Survey has provided invaluable insights into the community’s wellness needs, informing strategic planning for wellness initiatives. As Mission Health continues to refine its behavioral wellness services, the focus remains on fostering a supportive environment that prioritizes mental well-being and encourages individuals to seek the help they need. As one expert remarked, “Too many people go to jail or are involuntarily committed, which shows there are not services or current providers aren’t doing their job.”
This underscores the critical demand for improved mental wellness services in the region.
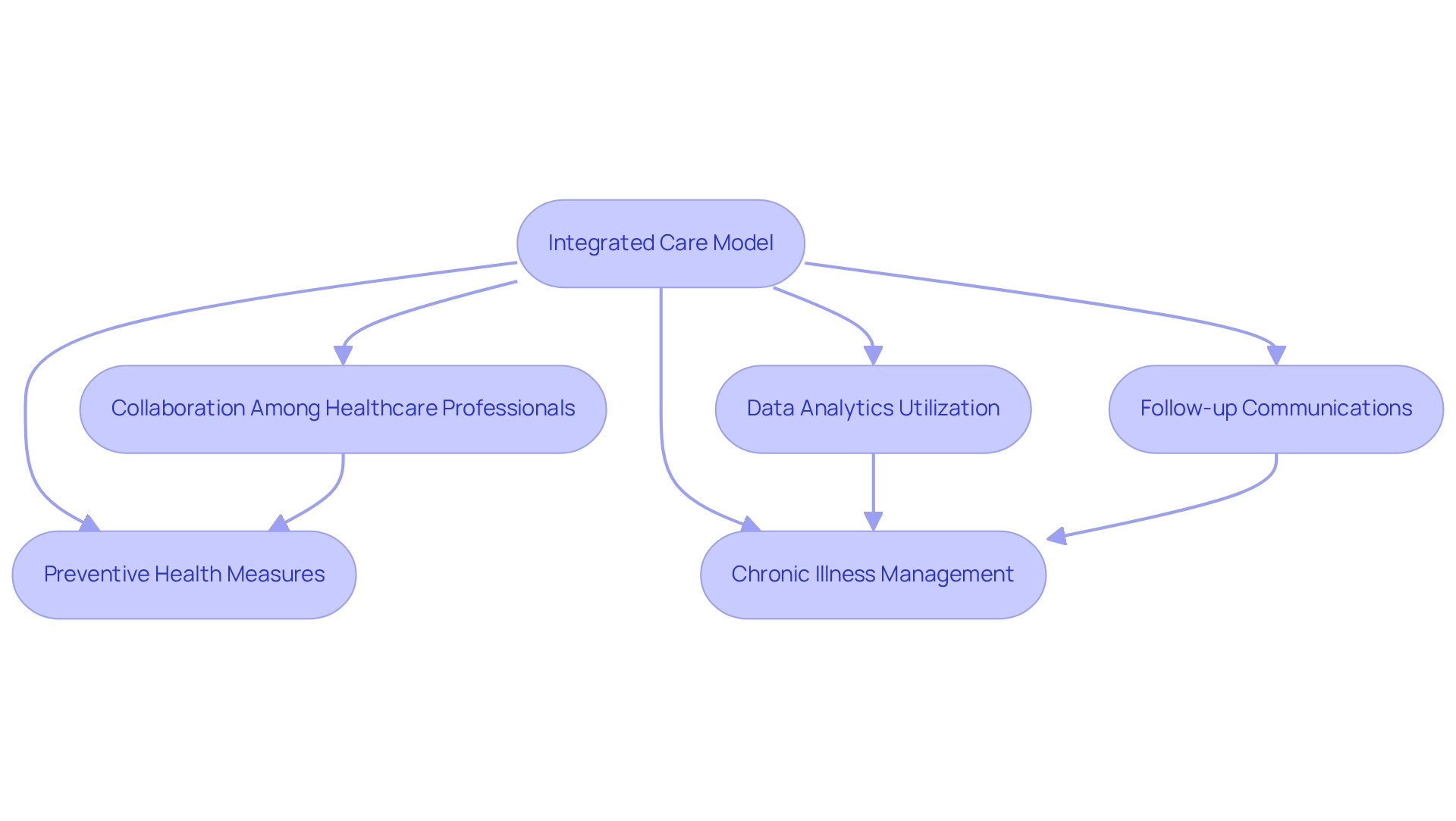
Caldwell Memorial Hospital: Comprehensive Care Through Integration
Caldwell Memorial Hospital exemplifies the advantages of a unified service model, offering a comprehensive range of services that cater to both physical and mental wellness needs. By fostering collaboration among diverse healthcare professionals, Caldwell ensures that individuals receive coordinated support tailored to their specific circumstances. This approach not only enhances preventive health measures but also significantly improves chronic illness management, resulting in better health outcomes and a notable reduction in hospital readmissions.
In 2025, Caldwell Memorial’s commitment to data analytics has proven essential in tracking individual progress, facilitating the continuous enhancement of treatment strategies. This proactive utilization of data, particularly insights derived from extensive Medicare claims data, allows the hospital to effectively adapt to the evolving needs of the community. For instance, research has shown that follow-up phone calls to individuals post-hospitalization can significantly boost compliance with treatment plans and address any emerging issues.
A specific case study highlighted that such follow-up calls markedly improved client engagement and decreased the likelihood of readmissions, underscoring the critical role of ongoing communication in care.
Furthermore, with approximately 1.4 million new cases of prostate cancer reported globally in 2020, the demand for effective chronic disease management is more pressing than ever. By leveraging insights from Medicare data, including NDC and HCPCS codes, Caldwell Memorial Hospital can gain a deeper understanding of treatment pathways and provider interventions, ensuring they meet urgent medical needs while promoting long-term health advancements. This illustrates the essential role of teamwork among medical providers in enhancing patient outcomes.
As Charles Darwin aptly noted, “It is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change,” emphasizing the necessity for adaptability in healthcare practices.
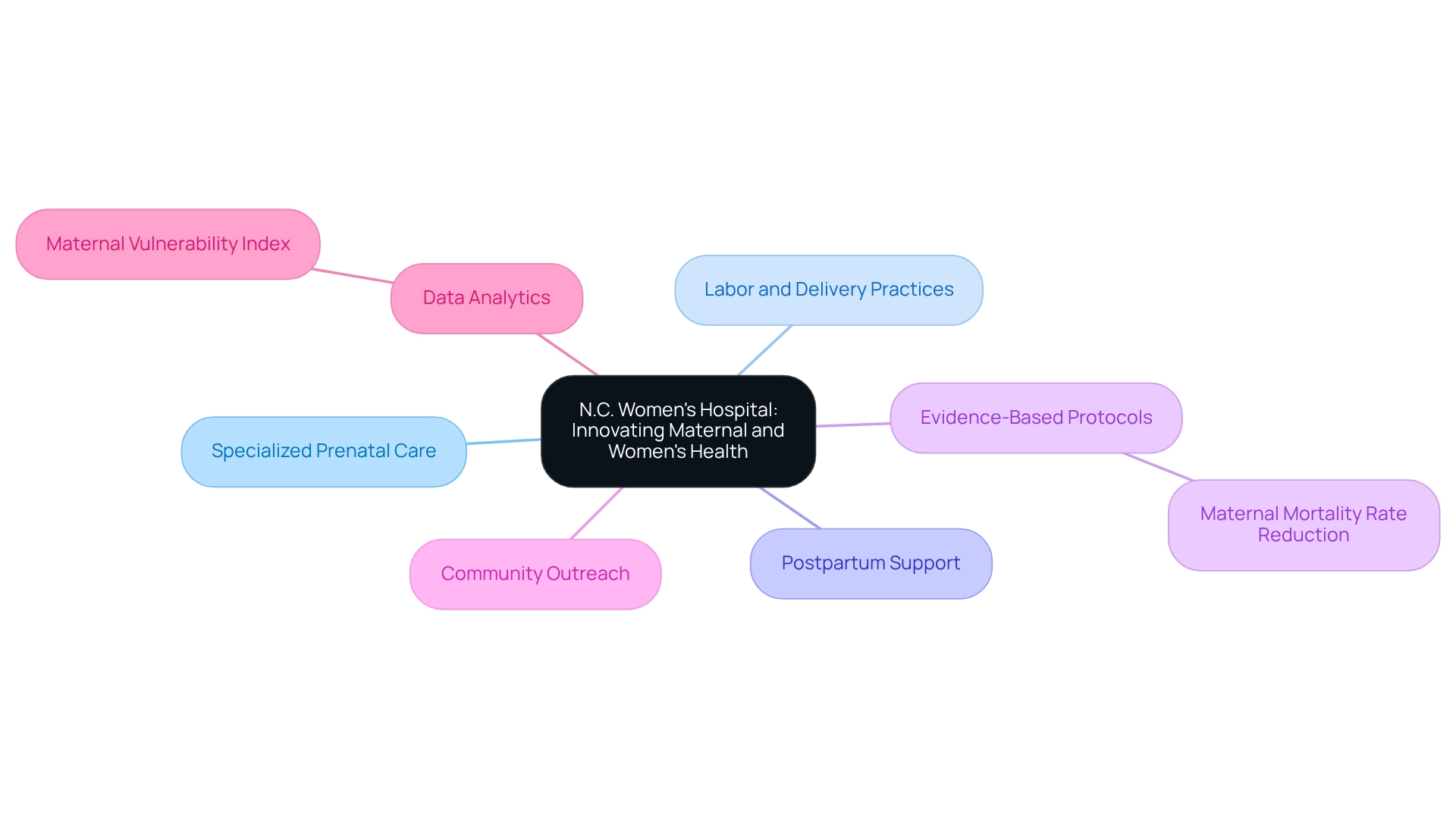
N.C. Women’s Hospital: Innovating Maternal and Women’s Health
Hospitals in North Carolina, such as N.C. Women’s Hospital, are at the forefront of transforming maternal and women’s wellness services through a comprehensive approach that emphasizes specialized prenatal care, advanced labor and delivery practices, and robust postpartum support. Evidence-based protocols have been adopted to enhance maternal safety, leading to significant improvements in outcomes for both mothers and infants. In 2025, statistics indicate that hospitals implementing these protocols have experienced a notable reduction in maternal mortality rates, aligning with the goals of the Healthy People 2030 initiative, which highlights the importance of decreasing maternal mortality as a key wellness indicator.
As the World Health Organization (WHO) asserts, “the majority of maternal deaths resulting from pregnancy-related complications are preventable.”
Moreover, hospitals in North Carolina, including N.C. Women’s Hospital, are dedicated to education and community outreach, ensuring that women have access to vital resources and support throughout their healthcare journeys. By utilizing data analytics, the hospital continuously evaluates and refines its services to meet the unique needs of women in the community. This commitment to innovation is further evidenced by recent advancements in prenatal support, recognized as essential for enhancing maternal well-being outcomes.
The Maternal Vulnerability Index (MVI) assigns a score of 0-100 to each geographic area, with a higher score indicating increased vulnerability to adverse maternal outcomes. By understanding the primary factors contributing to this vulnerability, N.C. Women’s Hospital actively implements targeted interventions to mitigate these risks. Consequently, N.C. Women’s Hospital not only excels in clinical outcomes but also cultivates a supportive environment that empowers women to take charge of their health.
AdventHealth: Utilizing Telehealth to Enhance Patient Access
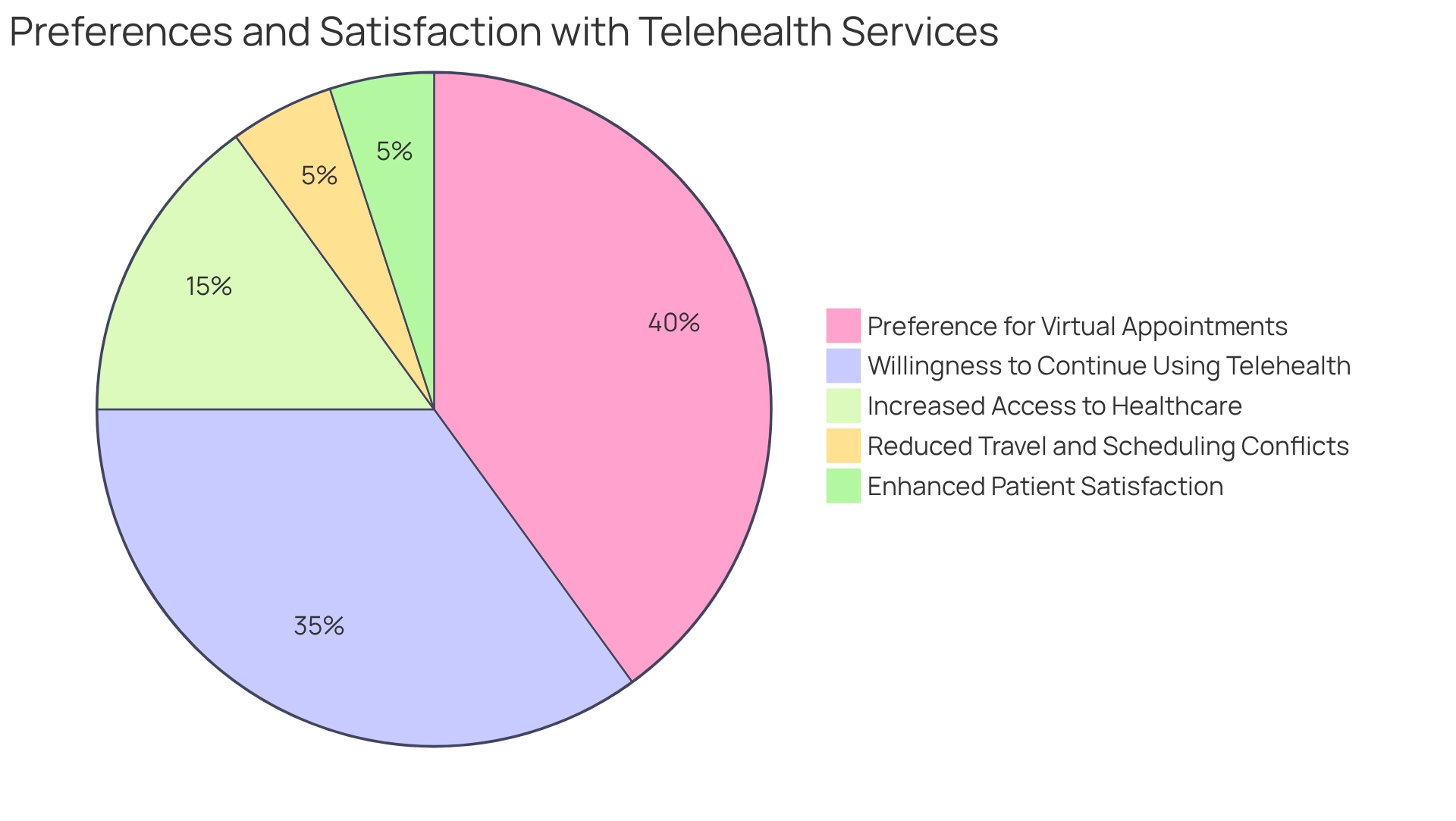
AdventHealth has strategically integrated telehealth into its care model, significantly enhancing access to medical services. By providing virtual consultations and remote monitoring, AdventHealth effectively eliminates common barriers such as travel and scheduling conflicts, ensuring timely medical care for patients. This platform addresses a diverse array of medical needs, ranging from routine check-ups to chronic illness management, thereby increasing overall patient satisfaction.
The benefits of this approach are particularly pronounced for individuals in rural and underserved regions, where access to healthcare can be limited. A recent analysis on patient satisfaction with telehealth services revealed that many users prefer virtual appointments over traditional in-person visits, highlighting a shift in service delivery preferences. Furthermore, a substantial proportion of patients expressed a willingness to continue utilizing telemedicine beyond the pandemic, underscoring its growing significance in modern healthcare.
AdventHealth’s commitment to telehealth not only broadens access for patients but also contributes to improved health outcomes, exemplifying a forward-thinking approach to healthcare delivery in 2025. By focusing on patient feedback and satisfaction, AdventHealth demonstrates the effectiveness of its telehealth services in meeting the evolving needs of its clientele.
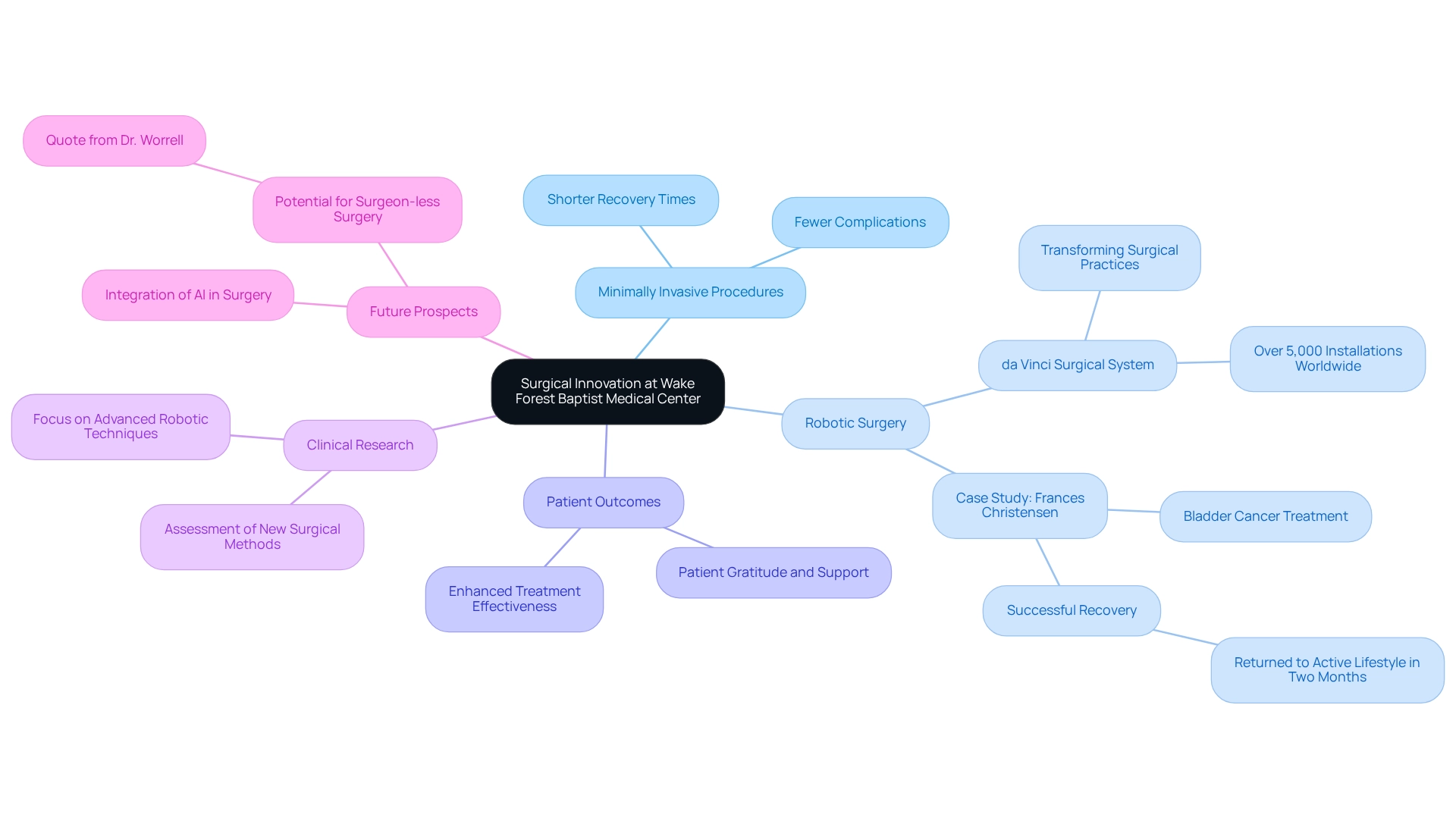
Wake Forest Baptist Medical Center: Innovating Surgical Care
Wake Forest Baptist Medical Center is at the forefront of surgical innovation, utilizing advanced techniques and technologies to significantly enhance patient care. Their commitment to minimally invasive procedures has led to shorter recovery times and fewer complications, greatly improving outcomes for individuals. The center’s adoption of robotic-assisted surgery exemplifies their dedication to precision; with over 5,000 installations of the da Vinci Surgical System worldwide, this technology is transforming surgical practices.
A notable case is that of Frances Christensen, a bladder cancer patient from Hertfordshire, who chose robotic surgery following chemotherapy. Under the expert guidance of Professor John Kelly, she successfully underwent the procedure and returned to her active lifestyle within two months. This case underscores the effectiveness of these innovative techniques and highlights the transformative potential of robotic-assisted surgery in enhancing treatment outcomes.
Wake Forest Baptist is also deeply engaged in clinical research, continuously assessing the effectiveness of new surgical methods, including advanced robotic techniques and minimally invasive approaches. This proactive strategy ensures they remain at the cutting edge of the field, providing the highest quality service to their patients. As Dr. Worrell noted, “The prospect of driverless cars makes it seem quite possible that we will one day see surgeon-less surgery,” reflecting the exciting future of surgical innovation.
Furthermore, as AI and new technologies continue to advance, the center is poised to further enhance the development and accessibility of surgical robotics, solidifying its role in transforming healthcare by 2025.
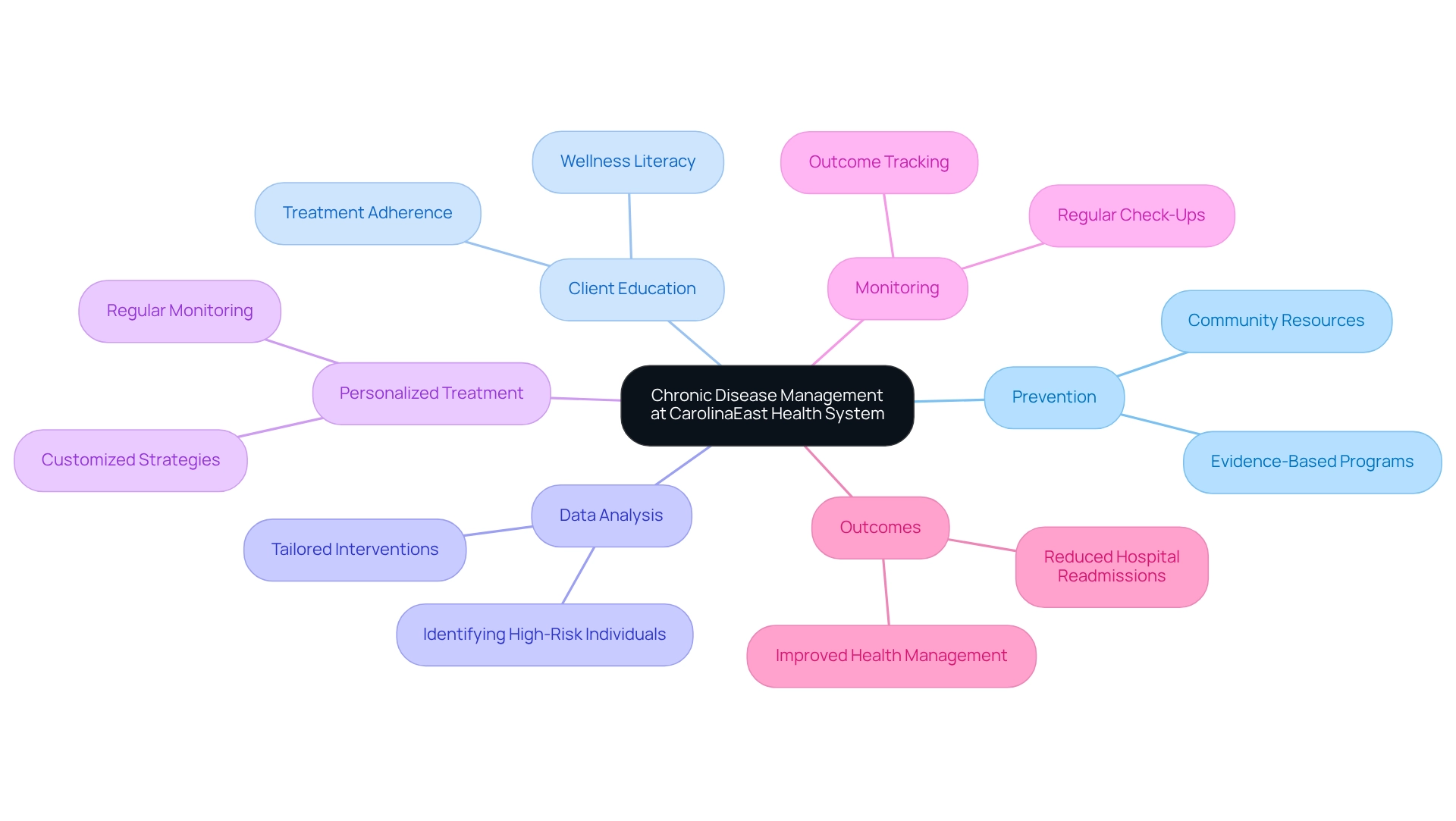
CarolinaEast Health System: Transforming Chronic Disease Management
CarolinaEast Health System is at the forefront of transforming chronic disease management through innovative programs centered on prevention and client education. By leveraging data analysis, the system adeptly identifies high-risk individuals, paving the way for targeted interventions tailored to the unique needs of those with chronic conditions such as diabetes and hypertension.
Their comprehensive care model encompasses regular monitoring, personalized treatment strategies, and access to community resources, all designed to empower individuals in managing their health. This proactive approach not only enhances outcomes for individuals but also enables them to take charge of their wellness.
In 2025, CarolinaEast’s commitment to chronic disease management is underscored by significant statistics: the adoption of evidence-based programs has led to a marked reduction in hospital readmissions in North Carolina among individuals with chronic conditions. An examination of 43 studies published from January 2018 to June 2024 reinforces these findings, highlighting the effectiveness of such programs in improving care for individuals.
Furthermore, expert insights emphasize that educational initiatives have been crucial in boosting wellness literacy, which is vital for the effective management of chronic illnesses. As highlighted in a recent report by Medscape Medical News, these findings can inform national wellness strategies and foster a shift towards integrated, patient-centered care models.
Innovations in consumer education at CarolinaEast have also yielded promising results, with studies indicating that informed individuals are more inclined to adhere to treatment plans and engage in preventive wellness behaviors. Consequently, the health system continues to set benchmarks in chronic disease management, illustrating the profound impact of education and data-driven strategies on health outcomes. This aligns with CareSet’s case study on ‘Long-Term Strategic Growth for Healthcare Partners,’ which demonstrates the broader implications of data-driven approaches on patient outcomes and strategic growth.
Conclusion
The advancements made by healthcare institutions such as Duke University Hospital, UNC Health, Atrium Health, and others showcase a significant shift towards innovative and patient-centered care. Each organization exemplifies a unique approach—whether through pioneering treatment protocols, integrating technology to enhance patient experiences, or addressing community health disparities. The commitment to utilizing data analytics and cutting-edge technologies highlights the transformative power of modern medicine in improving patient outcomes.
Duke University Hospital’s emphasis on personalized medicine and genomic data integration sets a benchmark for excellence in oncology and cardiology. Similarly, UNC Health’s investment in electronic health records and telehealth solutions underscores the importance of technology in streamlining patient interactions. Atrium Health’s community-focused initiatives demonstrate the impact of targeted programs in reducing health disparities, while Children’s Hospital of North Carolina illustrates the importance of family-centered care in pediatrics.
Moreover, Mission Health’s integration of behavioral health services and Caldwell Memorial Hospital’s comprehensive care model reflect the growing recognition of the interconnectedness of physical and mental health. As healthcare continues to evolve, the emphasis on innovative strategies and holistic approaches will be paramount in addressing the diverse needs of patients.
In conclusion, these institutions not only set new standards for healthcare excellence but also inspire a future where patient care is enhanced through collaboration, technology, and a deep understanding of community needs. The collective efforts of these leaders in healthcare pave the way for a more responsive and effective healthcare system, ultimately improving the health and well-being of the communities they serve.

