Overview
The article focuses on essential steps to master the 855A application process for healthcare providers seeking enrollment in federal healthcare programs. Notably, over 50% of applications are rejected due to missing documentation, underscoring the critical importance of meticulous preparation and accuracy in documentation.
Errors in this process can lead to significant delays or outright rejections, which can be detrimental to providers aiming to secure their place in federal healthcare initiatives. This statistic serves as a compelling call to action for providers to prioritize thoroughness in their applications.
Introduction
Navigating the complexities of the Medicare enrollment process presents a significant challenge for institutional providers. The CMS-855A Enrollment Application serves as a crucial gateway for healthcare facilities seeking to bill Medicare for their services. Given the heightened stakes, a comprehensive understanding of this application is vital to prevent costly delays or denials. In an increasingly competitive healthcare landscape, the ramifications of accurate enrollment extend beyond mere compliance; they can profoundly impact operational efficiency and patient care. This article explores the purpose of the CMS-855A application, outlines the necessary documentation, provides a step-by-step guide for completion, and addresses common pitfalls that applicants may encounter. By equipping providers with the knowledge to navigate this process effectively, the article aims to bolster their ability to serve Medicare beneficiaries with confidence and precision.
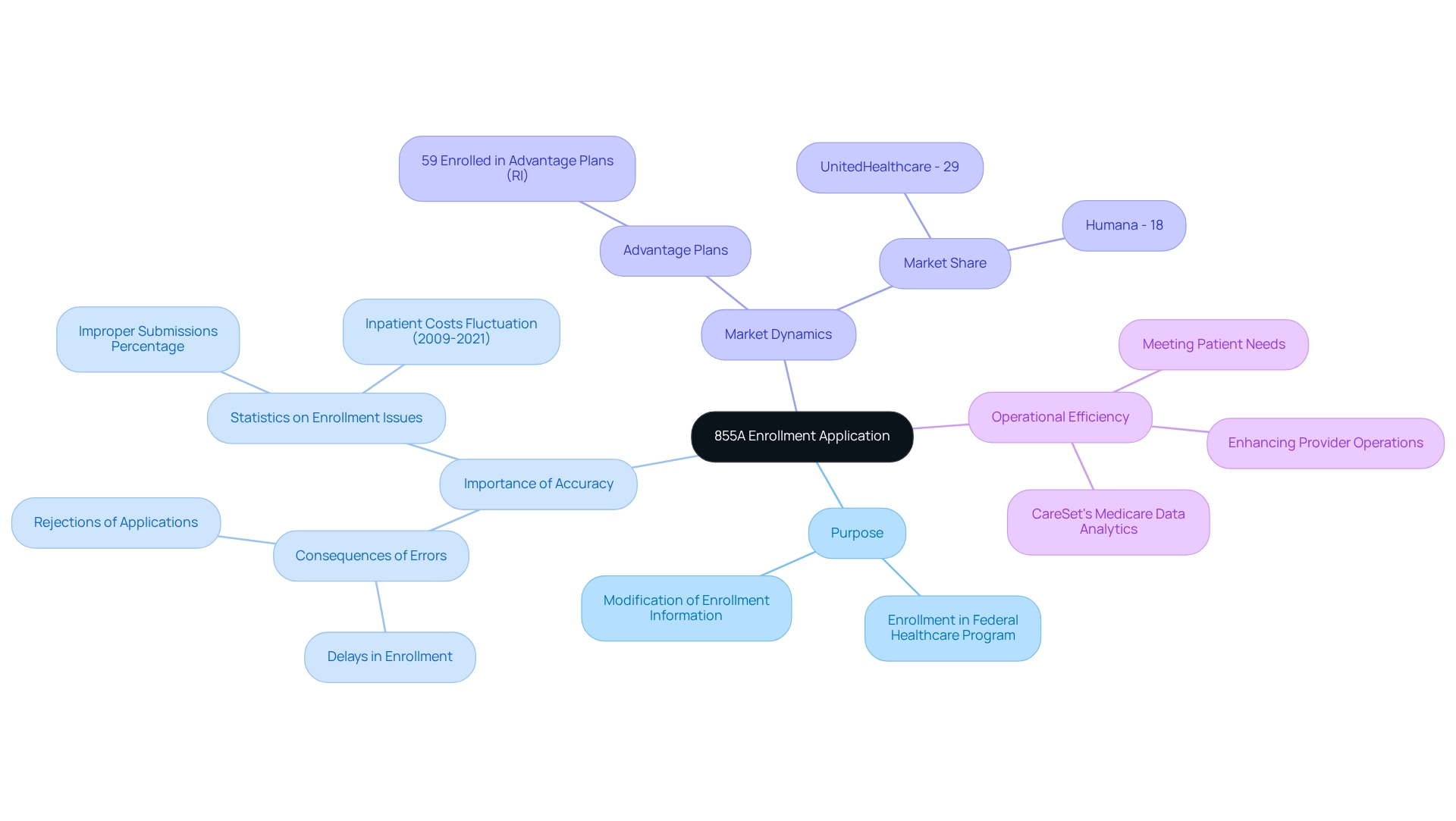
Understand the Purpose of the 855A Enrollment Application
The 855A Enrollment Application is a vital resource for institutional providers seeking to enroll in the federal healthcare program or modify their current enrollment information. This application is essential for healthcare facilities—such as hospitals, nursing homes, and rehabilitation centers—that intend to bill for the services they offer. A clear understanding of its purpose underscores the importance of precise and thorough entries, as mistakes can lead to significant delays or outright rejections in enrollment.
Precise entries are crucial; they ensure that providers comply with Medicare’s strict standards, enabling them to deliver essential services to patients under the program. Statistics reveal that improper submissions can result in a substantial percentage of enrollment issues, emphasizing the necessity for meticulous attention to detail. For instance, inpatient actual costs related to healthcare coverage as a percentage of total expenses have fluctuated from 2009 to 2021, underscoring the financial ramifications of accurate submissions.
Moreover, expert opinions highlight that the 855A request is not merely a bureaucratic procedure but a critical element that maintains the integrity of the healthcare system. Healthcare professionals consistently advocate for comprehensive preparation and understanding of the application process, as it directly impacts the ability of facilities to effectively assist beneficiaries.
As noted by Forbes Advisor, 59% of individuals enrolled in Rhode Island are part of a health insurance Advantage plan, illustrating the competitive landscape that healthcare providers must navigate. Additionally, the dominance of UnitedHealthcare and Humana in the Advantage market—accounting for 29% and 18% of the market share, respectively—further emphasizes the significance of accurate enrollment processes in a market dominated by a few key players.
By prioritizing precision in the 855A Enrollment Application, healthcare providers can enhance their operational efficiency and ensure they are well-prepared to meet the needs of their patients within the healthcare framework. Furthermore, CareSet’s advanced Medicare data analytics can offer critical insights into provider networks and treatment pathways, reinforcing the importance of accurate data submissions in the healthcare industry and ultimately enhancing patient care.
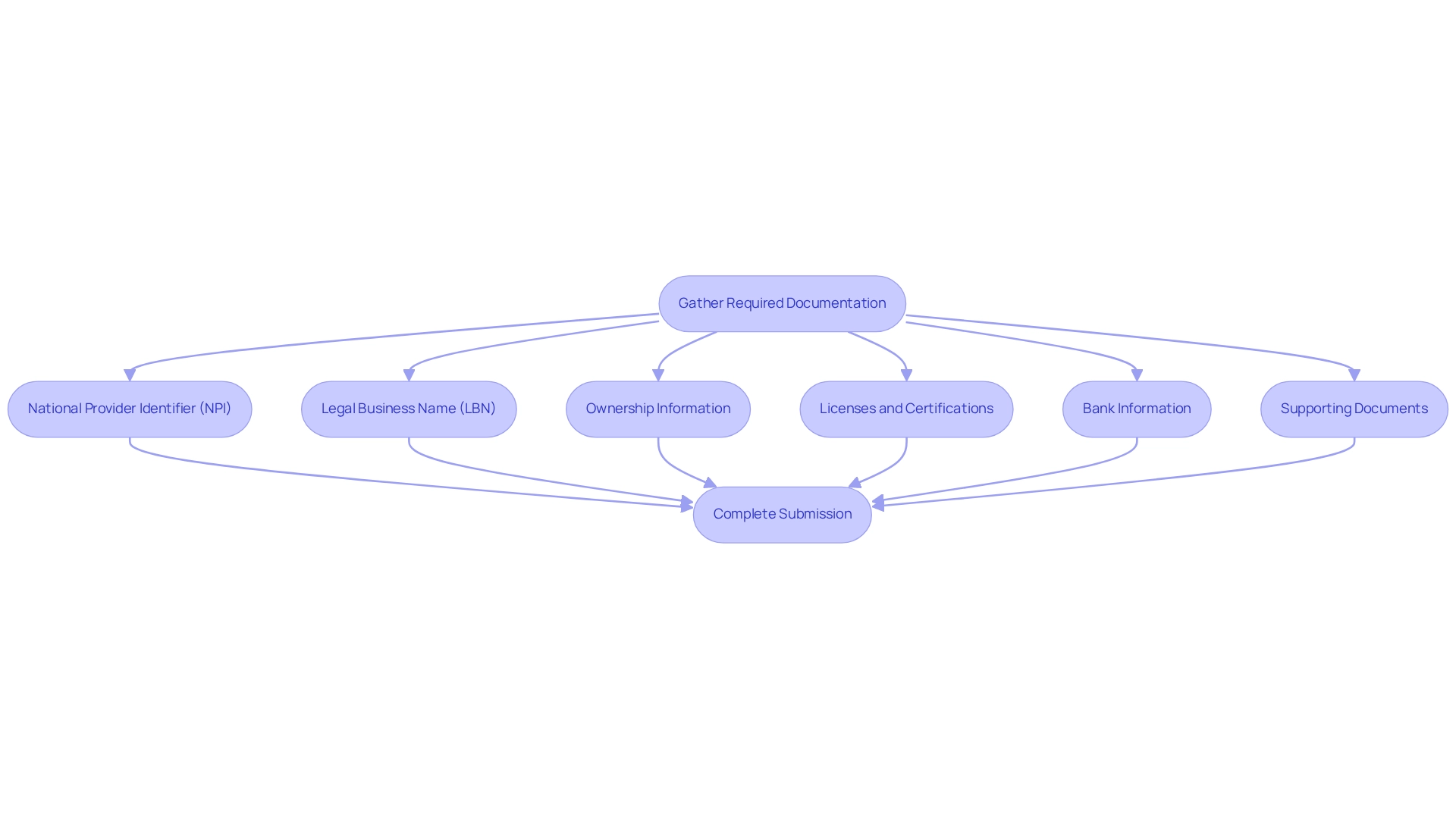
Gather Required Documentation and Information
Before initiating the 855a process, gathering all required documentation is essential to prevent delays and denials. The following items are crucial:
- National Provider Identifier (NPI): This identifier is mandatory for enrollment; ensure it is readily available.
- Legal Business Name (LBN): Obtain documentation from the IRS that verifies your LBN to confirm your business identity.
- Ownership Information: Provide detailed information about the ownership structure of your facility, including any controlling interests, to comply with regulatory requirements.
- Licenses and Certifications: Include copies of all relevant state licenses and certifications to demonstrate compliance with local regulations.
- Bank Information: Complete the CMS Form 588 to facilitate electronic funds transfer, ensuring that payment processes are streamlined.
- Supporting Documents: Depending on your specific provider type, additional documents may be required. Having these prepared will significantly improve the efficiency of your submission process.
Statistics indicate that over 50% of applications are rejected due to missing documentation, underscoring the importance of thorough preparation. Interacting with healthcare registration experts can offer crucial guidance on efficiently collecting the required documents. As Sheryl Xavier notes, “For further questions regarding these new SNF Medicare disclosure requirements please contact Sheryl Xavier.” This highlights the importance of seeking expert guidance. CareSet’s thorough strategy not only meets urgent data requirements but also promotes long-term strategic development for its partners, guaranteeing a more seamless journey to successful registration.
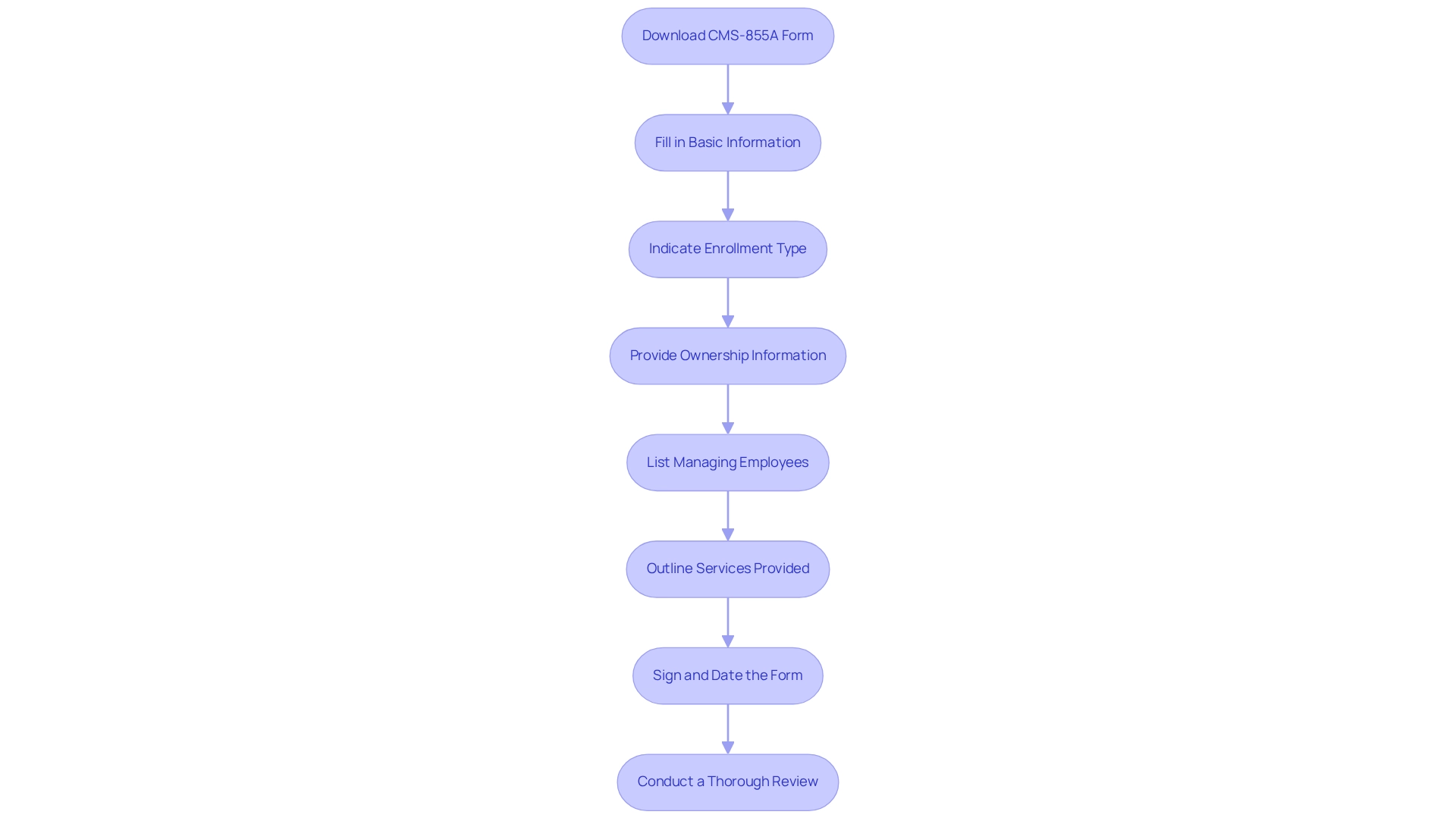
Complete the 855A Application Form Step-by-Step
To successfully complete the CMS-855A application form, adhere to the following steps:
- Access the 855A form by downloading the most recent version of the CMS-855A from the CMS website.
- Section 1: Basic Information: Accurately fill in your facility’s name, address, and National Provider Identifier (NPI). Ensure that all information aligns with your supporting documents.
- Section 2: Enrollment Type: Indicate whether this request is for new enrollment or a modification of existing information.
- Section 3: Ownership Information: Provide comprehensive details about the ownership structure, including the names and addresses of all owners.
- Section 4: Managing Employees: List key personnel along with their respective roles within the organization.
- Section 5: Services Provided: Clearly outline the types of services your facility will offer under Medicare.
- Section 6: Certification: Sign and date the form, ensuring that the signature of the authorized official is included.
- Review: Conduct a thorough review of all entries for accuracy and completeness prior to submission. Incomplete or incorrect information can lead to significant delays, as skilled nursing facility (SNF) providers are required to respond to revalidation requests from CMS within 90 days. Frequent mistakes in 855A submissions can result in rejections, underscoring the necessity for careful attention to detail.
Additionally, many applicants overlook critical details that can hinder their approval process, as noted by David J. Vernon, a partner specializing in Medicare and Medicaid reimbursement. With CMS dispatching notifications to all SNFs demanding they submit revalidation forms with updated information, the urgency of completing the form correctly cannot be overstated. Legal guidance is also recommended, as highlighted in the case study “Legal Considerations for SNFs Under New Regulations,” which discusses the importance of compliance with the new reporting requirements.
By diligently following these steps, you can enhance the likelihood of a successful submission and avoid common pitfalls that may arise during the process.
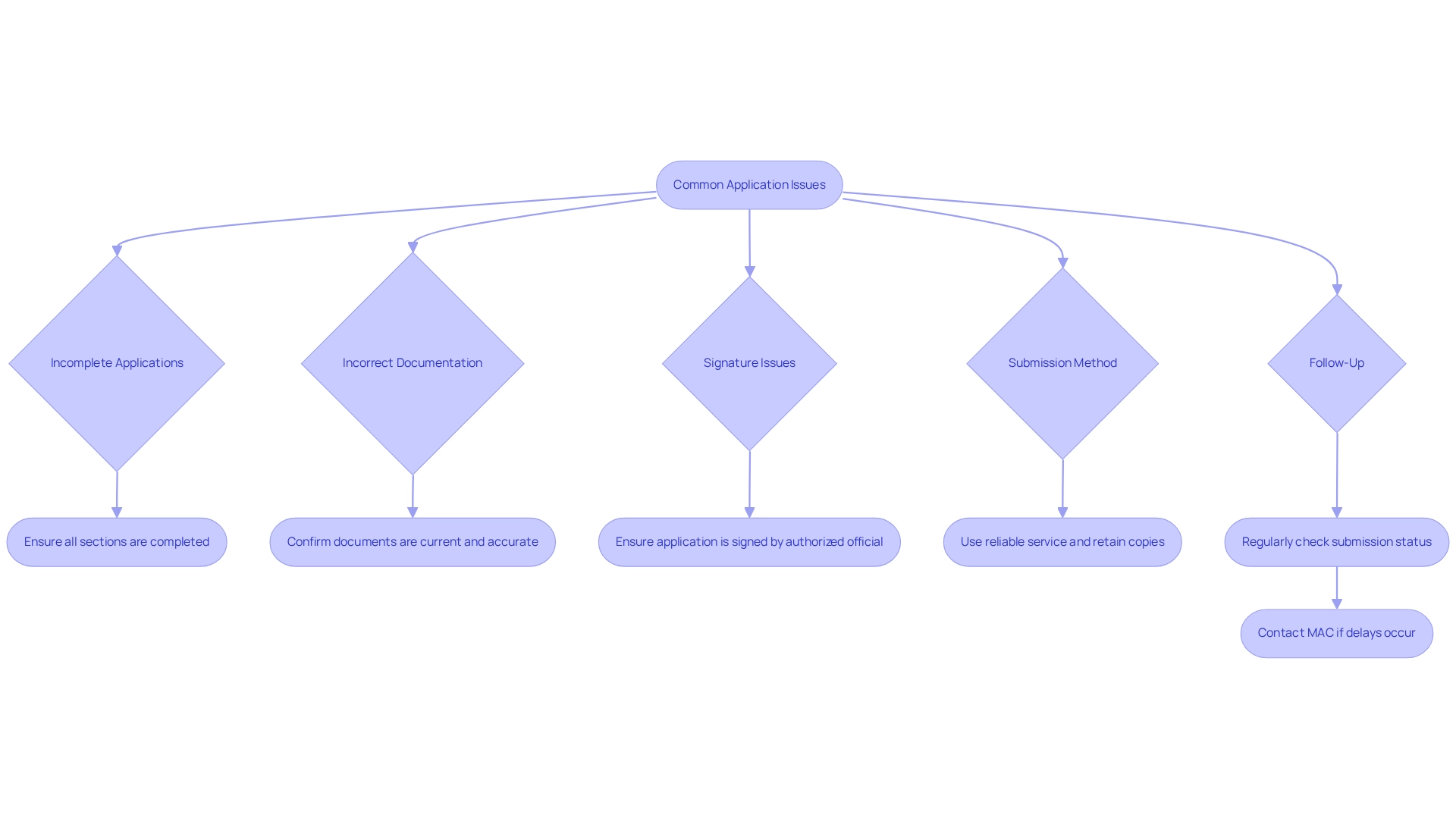
Troubleshoot Common Application Issues
Even with meticulous preparation, applicants may encounter challenges during the enrollment process. Common issues often arise, and understanding strategies for troubleshooting can significantly enhance the experience.
- Incomplete Applications: One of the most frequent causes of delays is missing information. It is crucial to ensure that every section of the application form is thoroughly completed. Statistics reveal that a substantial percentage of submissions are delayed due to incomplete information, emphasizing the importance of thoroughness in the submission process.
- Incorrect Documentation: Confirming that all supporting documents are current and accurately reflect the information submitted is essential. Discrepancies can lead to significant setbacks.
- Signature Issues: Applications must be signed by an authorized official; unsigned entries will be returned, resulting in unnecessary delays.
- Submission Method: When dispatching your request, utilize a reliable service and retain copies of all documents sent. For electronic submissions, strict adherence to PECOS guidelines is necessary to avoid complications.
- Follow-Up: Regularly checking the status of your submission post-sending is advisable. If delays occur, promptly contacting the Medicare Administrative Contractor (MAC) for assistance is crucial.
Healthcare compliance officers emphasize that addressing delays in submissions often relies on meticulous attention to detail and proactive communication with MACs. As Koziarz noted, “The costs associated with a breach are monumentous,” underscoring the necessity of thoroughness in the application process. By effectively addressing these common issues, applicants can streamline their enrollment experience and enhance their chances of timely approval. Furthermore, the ongoing need for continuous education against cybercrime highlights the importance of remaining vigilant and informed, ensuring that submissions are secure and complete.
Conclusion
Navigating the complexities of the CMS-855A Enrollment Application is essential for institutional providers seeking to bill Medicare effectively. Accurate and complete submissions are vital to avoid costly delays and rejections, as over 50% of applications are rejected due to missing information. Understanding the necessary documentation, such as the National Provider Identifier and legal business name, is paramount. By meticulously gathering required documents and adhering to the outlined steps for completing the application, providers can significantly enhance their chances of successful enrollment.
Moreover, troubleshooting common application issues is crucial in ensuring a smooth enrollment process. Addressing potential pitfalls—such as incomplete applications, incorrect documentation, and signature errors—can prevent unnecessary delays. The importance of proactive communication with Medicare Administrative Contractors cannot be overstated; it plays a significant role in resolving any challenges that may arise during the application process.
Ultimately, a thorough understanding of the CMS-855A application not only streamlines the enrollment process but also reinforces healthcare providers’ ability to serve Medicare beneficiaries effectively. By prioritizing accuracy and attention to detail, providers can enhance operational efficiency and ensure they are well-equipped to meet patients’ needs in an increasingly competitive healthcare landscape. Taking these steps safeguards compliance and contributes to the overall integrity of the Medicare system.


