Overview
North Carolina hospitals undergo rigorous evaluations against national care standards, showcasing notable advancements in patient satisfaction and safety. Leading institutions, such as Duke University Hospital and UNC Medical Center, exemplify these improvements.
While urban hospitals shine in this regard, rural facilities encounter significant challenges, including limited access and resources. This disparity underscores the urgent need for ongoing efforts aimed at bridging service quality gaps throughout the state.
Introduction
In the evolving landscape of healthcare, North Carolina hospitals stand at the forefront of enhancing patient care quality, showcasing significant advancements over the past decade. Institutions such as Duke University Hospital and UNC Medical Center are leading this charge, underscoring the state’s unwavering commitment to patient satisfaction and safety.
However, it is crucial to recognize that this progress is not uniform; disparities in care quality remain, particularly in rural areas where access to resources can be challenging. As hospitals adopt patient-centered initiatives and innovative care models, the focus is firmly placed on bridging these gaps, ensuring that all patients receive the high-quality care they rightfully deserve.
This article delves into the current state of patient care in North Carolina, examining the strengths and weaknesses of its healthcare facilities while highlighting the metrics that define success in this critical sector.
Overview of Patient Care Quality in North Carolina Hospitals
Over the past decade, North Carolina hospitals have made remarkable strides in enhancing the quality of care. Recent assessments reveal that numerous establishments in the state have achieved high ratings for client satisfaction and safety. Notably, institutions such as Duke University Hospital and UNC Medical Center consistently rank among the nation’s leaders in clinical outcomes and patient experiences.
As we look ahead to 2025, patient satisfaction ratings reflect a growing commitment to exceptional service, with many medical facilities launching effective programs aimed at improving the overall patient experience. Despite these advancements, challenges persist, particularly in rural areas where access to care and resources can be limited. The state’s healthcare landscape features a blend of high-performing urban medical centers and underperforming rural establishments, resulting in disparities in service quality across various regions.
To address these issues, North Carolina hospitals are increasingly focusing on person-centered care, prioritizing initiatives that enhance safety measures and foster a supportive environment for patients. For instance, UNC Health Rex’s recent leadership transition aims to expand operations in Wake County, emphasizing improved client support and service growth. This dedication is evident in the hospital’s consistently high ratings for safety and excellence, underscoring a commitment to enhancing healthcare delivery in the region.
As highlighted in NCHA’s 2024 Annual Report, “NCHA is excited to present our 2024 Annual Report, showcasing the progress and accomplishments made this year with member support,” reflecting the collaborative efforts driving these improvements. Integrating insights from CareSet’s extensive Medicare data can further empower healthcare stakeholders in North Carolina to understand and elevate the quality of service provided. By analyzing information from over 62 million beneficiaries and 6 million providers, CareSet offers valuable insights that can aid in addressing service standard disparities, particularly in rural areas.
As North Carolina hospitals advance their healthcare systems, the focus on high standards for patients remains paramount, propelling efforts to bridge gaps and enhance benchmarks across all facilities. According to NCHA’s 2023 Annual Report, the collaborative efforts among member facilities have significantly contributed to improving healthcare standards, further reinforcing the state’s commitment to healthcare excellence.
National Standards for Patient Care Quality
National standards for healthcare excellence are predominantly established by the Centers for Medicare & Medicaid Services (CMS) and the Joint Commission, which has been pivotal since its inception in 1951 in shaping healthcare delivery across the United States. These standards encompass a range of metrics, including safety, clinical effectiveness, and patient satisfaction, all of which are crucial for evaluating the performance of healthcare facilities. Key performance indicators (KPIs) such as readmission rates, infection rates, and experience scores serve as essential benchmarks for assessing the quality of services provided by North Carolina hospitals.
The CMS Hospital Compare tool provides a transparent platform, enabling individuals to evaluate hospitals based on these critical metrics, thereby fostering informed decision-making. It is anticipated that North Carolina hospitals will comply with these standards to ensure the delivery of safe, effective, and patient-centered services. Adhering to these standards is not only vital for securing accreditation for North Carolina hospitals but also significantly influences funding and reimbursement rates from Medicare and Medicaid.
In 2025, the Joint Commission will unveil revised safety standards for individuals, underscoring ongoing efforts to enhance healthcare quality. The inaugural UNIFY 2025 event, scheduled for September 16-17, 2025, in Washington, D.C., will convene healthcare leaders and policymakers to address pressing challenges in safety and quality, including the integration of artificial intelligence and the utilization of health data. This event underscores the importance of knowledge sharing among healthcare professionals as a catalyst for meaningful change in the industry.
Furthermore, the Core Quality Measures Collaborative (CQMC) is dedicated to minimizing unintended consequences and selecting new measures as improved options become available, reinforcing the commitment to advancing performance metrics. By leveraging comprehensive Medicare data insights from CareSet, healthcare stakeholders can analyze treatment pathways, understand provider interventions, and assess treatment approvals, ultimately enhancing service delivery and driving business success. As healthcare continues to evolve, the commitment to national standards for individual treatment remains paramount, ensuring that North Carolina hospitals not only fulfill compliance requirements but also aspire to achieve excellence in service.
Comparison Metrics: Evaluating Patient Care Quality
To effectively compare patient care quality, several key metrics are utilized:
- Satisfaction Scores: Derived from HCAHPS surveys, these scores reflect individuals’ perceptions of their care experience and are crucial for understanding service quality. In 2025, healthcare facilities are anticipated to disclose their HCAHPS outcomes every three months, as CMS releases these findings four times annually, offering prompt insights into satisfaction trends among individuals.
- Readmission Rates: This metric indicates the percentage of individuals who return to the hospital within 30 days of discharge. It serves as a critical quality indicator for care continuity, with lower rates suggesting better post-discharge management. In North Carolina, current readmission rates are being closely monitored, with comparisons to national averages highlighting areas for improvement.
- Infection Rates: Tracking hospital-acquired infections is essential for assessing the effectiveness of infection control practices. A decrease in these rates signifies enhanced safety measures for individuals receiving care.
- Mortality Rates: This metric assesses the number of fatalities occurring in the hospital, adjusted for risk factors of individuals. It provides insight into the overall quality of care and the effectiveness of treatment protocols.
- Timeliness of Care: This assesses how swiftly individuals receive essential treatments and interventions, which is crucial for enhancing outcomes and satisfaction.
These metrics collectively provide a comprehensive view of hospital performance, enabling detailed comparisons between hospitals in North Carolina and their national counterparts. By concentrating on these indicators, healthcare organizations can establish realistic and attainable objectives, ultimately improving client experience through data-driven decisions. As NRC Health specialists highlight, “Consistency and a long-term perspective are crucial for attaining significant and lasting enhancements in individual treatment and satisfaction.”
Furthermore, medical facilities are urged to gather information over extended periods to consider seasonality and other factors, which can result in more consistent and trustworthy metrics. Additionally, specific metrics associated with respiratory conditions, such as suitable testing for pharyngitis and asthma medication ratio, are also essential in assessing healthcare standards.
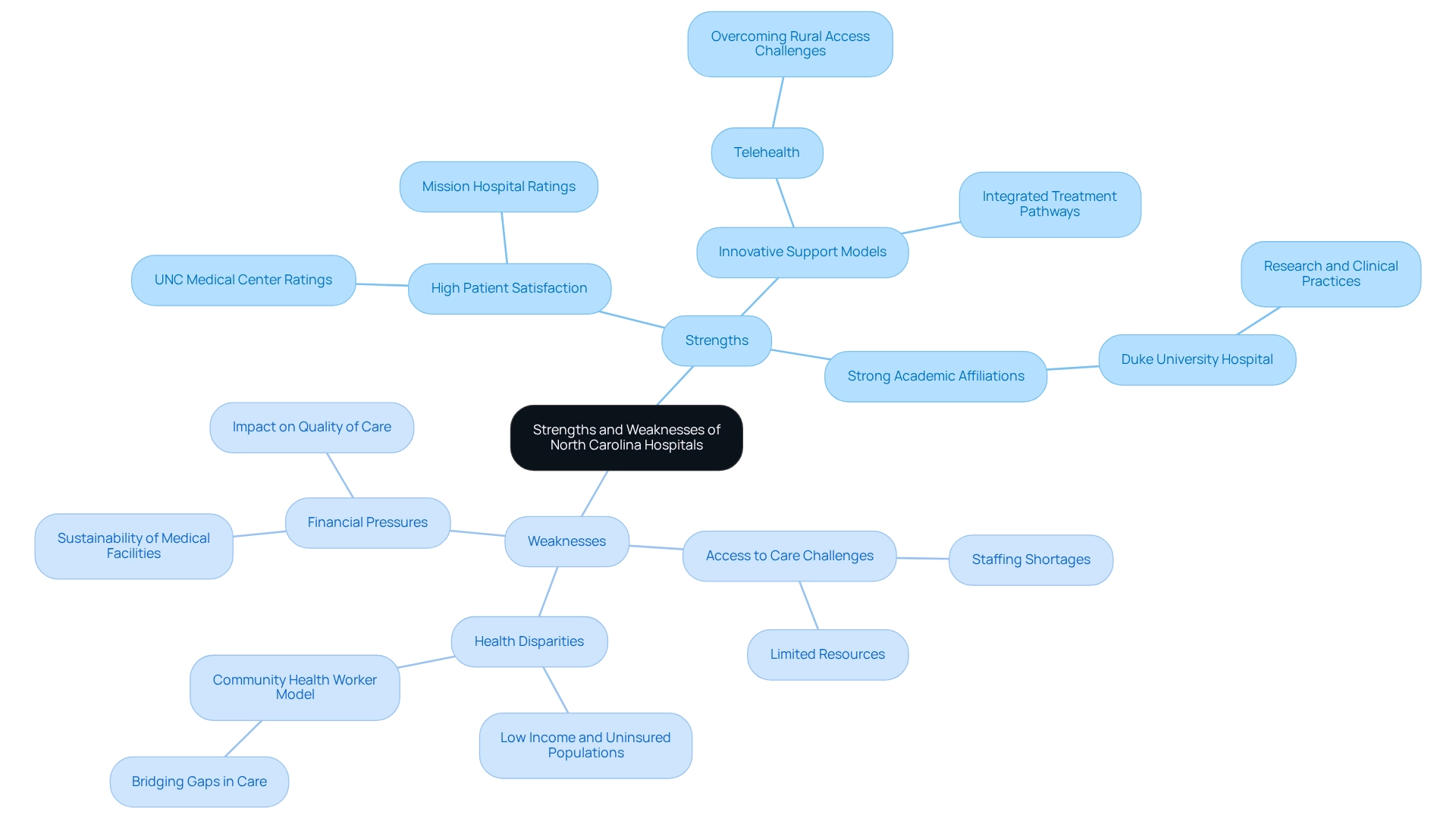
Strengths and Weaknesses of North Carolina Hospitals
North Carolina hospitals demonstrate significant strengths that bolster their reputation for quality care.
High patient satisfaction is a hallmark of facilities such as Mission Hospital and UNC Medical Center, which consistently achieve impressive ratings. This reflects their unwavering commitment to effective patient engagement and quality care delivery. In 2025, North Carolina hospitals were ranked among the best in the nation for patient satisfaction, underscoring their successful strategies in addressing patient needs.
Furthermore, the rise of innovative support models, including telehealth and integrated treatment pathways, enhances access for individuals and improves health outcomes, particularly in underserved areas. Telehealth has become an essential resource in overcoming rural healthcare access challenges, allowing patients to receive care without the barriers of distance. As highlighted in a 2024 report, “Telehealth is considered to be a key tool to help address rural healthcare access issues.”
Additionally, strong academic affiliations play a crucial role in enhancing the quality of care. Institutions like Duke University Hospital leverage their connections with leading medical schools to promote research and advanced clinical practices, fostering the adoption of evidence-based approaches.
Despite these strengths, challenges persist, especially in rural regions. Access to care remains a significant hurdle, as rural hospitals often face staffing shortages and limited resources, leading to longer wait times and restricted service availability. Notably, only 6% of OB/GYNs serve rural communities, despite 15% of the U.S. population residing in these areas, highlighting a stark disparity in services. Employing non-physician staff for substance use disorder treatment could be a beneficial strategy to mitigate these challenges.
Health disparities also pose a significant concern, particularly among low-income and uninsured populations. Innovative models, such as the Community Health Worker (CHW) model, have shown promise in bridging these gaps by providing essential support and resources to underserved communities. Implementing CHW programs can effectively tackle healthcare access issues by strengthening connections between healthcare providers and rural residents.
Moreover, financial pressures threaten the sustainability of many medical facilities, hindering their ability to invest in improvement initiatives. This financial strain can adversely affect the overall quality of care provided to patients.
In summary, while the strengths of North Carolina hospitals are commendable, addressing their weaknesses is crucial for enhancing the quality of patient care across the state.
Conclusion
The landscape of patient care in North Carolina hospitals illustrates a dynamic interplay of progress and ongoing challenges. Notable advancements in patient satisfaction and safety are evident, particularly in leading institutions such as Duke University Hospital and UNC Medical Center. These facilities exemplify the state’s commitment to delivering high-quality care through innovative practices and robust academic partnerships. However, disparities persist, particularly in rural areas where access to essential resources is limited, highlighting the need for targeted initiatives to ensure equitable care for all residents.
The framework of national standards established by organizations like CMS and the Joint Commission provides a crucial benchmark for evaluating hospital performance. Metrics such as patient satisfaction scores, readmission rates, and infection rates serve as vital indicators of care quality, guiding hospitals in their continuous improvement efforts. As North Carolina’s healthcare system evolves, emphasizing data-driven decision-making will be essential in bridging the gaps that exist within the state’s diverse healthcare landscape.
In conclusion, while North Carolina hospitals have made significant strides in enhancing patient care quality, the journey is far from complete. Addressing the challenges faced by rural facilities and underserved populations is imperative for achieving comprehensive healthcare equity. Through collaborative efforts and innovative care models, the state’s healthcare leaders can work towards a future where every patient, regardless of their location, receives the high-quality care they deserve. The commitment to excellence in patient care must remain steadfast, ensuring that all North Carolinians benefit from the advancements made in the healthcare sector.


