Overview
This article delves into the essential insights regarding CPT mammography codes, underscoring their critical role in billing, documentation, and the evolving landscape of breast cancer screening and diagnostics. Accurate coding, particularly for CPT Code 77063, which pertains to bilateral screening mammography, is imperative for ensuring proper reimbursement and enhancing patient outcomes. This assertion is bolstered by data reflecting Medicare payment trends and highlights the necessity of comprehensive screening practices. As we navigate this complex field, understanding the nuances of coding will empower healthcare professionals to optimize their billing processes and improve overall patient care.
Introduction
In the realm of breast health, precise coding and documentation are pivotal for ensuring timely diagnoses and effective treatment pathways. The utilization of various CPT codes—such as 77063 for bilateral screening mammography and 77065 for diagnostic mammography—plays a critical role in the financial viability of healthcare practices while enhancing patient outcomes.
As advancements in imaging technology and evolving Medicare reimbursement policies shape the landscape of breast cancer detection and management, understanding these codes becomes increasingly essential.
This article delves into the significance of key CPT codes in breast imaging, highlighting their impact on reimbursement, clinical practices, and the overall drive for improved patient care in a complex healthcare environment.
CPT Code 77063: Screening Mammography, Bilateral
CPT mammography codes, including CPT Code 77063, are integral to bilateral screening mammography, a vital procedure for the early detection of cancer in the mammary glands. This code specifically applies when both breasts are screened, typically involving two-view imaging. Accurate documentation of this procedure is essential for proper billing and ensuring that providers receive appropriate compensation. Medicare generally offers favorable payment rates for this code, underscoring its importance as a fundamental service for healthcare providers.
In 2025, updates to Medicare payments for CPT Code 77063 reflect ongoing initiatives aimed at enhancing accessibility to breast cancer screening. Importantly, this code can be billed alongside other imaging services, such as tomosynthesis, which enhances diagnostic accuracy. Current statistics reveal that mammography prevalence is at 65.7% among women aged 50–74 years who face three or more adverse social determinants of health (SDOH) and health-related social needs (HRSNs), emphasizing the critical role of comprehensive screening in this demographic.
Moreover, the transition from film-screen to digital mammography between 2007 and 2011 has significantly transformed screening practices, making it crucial to consider technological advancements when discussing CPT Code 77063. Insights from CareSet’s extensive Medicare data solutions illustrate how providers navigate patient treatment pathways using NDC and HCPCS codes, ensuring that interventions align with the latest compensation strategies and treatment approvals. Case studies suggest that while reimbursement for CPT Code 77063 is generally favorable, there are limitations in the data concerning mammography use, particularly due to reliance on self-reported data. This highlights the necessity for caution in interpreting the utilization rates of CPT mammography codes, indicating that further research is needed to validate findings and enhance generalizability.
Expert opinions further underscore the significance of CPT mammography codes, including CPT Code 77063, in cancer detection. Notably, substantial proportions of women with limited life expectancy continue to undergo mammography screening. Dr. James S. Goodwin states, “However, substantial proportions of women with limited life expectancy underwent mammography screening,” indicating a pressing need for continued advocacy for accurate and accessible breast cancer screening services. Additionally, the study’s findings were corroborated by the Cancer Prevention Research Institute of Texas and the National Institutes of Health, adding further credibility to the statistics and insights presented.
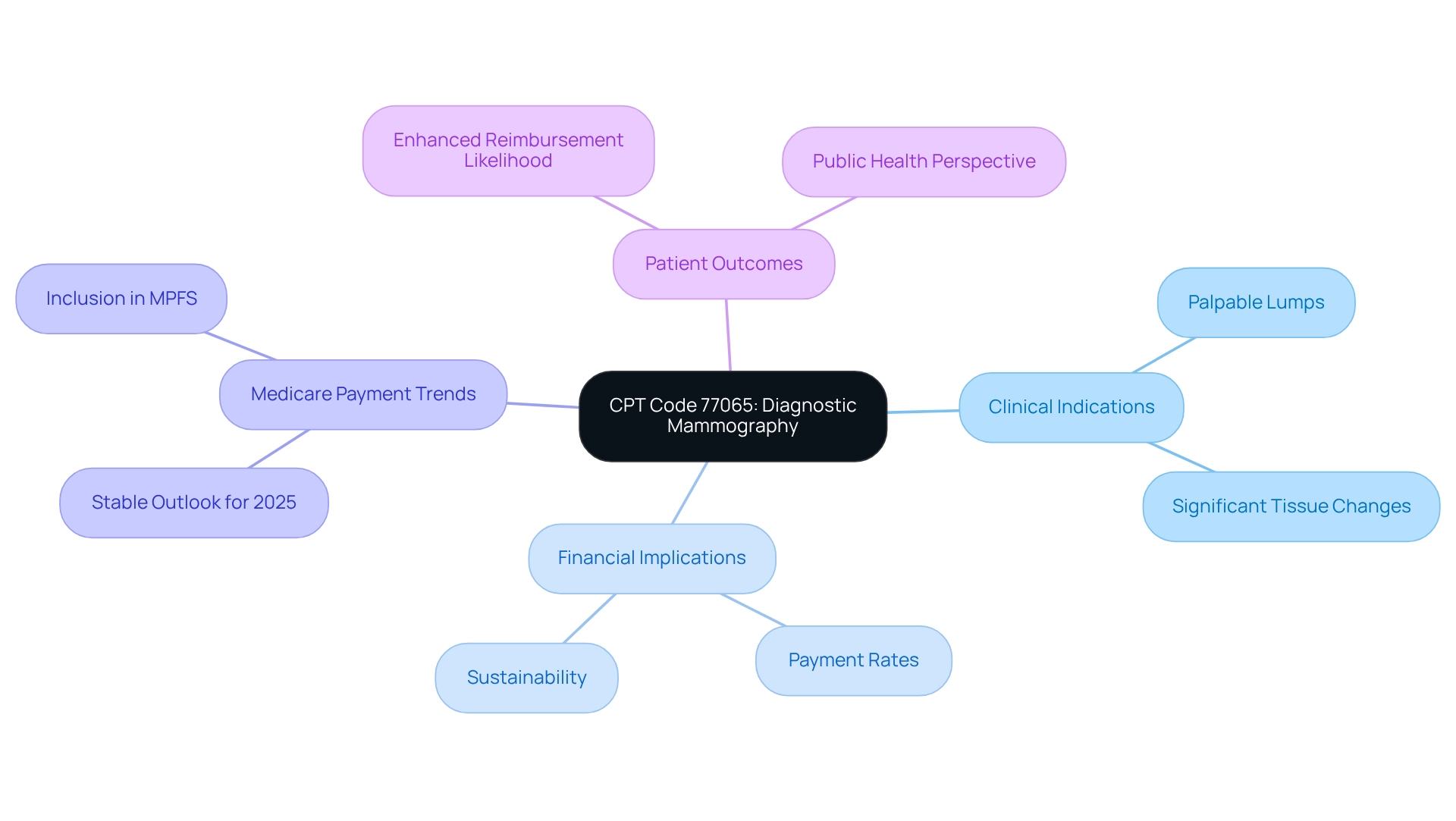
CPT Code 77065: Diagnostic Mammography, Bilateral
CPT Code 77065 is specifically designated for diagnostic mammography performed bilaterally, a procedure that is essential for patients who exhibit symptoms or have abnormal findings from prior screening mammograms. The precision in coding for this procedure, particularly regarding the CPT mammography codes, is vital, as it directly impacts payment rates and the financial sustainability of healthcare practices. Providers must meticulously document clinical indications for the diagnostic mammography, which may include symptoms such as palpable lumps or significant changes in tissue.
As we look toward 2025, the landscape of Medicare payment for diagnostic mammography is evolving, with trends indicating a stable outlook for CPT Code 77065, which is included in the Medicare Physician Fee Schedule (MPFS). This stability is crucial, reinforcing the importance of breast imaging from a public health perspective. Furthermore, understanding the clinical indications and ensuring accurate coding with CPT mammography codes can enhance the likelihood of successful reimbursement, ultimately bolstering the financial health of practices that prioritize care. CareSet’s comprehensive analysis of over $1.1 trillion in annual Medicare claims data equips healthcare stakeholders with critical insights into drug utilization and treatment pathways. This data not only underscores the importance of precise coding in the financial sustainability of healthcare practices but also contributes to the overall enhancement of patient outcomes.
CPT Code 76641: Breast Ultrasound, Unilateral
CPT Code 76641 pertains to unilateral mammary ultrasound, a critical imaging modality in the diagnostic workflow. This technique is especially beneficial when mammograms indicate possible abnormalities or when individuals exhibit specific symptoms. By providing real-time imaging, mammary ultrasound aids in distinguishing between solid masses and cysts, thereby enhancing diagnostic accuracy. In 2025, Medicare payment rates for mammary ultrasound procedures reflect the growing recognition of their importance in patient care, with increased usage observed in clinical environments. Recent statistics indicate a significant rise in the use of breast ultrasound, underscoring its role in comprehensive diagnostic strategies.
Precise documentation and the application of CPT mammography codes for this service are essential for ensuring payment, making it imperative for providers to understand the indications for its use. As John Verhovshek, a contributing editor at AAPC, emphasizes, ‘Accurate documentation and reimbursement are ensured through the use of CPT mammography codes.’ This is particularly significant as providers navigate the complexities of Medicare treatment pathways, utilizing ICD, NDC, and HCPCS codes to define interventions and track individual journeys from diagnosis to treatment.
Case studies demonstrate that employing CPT mammography codes, including CPT Code 76641, not only streamlines the diagnostic process but also positively impacts outcomes, especially when used in conjunction with mammography. For instance, a recent case study highlighted how the integration of mammary ultrasound in diagnostic protocols led to earlier identification of lesions, ultimately improving treatment outcomes. This aligns with a broader analysis of Medicare claims data, which shows that effective provider interventions can significantly enhance patient care.
As the role of mammary ultrasound in diagnostic imaging continues to evolve, its significance in the overall diagnostic strategy cannot be overstated.
CPT Code 19100: Breast Biopsy, Needle Core
CPT mammography codes, particularly CPT Code 19100, are integral to the process of percutaneous needle core biopsy in the mammary region. This procedure is essential for acquiring tissue samples from suspicious lesions, facilitating the diagnosis of conditions such as breast cancer. Accurate coding for this procedure is paramount, as it directly influences Medicare payment rates and overall care management strategies. As we look ahead to 2025, the reimbursement landscape for mammary biopsy procedures continues to evolve, underscoring the necessity for providers to meticulously document the specifics of each procedure.
The importance of precise coding, including CPT mammography codes, cannot be overstated. Research indicates that individuals undergoing needle biopsies face a 2.08% risk of requiring multiple surgeries for cancer, highlighting the critical need for accurate diagnosis and treatment pathways. Furthermore, insights gleaned from Medicare claims data illuminate how providers navigate the individual journeys of patients through various lines of therapy, accentuating the role of CPT Code 19100 in enabling timely and effective treatment options. This navigation often incorporates the use of NDC and HCPCS codes, which delineate the interventions necessary to support the treatment process.
A case study titled ‘Biopsy Patterns and Outcomes in SEER-Medicare Data’ underscores the efficacy of biopsy practices, offering potential guidance for clinical guidelines and enhancement of care strategies. Additionally, understanding the interconnections between HCPCS, ICD, and NDC codes within the context of biopsy procedures can further empower healthcare providers to refine treatment decisions and improve patient outcomes.
CPT mammography codes, including CPT Code 19100, are frequently employed in conjunction with imaging studies. Grasping their application is critical for navigating the complexities of Medicare treatment pathways. As the healthcare landscape evolves, maintaining an up-to-date knowledge of coding practices and compensation policies will enable providers to efficiently manage these complexities, ultimately leading to improved outcomes for patients receiving care.
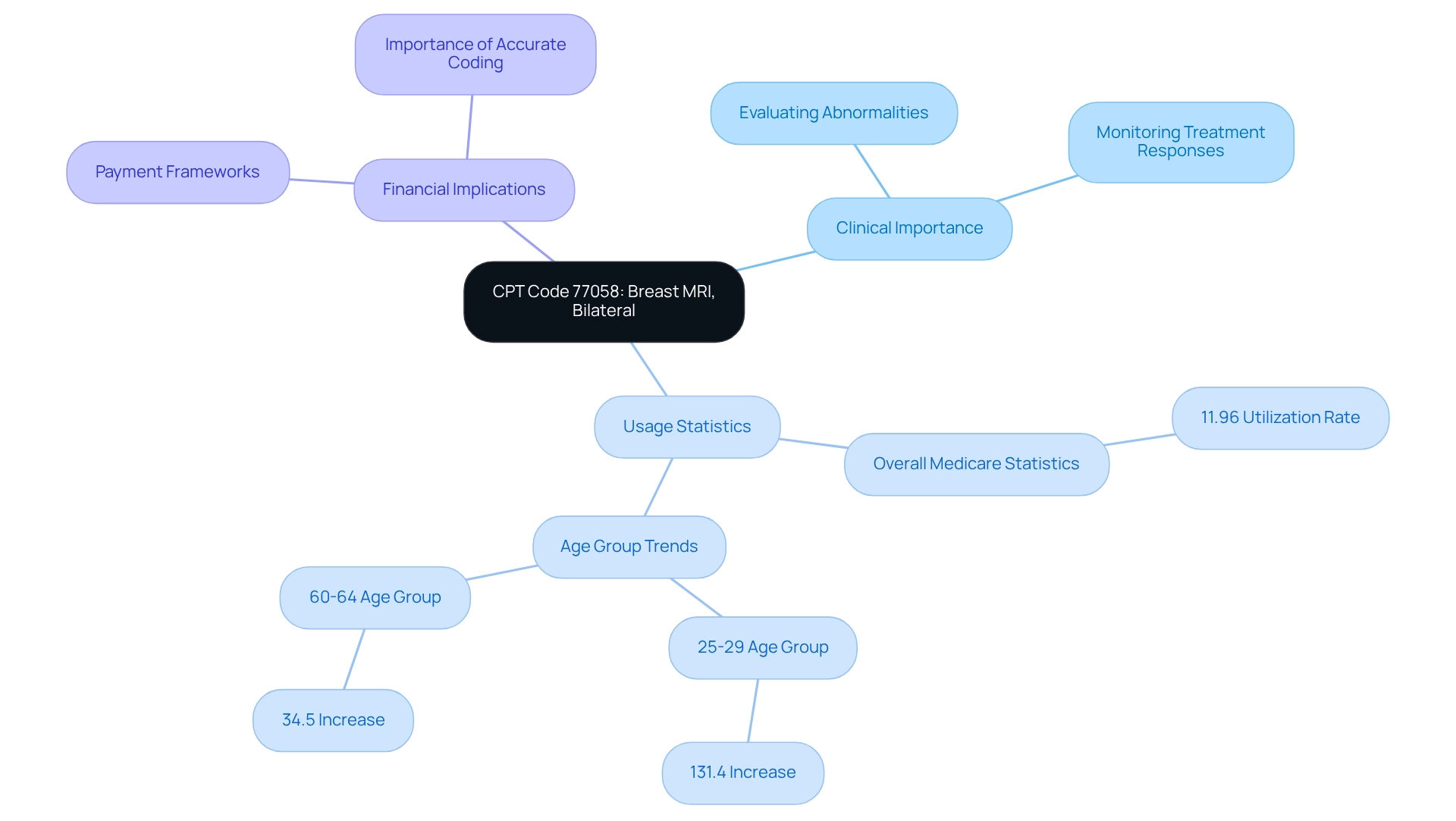
CPT Code 77058: Breast MRI, Bilateral
CPT Code 77058 is designated for bilateral mammary MRI, a vital imaging technique for evaluating abnormalities, particularly in high-risk patients or those with a prior history of cancer. This advanced imaging modality provides high-resolution images that are crucial for assessing disease extent and monitoring treatment responses. Precise coding and comprehensive documentation are essential for obtaining payment, making it imperative for providers to understand the clinical indications that validate the use of MRI.
Current statistics reveal that among women enrolled in Medicare for ten years or more, 11.96% underwent MRI, underscoring its growing role in cancer management. A notable case study titled ‘Age Group Analysis of Breast MRI Utilization’ examined trends from 2007 to 2017, demonstrating a significant increase in MRI use across all age groups, with the 25-29 age group experiencing a remarkable 131.4% rise. This trend highlights the increasing reliance on MRI for early detection and ongoing assessment in younger populations.
Understanding the payment framework for CPT mammography codes, such as CPT Code 77058, is crucial for practices aiming to optimize financial performance. As of 2025, Medicare payment rates for breast MRI procedures indicate a growing acknowledgment of their clinical value. Providers must stay informed about these rates and the evolving guidelines to effectively advocate for their patients’ needs while maintaining the financial health of their practices. Additionally, insights from Medicare claims data reveal how providers navigate treatment pathways, emphasizing the importance of accurate coding in securing necessary approvals and enhancing healthcare provider engagement. As Anuja Mohla stated, “This webcast will address key issues affecting observation data integrity and offer strategies for improving consistency in reporting,” underscoring the significance of accurate data in the reimbursement process.
Conclusion
The importance of accurate coding and documentation in breast health is paramount, as underscored by the various CPT codes discussed throughout this article. Each code, from 77063 for bilateral screening mammography to 77058 for breast MRI, plays a crucial role in ensuring appropriate reimbursement, facilitating timely diagnoses, and enhancing patient care. Understanding these codes is essential for healthcare providers to navigate the complexities of Medicare reimbursement policies and bolster the financial viability of their practices.
As advancements in imaging technology continue to shape the landscape of breast cancer detection and management, the significance of these coding practices becomes increasingly evident. This article illustrates how precise documentation not only supports financial outcomes but also enhances the accuracy of diagnoses and treatment pathways. This dual focus on financial viability and quality of care underscores the necessity for providers to remain vigilant and informed about evolving coding practices and reimbursement rates.
In conclusion, the effective use of CPT codes is integral to optimizing breast health services. By prioritizing accurate coding and documentation, healthcare providers can ensure that patients receive the best possible care while maintaining the sustainability of their practices. As the healthcare environment continues to evolve, embracing these practices will be vital in the ongoing fight against breast cancer and in the pursuit of improved patient outcomes.


