Overview
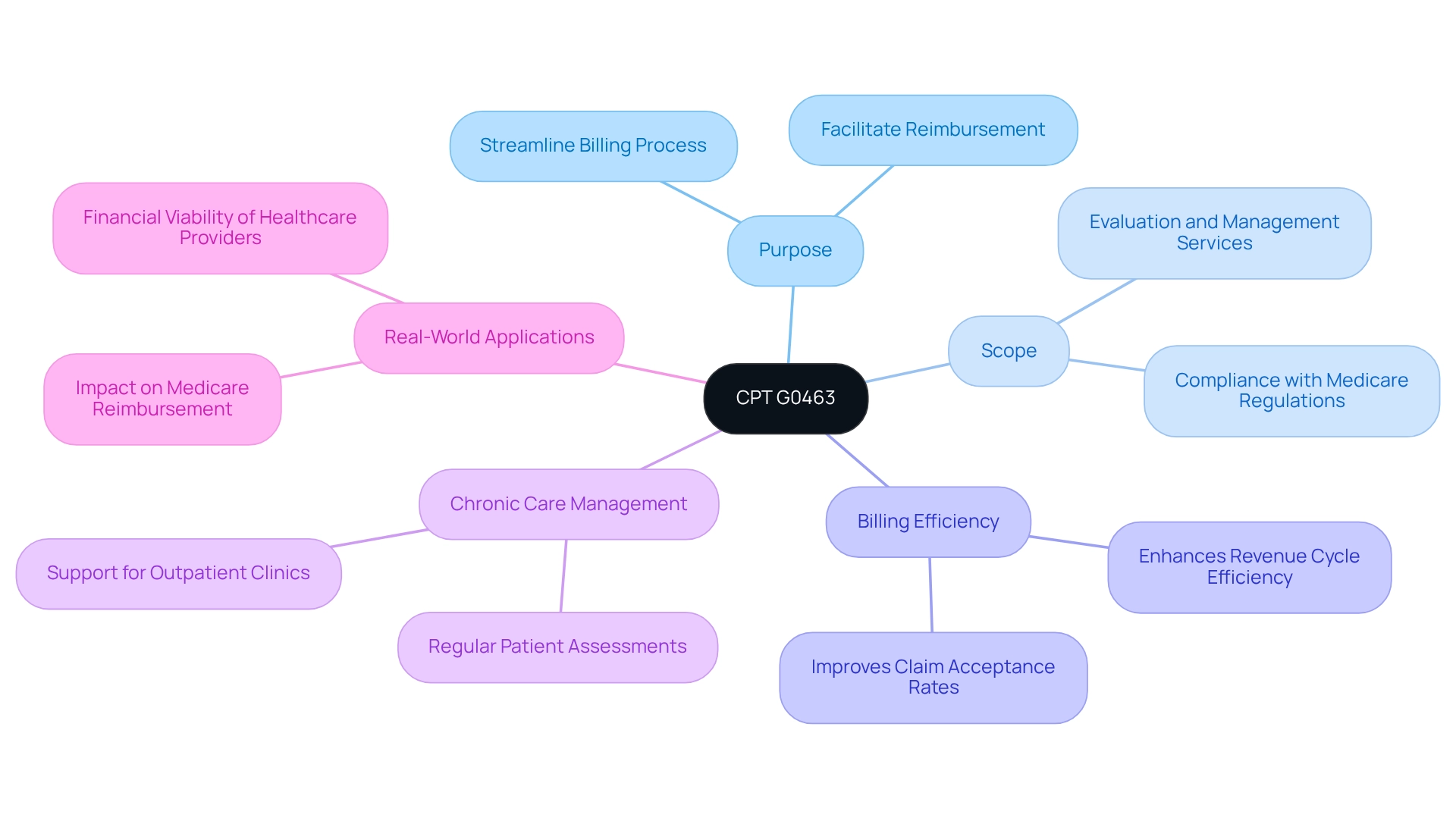
The article centers on CPT G0463, a pivotal billing code for outpatient clinic appointments that encompass evaluation and management services. It underscores the necessity of precise documentation and compliance with Medicare regulations, which are essential for optimizing revenue cycle efficiency. By adhering to these guidelines, healthcare providers can secure appropriate reimbursement, thereby enhancing their financial sustainability. This focus on CPT G0463 not only highlights its relevance but also prompts healthcare professionals to consider the broader implications of effective billing practices.
Introduction
In the intricate realm of healthcare billing, CPT G0463 emerges as a vital code for outpatient clinic visits, encapsulating essential evaluation and management services. This code is meticulously designed to streamline the billing process for hospitals, facilitating not only accurate reimbursement but also playing a crucial role in chronic care management and patient evaluations.
As healthcare providers navigate the complexities of coding and compliance, grasping the full scope and applications of CPT G0463 becomes imperative. Its implications extend well beyond mere billing, influencing both the quality of patient care and the financial sustainability of healthcare institutions.
With the ever-evolving landscape of healthcare reimbursement policies, an in-depth examination of CPT G0463 unveils its importance in ensuring operational success and enhancing patient outcomes in outpatient settings.
Define CPT G0463: Purpose and Scope
The CPT G0463 code is a vital reference for hospital outpatient clinic appointments that encompass evaluation and management (E/M) services. The CPT G0463 code was established to streamline the billing process for outpatient services provided by hospitals, enabling facilities to charge a fee associated with these visits. The scope of CPT G0463 includes comprehensive patient evaluations and management strategies, ensuring that all services delivered during the visit are recorded under a single code. This is essential for compliance with Medicare regulations, which mandate the use of coding like CPT G0463 to facilitate reimbursement.
The significance of CPT G0463 transcends mere invoicing; it plays a pivotal role in chronic care management, necessitating regular patient assessments in outpatient settings. Accurate documentation and invoicing practices for CPT G0463 can significantly enhance a hospital’s revenue cycle efficiency and improve claim acceptance rates. As noted by Brian Bertrand, a hospital’s revenue cycle efficiency enhances while claim acceptance rates rise when healthcare providers employ precise documentation and billing methods for CPT G0463. This underscores the critical nature of proper coding, including CPT G0463, in maximizing financial outcomes.
Furthermore, G codes under HCPCS, including G code 463, are instrumental in recording specific medical services and procedures, particularly in health programs that cover evaluations, screenings, and chronic care management. CareSet’s extensive data analytics for public health programs, which incorporates over 100 external data sources, provides valuable insights into these coding practices, emphasizing the importance of CPT codes in ensuring accurate reimbursement and enhancing patient care.
Real-world applications of CPT G0463 illustrate its impact on Medicare reimbursement. By effectively utilizing the CPT G0463 code, healthcare providers can ensure they receive appropriate compensation for the services rendered, thereby bolstering their financial viability. As the healthcare landscape evolves, understanding the purpose and scope of CPT G0463 becomes increasingly critical for compliance and operational success in outpatient billing.
Explore Applications of CPT G0463 in Clinical Settings
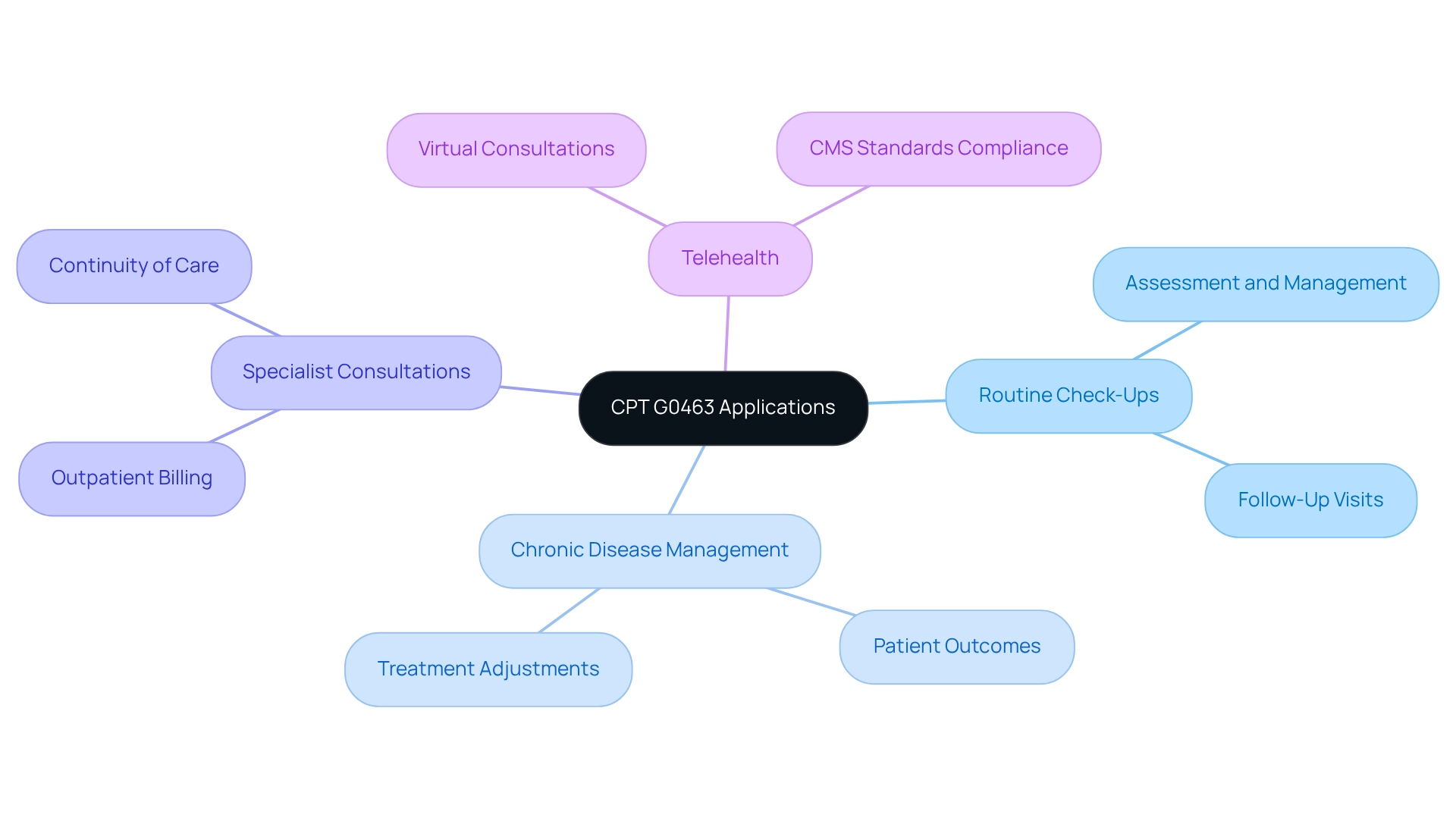
CPT G0463 is primarily employed in hospital outpatient environments, facilitating assessment and management services for patients. Its applications are diverse and critical for effective patient care.
Routine check-ups frequently utilize this code for follow-up visits, enabling healthcare providers to assess ongoing health issues and adjust treatment plans accordingly. Understanding how this aligns with the ICD framework helps providers ensure precise documentation and reimbursement.
Chronic disease management is another area where CPT plays a crucial role, overseeing patients with chronic conditions and facilitating comprehensive evaluations and essential adjustments to treatment approaches. Statistics indicate that effective chronic disease management can significantly improve patient outcomes and reduce hospital readmissions. Insights from Medicare claims data reveal how interventions linked to CPT G0463 can enhance patient journeys through various lines of therapy.
Specialist consultations also benefit from this code, as it can be billed for outpatient visits when patients are referred to specialists within the hospital. This ensures that comprehensive care is documented and reimbursed appropriately, which is vital for maintaining continuity of care across various healthcare environments. The growing use of telehealth has broadened the relevance of CPT G0463 to virtual consultations, provided that these consultations meet the outpatient service standards set by CMS. This adjustment is crucial as healthcare progresses toward more accessible and remote care options, reflecting the shifting dynamics of patient treatment routes.
In 2025, the importance of CPT in hospital outpatient environments is underscored by ongoing assessments from CMS, which are scheduled to reevaluate the APC classification for associated codes. This reflects a commitment to maintaining the integrity and effectiveness of billing practices amid changing healthcare dynamics. Moreover, case studies emphasize the successful application of CPT in chronic disease management, showcasing its influence on patient care and healthcare efficiency. Significantly, the geometric mean per diem expense for hospital-based providers offering four-service days is $367.79, demonstrating the financial effects of effectively utilizing the specific CPT code. Additionally, consistent billing practices, as highlighted in the case study on ‘Consistency in 340B Reporting,’ are essential for ensuring program integrity and enhancing the overall quality of care.
Detail Billing and Coding Procedures for CPT G0463
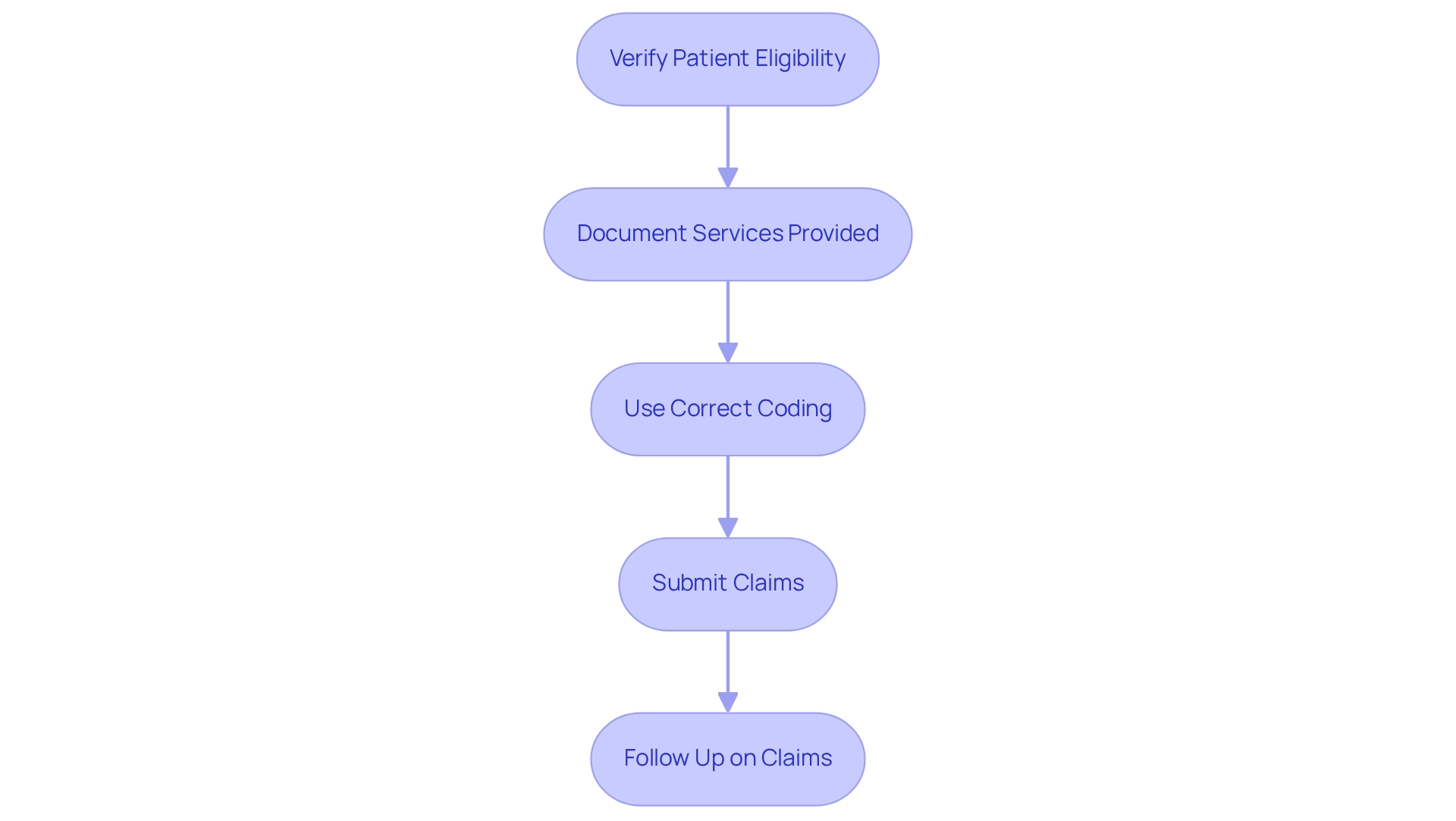
To effectively bill for CPT G0463, healthcare providers must follow these essential procedures:
- Verify Patient Eligibility: It is crucial to confirm that the patient qualifies for outpatient services under their insurance plan, particularly Medicare-related options. This verification step directly influences reimbursement rates and compliance with billing regulations, especially when navigating the complexities of treatment pathways.
- Document Services Provided: Comprehensive documentation of all evaluation and management services performed during the visit is necessary. This includes a thorough patient history, examination results, and treatment strategies, which are vital for validating claims and ensuring adherence to healthcare guidelines. A solid understanding of the relationship between ICD, NDC, and HCPCS codes can further enhance documentation accuracy.
- Use correct coding: CPT G0463 should be designated as the primary code when submitting claims for the outpatient visit. It is imperative to apply any relevant modifiers, such as those for telehealth services, to accurately reflect the nature of the visit and improve claim acceptance rates. This coding practice is essential for aligning with the approval processes and treatment interventions of the healthcare program.
- Submit Claims: Claims must be submitted to the appropriate payer, ensuring compliance with their specific billing requirements. This includes adhering to submission deadlines and providing any additional documentation that may be required, which is crucial for enhancing revenue cycle management and ensuring that treatments are authorized under Part D Plans.
- Follow Up on Claims: Regular monitoring of the status of submitted claims and prompt addressing of any denials or requests for further information is necessary. This proactive approach is vital for ensuring timely reimbursement and maintaining financial stability within healthcare organizations, particularly in light of insights derived from CareSet’s comprehensive Medicare data solutions.
Understanding and applying these invoicing procedures not only enhances claim acceptance rates but also optimizes revenue cycle management, ultimately supporting high-quality patient care. As highlighted in the case study ‘Importance of CPT G0463 in Medical Billing,’ a proper understanding and execution of payment practices related to CPT G0463 can significantly improve claim acceptance rates and simplify revenue cycle management for healthcare facilities. Moreover, a common concern among providers, as reflected in a quote from Cat00a@gmail.com, is the confusion surrounding charges for CPT G0463 along with visit fees. Addressing such misunderstandings is essential for effective invoicing practices. Furthermore, statistics indicate that outsourcing medical billing services can improve efficiency and increase revenue for healthcare providers, underscoring the critical importance of effective billing practices.
Analyze Reimbursement Policies and Payer Considerations for CPT G0463
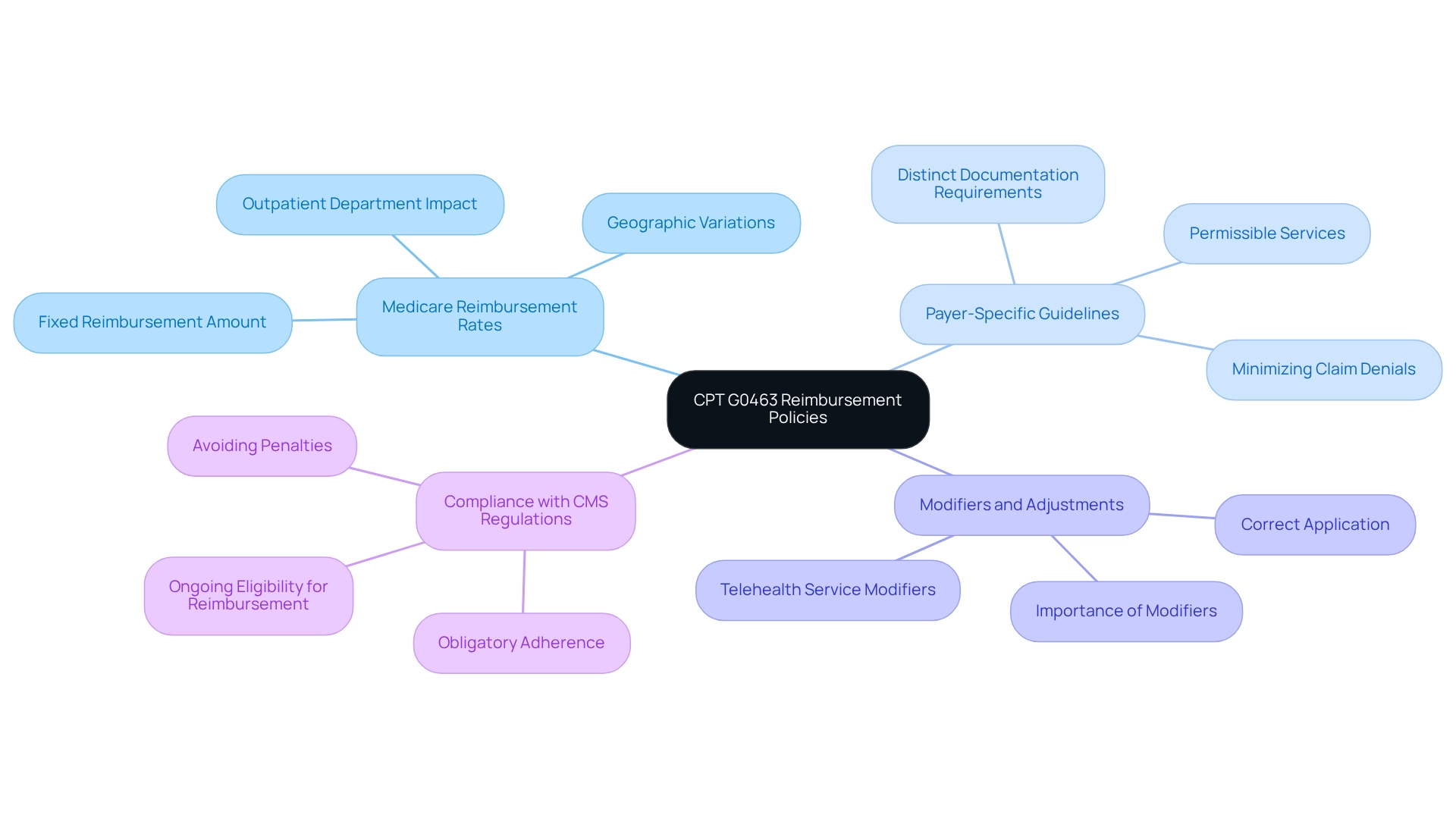
Reimbursement for CPT code is influenced by various policies set by government health programs and other insurance providers, necessitating careful navigation by healthcare practitioners. Key considerations include:
-
Medicare Reimbursement Rates: Medicare generally offers a fixed reimbursement amount for services billed under CPT G0463. This amount can fluctuate based on geographic location and the specific outpatient department involved, reflecting the need for providers to stay informed about regional variations.
-
Payer-Specific Guidelines: Each insurance company may implement distinct guidelines for CPT G0463, which encompass documentation requirements and permissible services. Familiarity with these guidelines is essential for providers to minimize the risk of claim denials and ensure smooth reimbursement processes.
-
Modifiers and Adjustments: The application of modifiers is critical, as they can significantly influence reimbursement rates. For instance, modifiers related to telehealth services must be correctly applied to secure appropriate payment, highlighting the importance of understanding when and how to use them effectively.
-
Compliance with CMS Regulations: Adherence to the Centers for Medicaid Services (CMS) guidelines is obligatory for providers. Compliance not only helps avoid penalties but also ensures ongoing eligibility for reimbursement, reinforcing the importance of staying updated on regulatory changes.
G codes under HCPCS are utilized to record particular medical services and procedures for government health programs, including evaluations, screenings, and chronic care management. In 2025, Medicare reimbursement policies for CPT code will continue to evolve, necessitating ongoing education and adaptation by healthcare providers. CareSet integrates more than 100 external data sources for comprehensive insights, emphasizing the importance of utilizing extensive data to understand reimbursement policies. As noted by Medical Bill Gurus, healthcare providers need to understand the guidelines and requirements associated with CPT G0463 to ensure accurate and timely reimbursement for their services. Real-world examples illustrate that understanding these payer considerations can lead to improved reimbursement outcomes and enhanced financial stability for healthcare practices, ultimately empowering stakeholders with the insights needed for data-driven success.
Conclusion
CPT G0463 stands as a pivotal code in healthcare billing for outpatient clinic visits, effectively streamlining reimbursement for essential evaluation and management services. Its importance transcends mere financial implications; it plays a crucial role in chronic care management and enhances patient evaluations, which are vital for the operational success of healthcare institutions.
The applications of CPT G0463 are extensive, covering routine check-ups, chronic disease management, specialist consultations, and telehealth services. Each application underscores the code’s significance in delivering comprehensive patient care while ensuring that providers receive appropriate compensation. As telehealth continues to gain traction, mastering the utilization of CPT G0463 becomes increasingly essential.
To optimize claim acceptance rates and bolster revenue cycle management, healthcare providers must adhere to effective billing and coding procedures. Implementing best practices—such as verifying patient eligibility and monitoring claims—is essential for enhancing financial stability and maintaining high-quality care. Furthermore, a thorough understanding of reimbursement policies and payer considerations is crucial, as these factors significantly influence financial outcomes.
In conclusion, CPT G0463 represents more than just a billing code; it is a fundamental element of effective outpatient care and financial sustainability for healthcare institutions. By mastering its applications and coding practices, healthcare providers can adeptly navigate the complexities of billing, ultimately leading to improved patient outcomes and operational success.


