Overview
Hospital systems generally provide more effective and coordinated care compared to traditional healthcare models, leading to better patient outcomes and increased satisfaction. This is particularly significant as integrated hospital systems leverage data and resources to enhance service delivery. In contrast, conventional models often struggle with continuity and comprehensive management, resulting in disjointed patient experiences. By understanding these dynamics, stakeholders can appreciate the potential for improved healthcare delivery and patient satisfaction.
Introduction
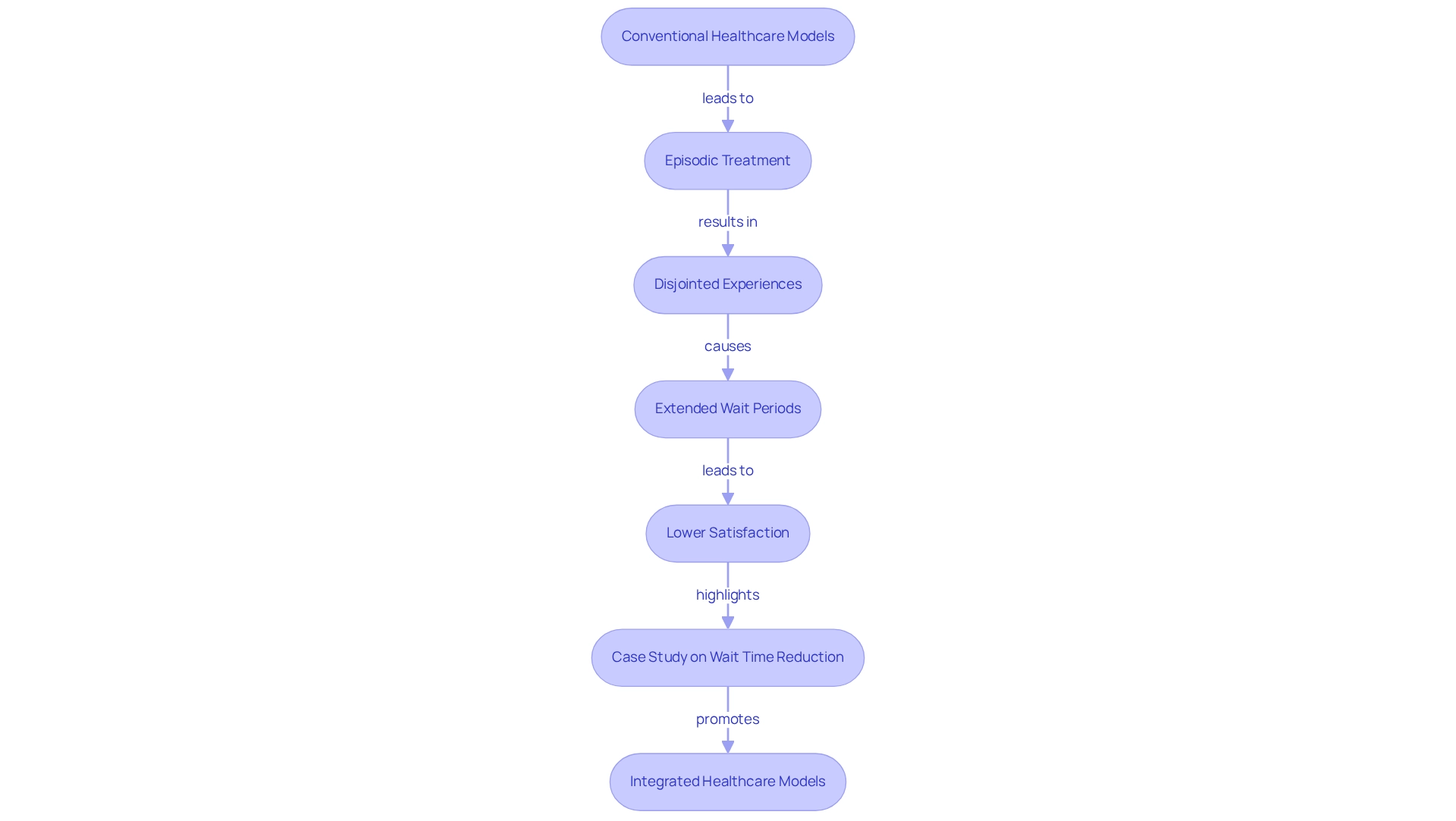
In the intricate landscape of healthcare, distinguishing between hospital systems and traditional healthcare models is crucial for shaping patient experiences and outcomes. Hospital systems, defined by their integrated networks of facilities and providers, deliver a comprehensive approach to care that prioritizes continuity and collaboration. Conversely, traditional models often function in silos, concentrating on episodic treatment, which can result in fragmented care and patient dissatisfaction.
As the healthcare sector evolves, grasping these differing structures is essential for stakeholders intent on enhancing patient care and operational efficiency. This article examines the effectiveness of these two models, investigating how integrated systems utilize data and technology to improve outcomes while also shedding light on the challenges traditional approaches face in providing cohesive healthcare experiences.
Defining Hospital Systems and Traditional Healthcare Models
Hospital systems represent integrated collections of medical facilities and providers, delivering a comprehensive array of services that include both inpatient and outpatient support, typically managed under a unified structure. These hospital systems often encompass various hospitals, specialty clinics, and long-term treatment centers, working together to ensure coordinated and ongoing support for individuals. In contrast, conventional medical models consist of standalone hospitals or clinics operating independently, primarily focusing on episodic treatment. This lack of integration can lead to significant gaps in individual treatment and communication among providers.
Understanding these definitions is crucial, as they highlight the structural differences that profoundly influence patient outcomes and the efficiency of healthcare delivery. For instance, statistics reveal that in 2023, half of all hospitals reported charity expenses constituting 1.2% or less of their operating costs, underscoring the financial pressures faced by standalone facilities. Furthermore, a case study examining the impact of Medicare Advantage on hospital services indicates that from 2015 to 2023, the share of inpatient days associated with Medicare Advantage rose from 13% to 24%, while traditional Medicare’s share decreased. This shift suggests that hospital systems that are integrated may be better equipped to adapt to evolving individual needs and coverage requirements, ultimately enhancing care and operational efficiency.
Moreover, CareSet’s innovative data science products illustrate how leveraging comprehensive Medicare data solutions can empower healthcare strategies by providing insights from over 62 million beneficiaries and 6 million providers. This data is vital for analyzing treatment pathways, understanding provider interventions, and evaluating treatment approvals. As Sara Vaezy noted, “It’s less about adjusting to the pandemic and more about utilizing our insights to advance the health framework’s mission to assist all individuals in a more efficient, scalable, and fair manner.” This perspective underscores the broader mission of healthcare networks in delivering integrated support. Additionally, the trend of mergers among hospitals in various geographic regions may lead to increased costs, raising significant considerations regarding the implications of hospital integration on operational efficiency and service for individuals. For pharmaceutical market access managers, understanding these dynamics is essential, as they directly influence market access strategies and engagement initiatives.
Evaluating the Effectiveness of Hospital Systems
Healthcare organizations undergo rigorous evaluation based on their capacity to deliver exceptional service, manage expenses efficiently, and maintain client satisfaction. Research indicates that integrated service frameworks significantly enhance client outcomes by fostering better coordination, minimizing service duplication, and improving communication among providers. For instance, a Deloitte report reveals that hospital systems that adopt value-focused models achieve superior health outcomes while effectively managing costs. Brian, a Manager at Deloitte Consulting LLP, asserts, ‘the integration of data and technology is essential in value-based services, allowing healthcare providers to make informed choices that result in enhanced outcomes for individuals.’ CareSet’s integration of over 100 external data sources, including insights from more than 62 million beneficiaries and 6 million providers, underscores the critical role of data in improving individual support and outcomes.
Case studies, such as ‘PUTTING INDIVIDUALS FIRST: Unlocking Medicare Data to Empower HCP,’ illustrate the necessity of incorporating data and technology in value-based support. This approach facilitates the collection and analysis of individual information, leading to informed decision-making and improved coordination. For example, CareSet’s Medicare Data Analysis demonstrates how extensive data insights can address challenges faced by healthcare facilities, particularly in oncology treatment options like Qinlock for Gastrointestinal Stromal Tumor (GIST), ultimately enhancing wellness through targeted methodologies and processes.
Despite these advantages, healthcare facilities grapple with issues such as bureaucratic inefficiencies and rising operational costs, which can impede their overall effectiveness. Nevertheless, evidence suggests that while hospital systems have the potential for improved client support through integrated methods, they must remain adaptable and open to overcoming these ongoing challenges. The ongoing evolution of medical service delivery models, highlighted by a 154% increase in telehealth utilization in 2020, emphasizes the importance of flexibility in achieving optimal outcomes for individuals.
Assessing the Effectiveness of Traditional Healthcare Models
Conventional healthcare frameworks frequently highlight episodic treatment, leading to disjointed experiences for individuals. While these models may offer prompt access to services, they often lack the consistency of support that integrated approaches provide. Studies indicate that individuals in conventional environments frequently encounter extended wait periods and reduced coordination, negatively impacting health outcomes.
For instance, research shows that individuals receiving treatment in conventional models report lower satisfaction levels compared to those in integrated systems. A significant case study emphasizes that prioritizing the reduction of client wait times fosters a culture of respect and efficiency among service providers, resulting in higher customer satisfaction ratings, repeat visits, and stronger referrals. This enhancement elevates the healthcare organization’s reputation and underscores the importance of patient-focused services.
As Paula Saez notes, “Reducing Waiting Times to Improve Customer Satisfaction: A Hybrid Strategy for Decision Support Management,” emphasizes the critical role of wait time reduction in enhancing experiences. Although conventional models can excel in specialized care areas, where focused expertise can yield high-quality outcomes, they often struggle with coordination and comprehensive management of individuals.
The challenges inherent in conventional medical models necessitate a reassessment of approaches to enhance individual experiences and outcomes. Furthermore, leveraging comprehensive insights from CareSet’s monthly Medicare updates, which analyze drug utilization and treatment pathways for over 62 million beneficiaries and 6 million providers, can inform future healthcare reform initiatives aimed at improving market access and engagement strategies.
CareSet’s updates address essential business inquiries, such as which diseases providers diagnose and treat, and how individuals transition from diagnosis to treatment. Notably, CareSet identifies 15% more targets and 250% more individuals than top claims vendors, offering valuable data to refine pharmaceutical strategies.
Comparative Analysis: Hospital Systems vs. Traditional Healthcare Models
In comparing medical facilities and traditional healthcare models, several critical factors arise. Hospital systems generally provide a more unified strategy within healthcare networks, enhancing care coordination and resulting in better outcomes for individuals. By utilizing shared resources and sophisticated data analytics, such as those offered by CareSet, these systems can improve service delivery, leading to substantial cost savings and increased satisfaction for individuals. CareSet’s comprehensive Medicare data insights, derived from over 62 million beneficiaries and 6 million providers, empower healthcare stakeholders to navigate treatment pathways effectively, analyzing provider interventions through frameworks like ICD, NDC, and HCPCS codes.
For instance, providers employ:
- ICD codes to diagnose conditions
- NDC codes to identify medications
- HCPCS codes to define services
This facilitates a seamless experience from diagnosis to treatment. A case study on disease-based efficiency has demonstrated that focusing on uniform groups can reveal substantial variations in resource utilization and outcomes, underscoring the effectiveness of integrated support. CareSet’s analytics solutions have identified 15% more targets and uncovered 250% more individuals indicated for treatment, showcasing the power of data in enhancing targeting and provider insights.
In contrast, conventional healthcare models may provide faster access to specialized services but often lack the continuity and thorough treatment that hospital systems excel at. While conventional models can be more adaptable and reactive to urgent client needs, they may not effectively support value-driven initiatives that prioritize outcomes over service volume.
The advantages of unified approaches within hospital systems are clear, particularly in their capability to simplify patient experiences and reduce unnecessary expenses. Statistics suggest that integrated medical frameworks can achieve significant cost reductions compared to episodic treatment models, rendering them an attractive option for various medical situations. As noted by Wenke Hwang, PhD, “A thorough examination of the current literature that evaluates the connection between IDSs and cost/quality is urgently required,” emphasizing the importance of assessing integrated treatment models.
Ultimately, the choice between these models depends on specific individual requirements, medical goals, and the setting of service delivery, with hospital systems often proving to be the more beneficial option for long-term individual management. In summary, the integration of care within hospital systems enhances patient outcomes and provides a more efficient and cost-effective approach to service delivery, supported by advanced analytics from CareSet. For more insights on how CareSet can enhance your healthcare strategies, explore our analytics solutions today.
Conclusion
The comparison between hospital systems and traditional healthcare models reveals significant implications for patient care and operational efficiency. Hospital systems, with their integrated networks, foster improved care coordination, leading to better patient outcomes and higher satisfaction levels. The ability to leverage comprehensive data analytics, as demonstrated by CareSet, enhances the decision-making process and streamlines treatment pathways. This evidence proves that integrated care can effectively address the challenges of modern healthcare delivery.
In contrast, traditional healthcare models often struggle with fragmentation and lack of continuity, which can negatively impact patient experiences and outcomes. While they may provide immediate access to specialized services, the episodic nature of care in these models can result in longer wait times and lower satisfaction scores. This situation highlights the need for a reevaluation of strategies aimed at improving care delivery within these systems.
Ultimately, the effectiveness of hospital systems in delivering cohesive and patient-centered care underscores their growing importance in the healthcare landscape. As the sector continues to evolve, embracing integrated care models will be crucial for enhancing patient experiences, improving outcomes, and achieving greater operational efficiencies. The evidence strongly supports the notion that a shift towards hospital systems is not only beneficial but necessary for meeting the complex demands of today’s healthcare environment.


