Overview
The article emphasizes the critical importance of accurately calculating carboplatin doses in cancer treatment. It highlights the essential roles of pharmacokinetics, patient-specific factors, and the Calvert formula in achieving effective therapy.
A detailed step-by-step guide is provided for healthcare professionals to determine the appropriate dosage, addressing potential challenges such as renal impairment and documentation errors.
This approach not only ensures patient safety but also enhances treatment efficacy, reinforcing the necessity for precision in oncology dosing.
Introduction
In the realm of oncology, the precision of chemotherapy dosing can mean the difference between life and death. Carboplatin, a cornerstone treatment for various cancers, exemplifies this critical need for accuracy. Understanding its pharmacokinetics—how the drug is absorbed, distributed, metabolized, and excreted—plays a vital role in tailoring doses that maximize efficacy while minimizing toxicity.
As healthcare professionals navigate the complexities of patient-specific factors, from renal function to previous treatment histories, the importance of employing the Calvert formula becomes evident. This article delves into the intricacies of carboplatin dosing, offering insights into the key factors influencing calculations, step-by-step guidance for accurate dosing, and strategies to troubleshoot common challenges faced in clinical practice.
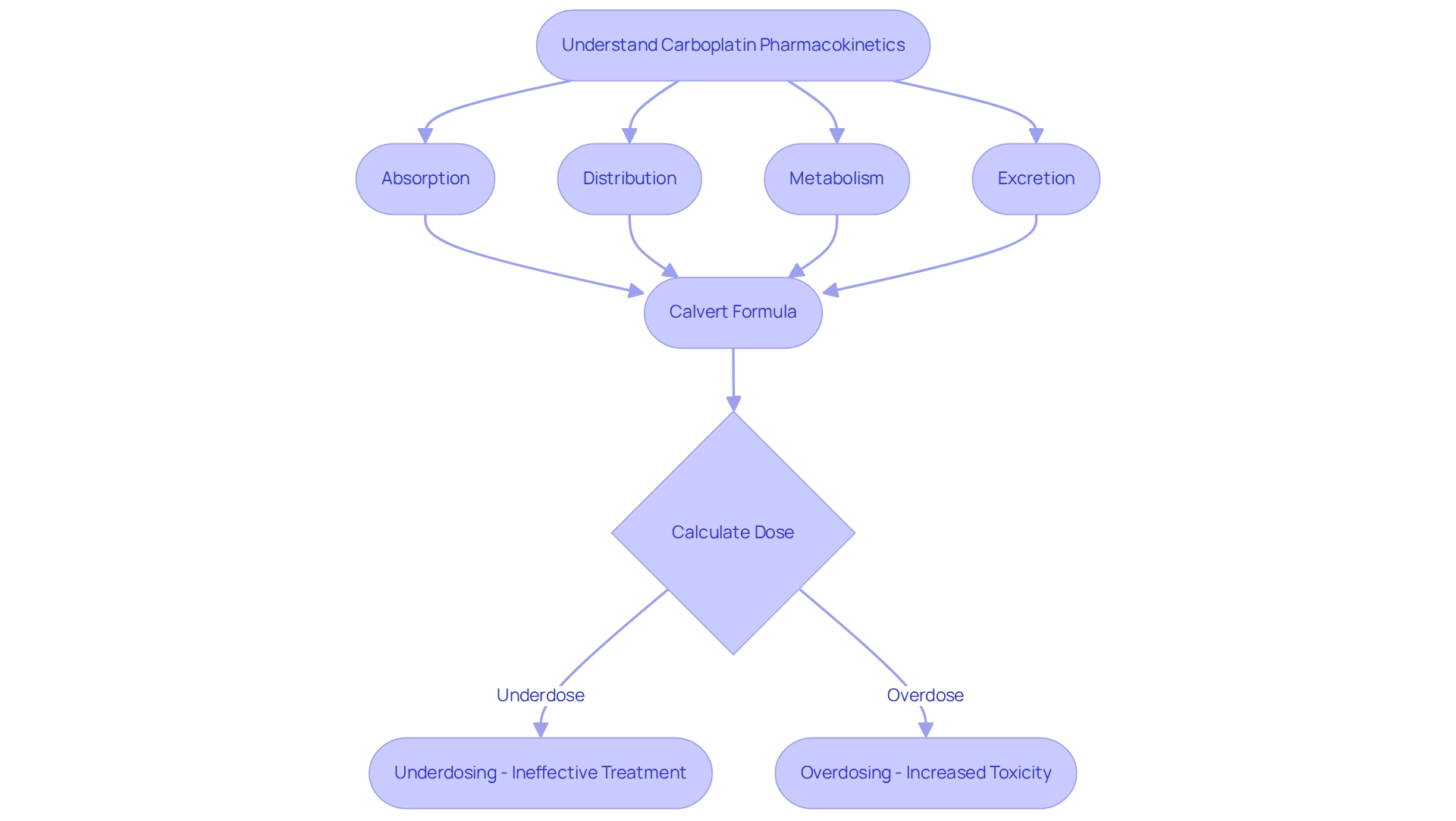
Understand Carboplatin Pharmacokinetics and Dosing Importance
Carboplatin is a chemotherapy drug primarily utilized in the treatment of various cancers, including ovarian and lung cancer. Understanding its pharmacokinetics—how the drug is absorbed, distributed, metabolized, and excreted in the body—is essential to calculate carboplatin dose for each patient.
The administration of this chemotherapy agent is often guided by the Calvert formula to calculate carboplatin dose, taking into account the area under the concentration-time curve (AUC) and the patient’s kidney function, specifically the glomerular filtration rate (GFR).
Accurate dosing is paramount; thus, it is crucial to calculate carboplatin dose properly, as both underdosing and overdosing can lead to ineffective treatment or increased toxicity, respectively.
Consequently, a comprehensive understanding of the drug’s pharmacokinetics is crucial for healthcare professionals involved in chemotherapy administration to accurately calculate carboplatin dose.
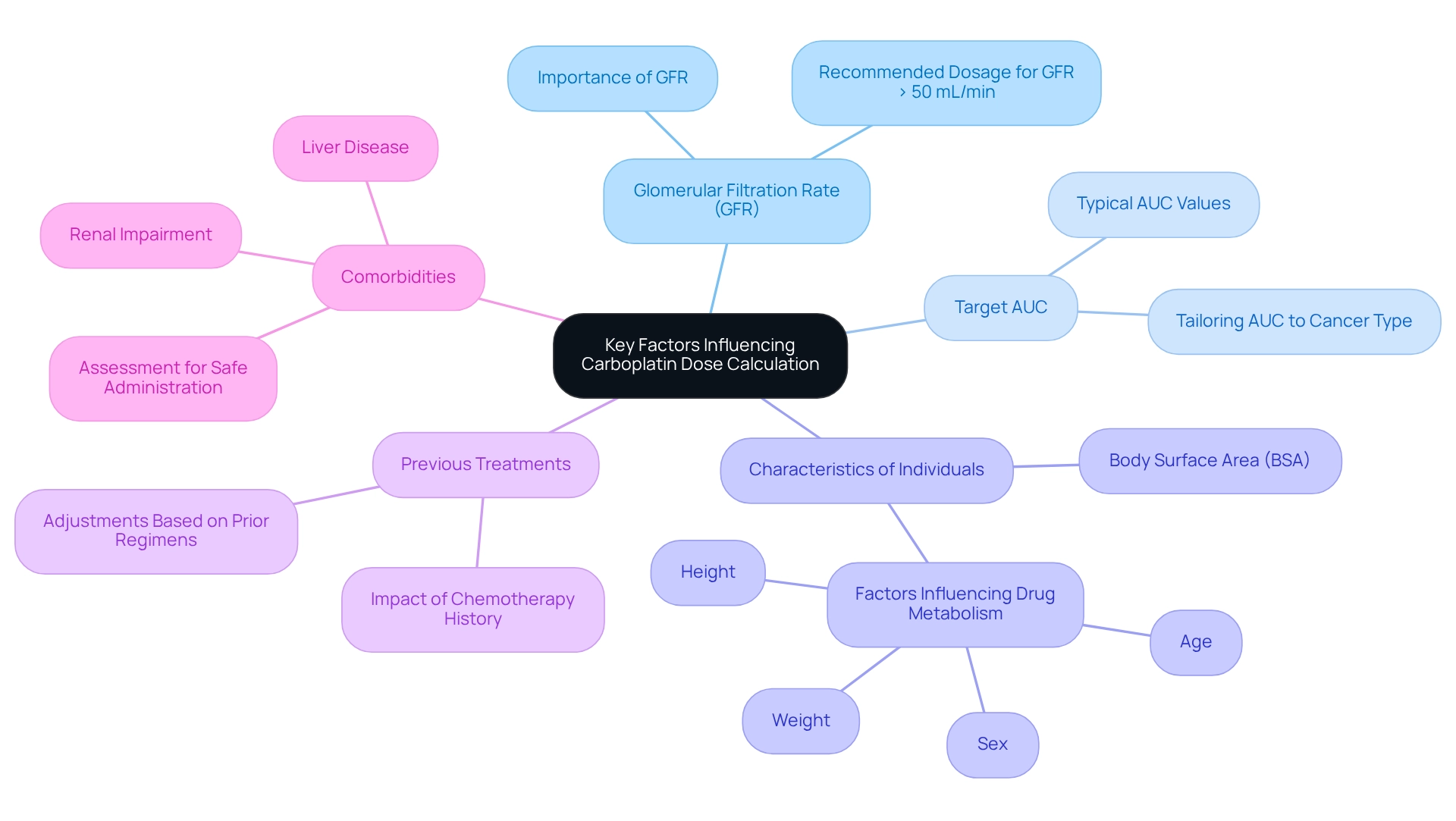
Identify Key Factors Influencing Carboplatin Dose Calculation
Several key factors significantly affect the ability to calculate carboplatin dose levels.
- Glomerular Filtration Rate (GFR) is a critical element in assessing how efficiently the kidneys eliminate the drug from the bloodstream. An elevated GFR signifies improved kidney performance, which might necessitate a larger dosage of the drug to achieve the intended therapeutic effect. Corine Ekhart from the Netherlands Cancer Institute recommends that when specific exposures to this drug are required, dosing should rely on the average population clearance for individuals with a GFR exceeding 50 mL/min.
- Target AUC: The target area under the curve (AUC) is tailored according to the specific cancer type and the individual’s overall health status. Typical AUC values for carboplatin range from 4 to 6 mg/mL/min, guiding clinicians in dose adjustments to optimize treatment outcomes.
- Characteristics of Individuals: Individual factors, including age, weight, height, and sex, can influence drug metabolism and clearance. Body surface area (BSA) is often utilized alongside GFR to determine suitable medication amounts, ensuring personalized treatment.
- Previous Treatments: A person’s history of chemotherapy can affect their response to a particular medication, necessitating careful consideration of prior regimens when determining the current dose. Adjustments may be required based on previous treatment outcomes and tolerability.
- Comorbidities: The presence of comorbid conditions, such as renal impairment or liver disease, can significantly alter drug clearance rates. These factors must be meticulously assessed to ensure safe and effective administration of the drug, minimizing the risk of adverse effects while maximizing therapeutic efficacy.
The original Calvert formula for the medication’s administration includes a constant of 25 mL/min to account for nonrenal clearance, which is vital to calculate carboplatin dose accurately. Understanding these elements is essential for enhancing medication management, ultimately improving treatment results for individuals with various types of cancers, including ovarian and small cell lung cancers. The Calvert formula exemplifies how customized strategies can enhance care and treatment success. Notably, this chemotherapy drug has played a crucial role in improving short-term survival rates for small cell lung cancer, underscoring the necessity of accurate dosing in achieving better outcomes for individuals.
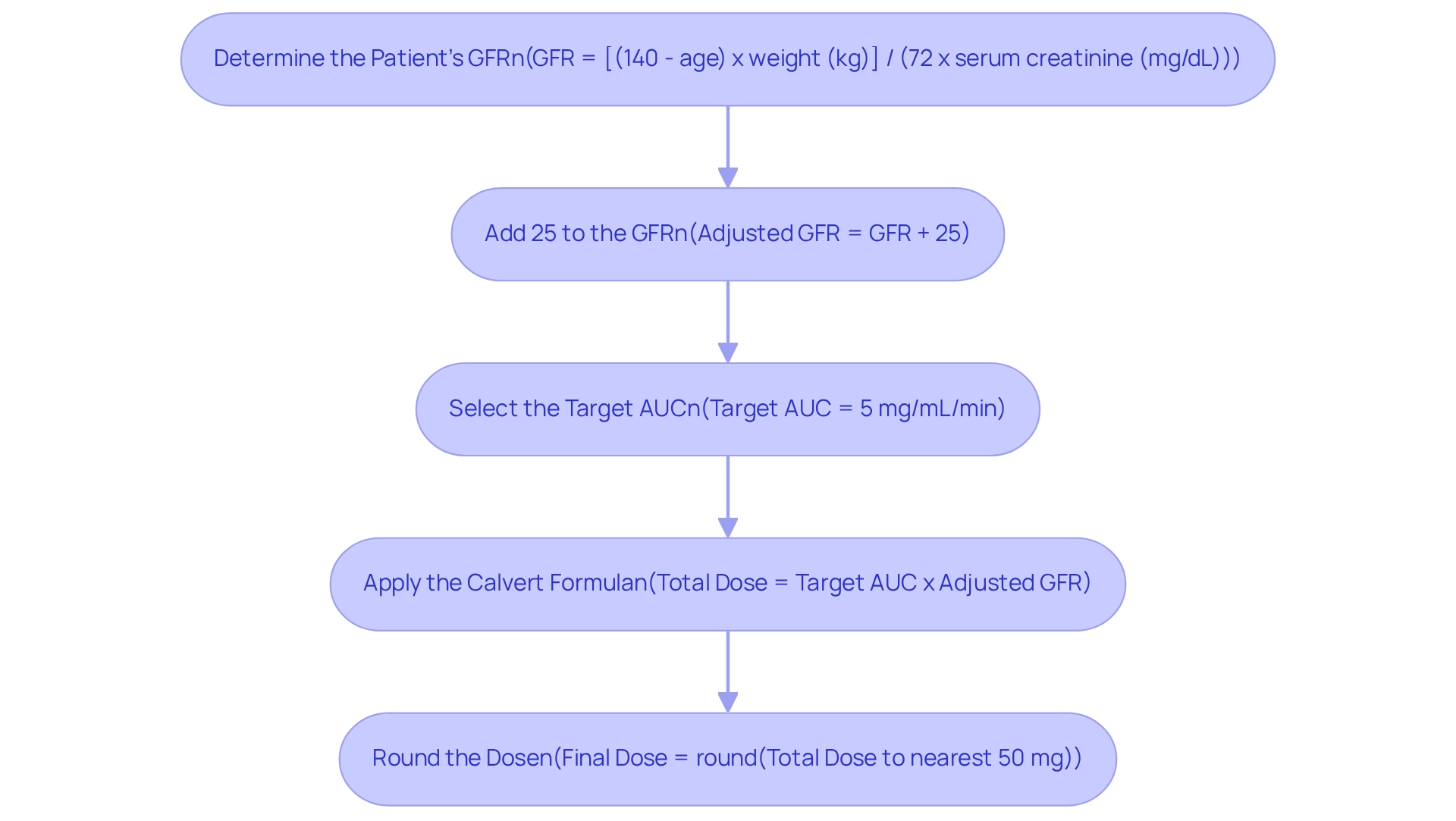
Follow Step-by-Step Instructions for Carboplatin Dose Calculation
To accurately calculate carboplatin dose, healthcare professionals should adhere to the following steps using the Calvert formula:
-
Determine the Patient’s GFR: Begin by utilizing a reliable method, such as the Cockcroft-Gault equation, to estimate the patient’s GFR. This estimation relies on the serum creatinine level, age, weight, and sex. For instance, for a 60-year-old male weighing 70 kg with a serum creatinine of 1.2 mg/dL, the GFR can be computed as follows:
GFR = [(140 - age) x weight (kg)] / (72 x serum creatinine (mg/dL))GFR = [(140 - 60) x 70] / (72 x 1.2) = 70.4 mL/min -
Add 25 to the GFR: This adjustment is critical as it accounts for the pharmacokinetics of the drug. Thus, the adjusted GFR becomes:
Adjusted GFR = 70.4 + 25 = 95.4 mL/min -
Select the Target AUC: Depending on the treatment protocol, it is essential to choose the appropriate AUC value, such as 5 mg/mL/min.
-
Apply the Calvert Formula: The total carboplatin dose can be calculated using the following formula:
- Total Dose (mg) = Target AUC x (Adjusted GFR)
- Therefore, Total Dose = 5 x 95.4 = 477 mg
-
Round the Dose: In accordance with clinical practice, round the calculated dose to the nearest 50 mg for administration, resulting in:
- Final Dose = 500 mg
By meticulously following these steps, healthcare providers can ensure precise dosing of carboplatin, thereby optimizing treatment efficacy while minimizing the risk of toxicity.
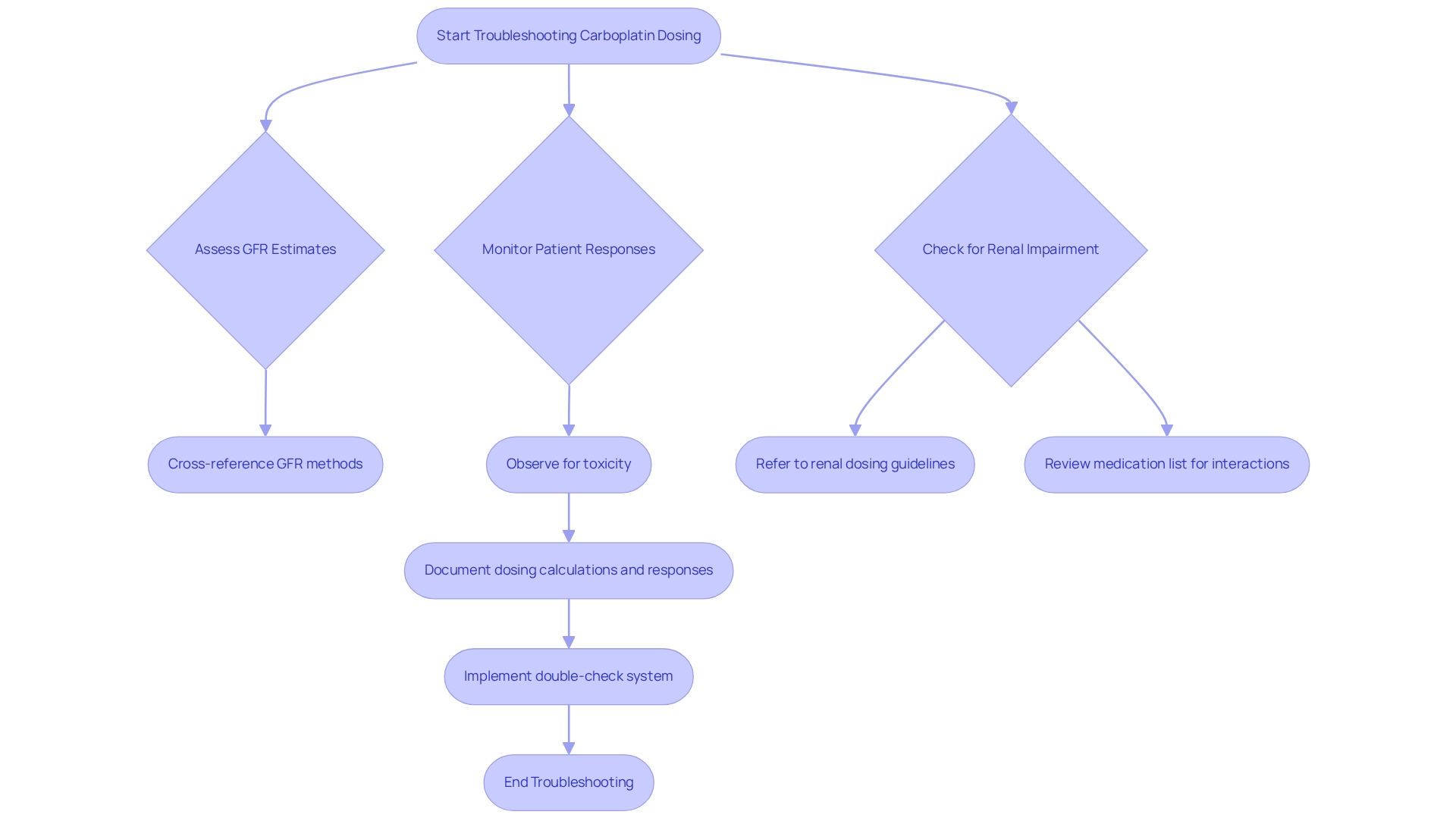
Troubleshoot Common Carboplatin Dosing Challenges
When healthcare providers calculate carboplatin dose, they may encounter several challenges that require careful consideration, as inaccurate GFR estimates can significantly impact dosing decisions. Variability in serum creatinine measurements often leads to incorrect GFR calculations. To mitigate this issue, it is advisable to employ multiple methods for estimating GFR and to cross-reference results for accuracy, especially when aiming to calculate carboplatin dose, as individual variability is another critical factor. Responses to carboplatin can differ markedly among individuals. It is essential to observe patients closely for signs of toxicity and adjust doses accordingly, based on their reactions and side effects.
Renal Impairment presents additional complexities. Patients with compromised kidney function may necessitate dose adjustments. Always refer to renal dosing guidelines and consider utilizing lower AUC targets for these individuals to calculate carboplatin dose safely, while also taking drug interactions into account. Be vigilant about other medications the patient is taking that may influence carboplatin metabolism. A thorough examination of the individual’s medication list, along with consulting drug interaction resources, is crucial.
Documentation Errors can lead to significant issues in treatment continuity. Ensure accurate documentation of dosing calculations and patient responses to prevent errors in future treatments. Implementing a double-check system, where another healthcare professional verifies the calculations before administration, is a prudent practice.
By proactively addressing these challenges, healthcare providers can significantly enhance the safety and effectiveness of carboplatin therapy.
Conclusion
The significance of precise carboplatin dosing is paramount in the intricate field of oncology. Understanding the pharmacokinetics of carboplatin—specifically, the essential factors that influence its dosing, such as:
- Glomerular filtration rate (GFR)
- Target AUC
- Patient characteristics
- Previous treatments
- Comorbidities
is crucial for optimizing treatment outcomes. The Calvert formula emerges as a vital tool in this context, enabling healthcare professionals to customize doses according to individual patient needs, thereby maximizing efficacy while minimizing the risk of toxicity.
Adopting a systematic approach to dose calculation not only ensures accuracy but also empowers providers to navigate the inherent challenges of chemotherapy administration. By addressing potential obstacles, including:
- Inaccurate GFR estimates
- Patient variability
- Renal impairment
healthcare professionals can enhance both the safety and effectiveness of carboplatin therapy. This diligence in dosing strategy ultimately contributes to improved survival rates and quality of life for patients battling various forms of cancer.
In conclusion, the meticulous consideration of pharmacokinetics and personalized dosing strategies is essential in administering carboplatin. As the oncology landscape continues to evolve, the commitment to precision in chemotherapy dosing will remain a cornerstone of effective cancer treatment, underscoring the profound impact healthcare providers can have on patient outcomes.

