Overview
The article delineates nine robust strategies aimed at enhancing operational health within healthcare settings. These strategies encompass critical areas such as:
- Data analytics
- Lean management
- Employee training
- Patient feedback systems
Each approach is underpinned by compelling evidence demonstrating its effectiveness in improving care quality, optimizing resource allocation, and nurturing a culture of continuous improvement. Ultimately, these initiatives lead to superior health outcomes and heightened operational efficiency in medical organizations.
Introduction
In the rapidly evolving landscape of healthcare, organizations are increasingly adopting data-driven strategies to enhance operational efficiency and improve patient outcomes. The significance of leveraging comprehensive Medicare data cannot be overstated; it serves as a cornerstone for informed decision-making. By integrating innovative management methodologies such as Lean and Six Sigma, healthcare providers can focus on continuous improvement, which is paramount in today’s challenging environment.
Facing unprecedented challenges, including rising inpatient admissions and the pressing need for effective care coordination, the integration of advanced analytics and employee training becomes crucial. This article explores various approaches that healthcare providers can implement, showcasing how data insights and operational strategies can transform service delivery and foster a culture of excellence in patient care.
CareSet: Leverage Comprehensive Medicare Data for Operational Insights
CareSet excels in extracting and interpreting Medicare claims information, which empowers healthcare entities to enhance their operations health and derive critical operational insights. By examining over $1.1 trillion in yearly claims information, CareSet reveals treatment trends, provider networks, and individual demographics, enabling informed decision-making that improves both care quality and operations health.
The recognition of data deficiencies and the mapping of healthcare journeys enable entities to enhance their services, leading to substantial advancements in outcomes for individuals, especially as the influence of Medicare data on operations health becomes more evident than ever in 2025. Inpatient admissions have increased almost 19% compared to 2022 levels as of February 2024. This surge highlights the necessity for medical organizations to rethink their strategies for effectively managing total care costs.
Experts emphasize the importance of operations health by distinguishing between care coordination and case management roles to optimize patient engagement and resource allocation. Kelsey Waddill, managing editor of Healthcare Payers, underscores the implications of Medicaid per capita caps, which further complicate the environment for medical providers.
Recent case studies demonstrate how CareSet’s information analysis has enabled oncology treatment manufacturers to connect more effectively with medical practitioners regarding late-stage therapy options, such as Qinlock for Gastrointestinal Stromal Tumor (GIST). This engagement is essential as existing entities face challenges in the competitive Medicaid landscape, where they are losing contracts in the 2025 bidding process.
Payers like Anthem and Aetna are compelled to innovate beyond cost considerations, presenting opportunities for Dual-Eligible Special Needs Plans (D-SNPs) to enhance care integration for low-income individuals eligible for both Medicare and Medicaid. CareSet’s information analysis plays a crucial role in assisting entities to navigate these challenges by offering insights that enhance care coordination and operations health strategies.
Additionally, CareSet’s information analysis addresses immediate operations health requirements while promoting long-term strategic growth for medical partners. By utilizing extensive Medicare insights from more than 62 million beneficiaries and 6 million providers, organizations can navigate the complexities of the medical landscape, ultimately enhancing patient outcomes and optimizing the lifecycle management of pharmaceutical products.
Furthermore, CareSet’s innovative data science products are designed to assist drug launches, offering actionable insights that improve interaction with medical providers and streamline operational processes.
Lean Management: Streamline Processes to Enhance Efficiency
Lean management is a systematic methodology designed to identify and eliminate waste within medical processes, ultimately enhancing operations health. By prioritizing value from the individual’s viewpoint, medical organizations can enhance operations health, reduce wait times, and improve overall service provision. Techniques such as value stream mapping and continuous flow are crucial in optimizing care processes, ensuring that resources are utilized effectively and that needs are addressed promptly.
In 2025, the impact of lean management on medical operational efficiency is underscored by the potential for a 200% return on investment (ROI). This statistic highlights the financial advantages of adopting lean practices, which not only improve outcomes for individuals but also contribute to the sustainability of medical institutions.
Integrating CareSet’s comprehensive Medicare data insights can further enhance these lean management strategies. By leveraging insights from over 62 million beneficiaries and 6 million providers, medical organizations can make informed decisions that align with lean principles, ensuring that patient care processes are both efficient and effective.
Case studies illustrate the effectiveness of lean management strategies in the medical field. For example, Intel’s ‘Copy Exactly!’ methodology, which standardized manufacturing processes across all facilities, achieved an impressive 99.999% reliability in microprocessor production. This level of consistency serves as a benchmark for medical operations health, where similar standardization can lead to enhanced quality and efficiency.
Current best practices in lean management emphasize the development of metrics that drive the right behaviors and reflect true value creation from the customer’s perspective. This approach is essential for lean success, as it aligns operational goals with client satisfaction and outcomes. As Sunny T., a Group CI Practitioner, states, “We need to separate the approach versus the tools,” underscoring the importance of focusing on strategic growth rather than merely the methodologies employed.
To effectively implement lean management strategies, medical facilities should consider actionable steps such as utilizing CareSet’s data insights to identify areas of waste and streamline processes. By concentrating on strategic growth and operational excellence, medical organizations can foster long-term advancements that benefit both patients and providers. Overall, the implementation of lean management strategies in medical services not only addresses immediate inefficiencies but also contributes to operations health and lays the groundwork for sustainable operational success.
Six Sigma: Minimize Errors and Improve Quality Control
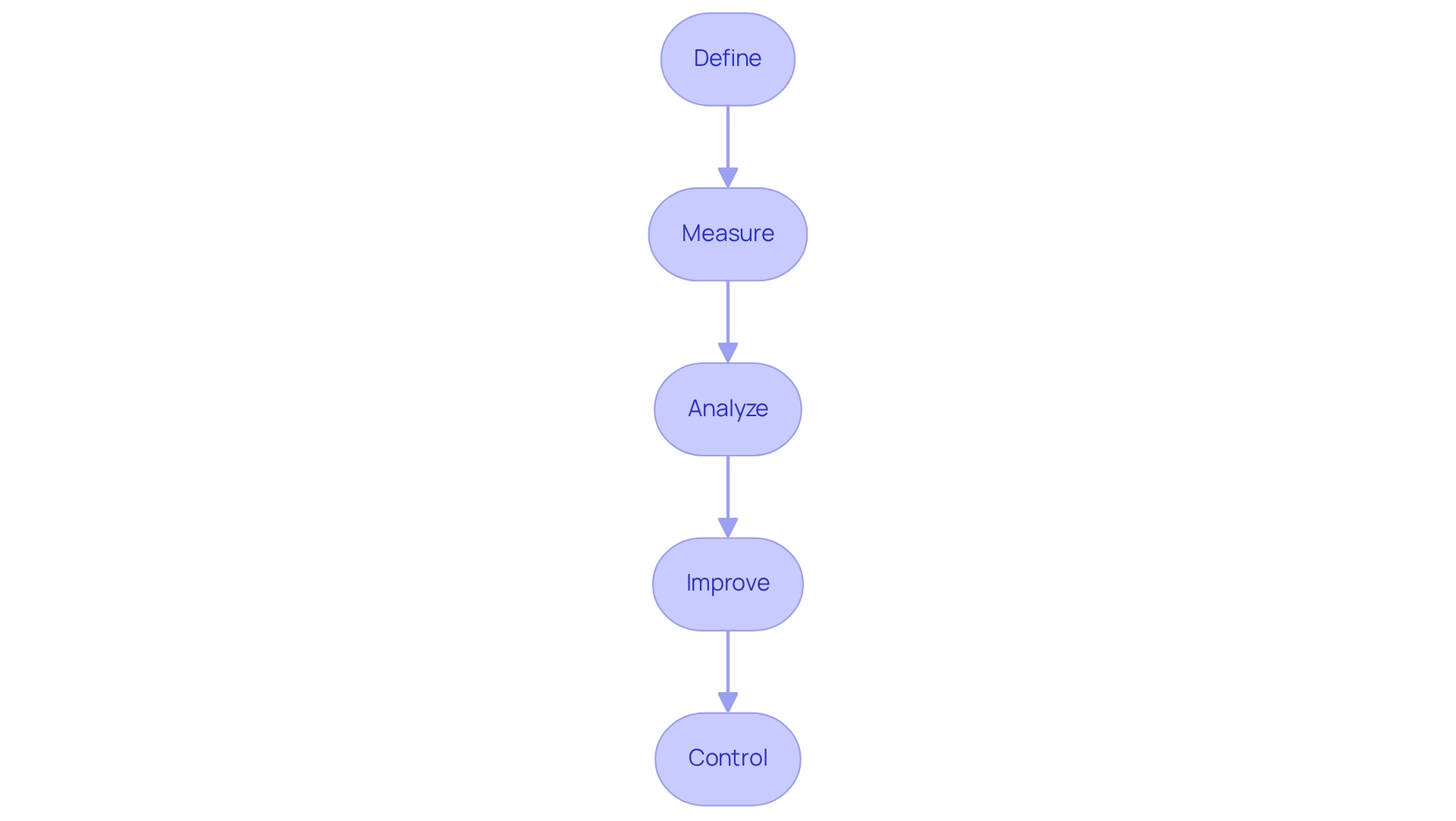
Six Sigma represents a data-driven methodology aimed at minimizing errors and enhancing quality control to improve operations health within the medical field. By leveraging statistical methods and quality management tools, organizations can improve operations health by pinpointing defects in processes and implementing effective solutions to elevate care standards.
The integration of extensive Medicare data insights from CareSet significantly empowers stakeholders in healthcare by providing crucial information regarding treatment pathways and provider interventions. Understanding the transitions individuals experience from diagnosis to treatment across Medicare A, B, and D benefits is essential for improving operations health in care delivery.
Furthermore, the application of the DMAIC (Define, Measure, Analyze, Improve, Control) framework enables service providers to systematically tackle issues, resulting in improved outcomes and enhanced operations health along with reduced operational costs.
CareSet’s monthly Medicare updates further enhance provider engagement by delivering insights into drug utilization, treatment approvals, and the specific relationships among HCPCS, ICD, DRGs, and NCDs within therapeutic areas, ultimately supporting the overarching goal of delivering high-quality care.
Telehealth Solutions: Enhance Patient Access and Operational Efficiency
Telehealth solutions are revolutionizing healthcare by facilitating remote consultations, particularly for individuals in underserved regions. This technology not only enhances access to medical services but also substantially reduces overhead costs associated with traditional in-person appointments. By streamlining operations health, telehealth improves flow management, which is vital for optimizing health outcomes and increasing satisfaction.
In 2025, the adoption of telehealth is projected to surge dramatically, with the market potentially expanding from $3 billion to an astonishing $250 billion. This significant shift highlights the urgent need for healthcare systems to act decisively in developing capabilities that provide high-quality care. Notably, 63% of individuals express interest in expanded digital health solutions, indicating a robust demand for telehealth services.
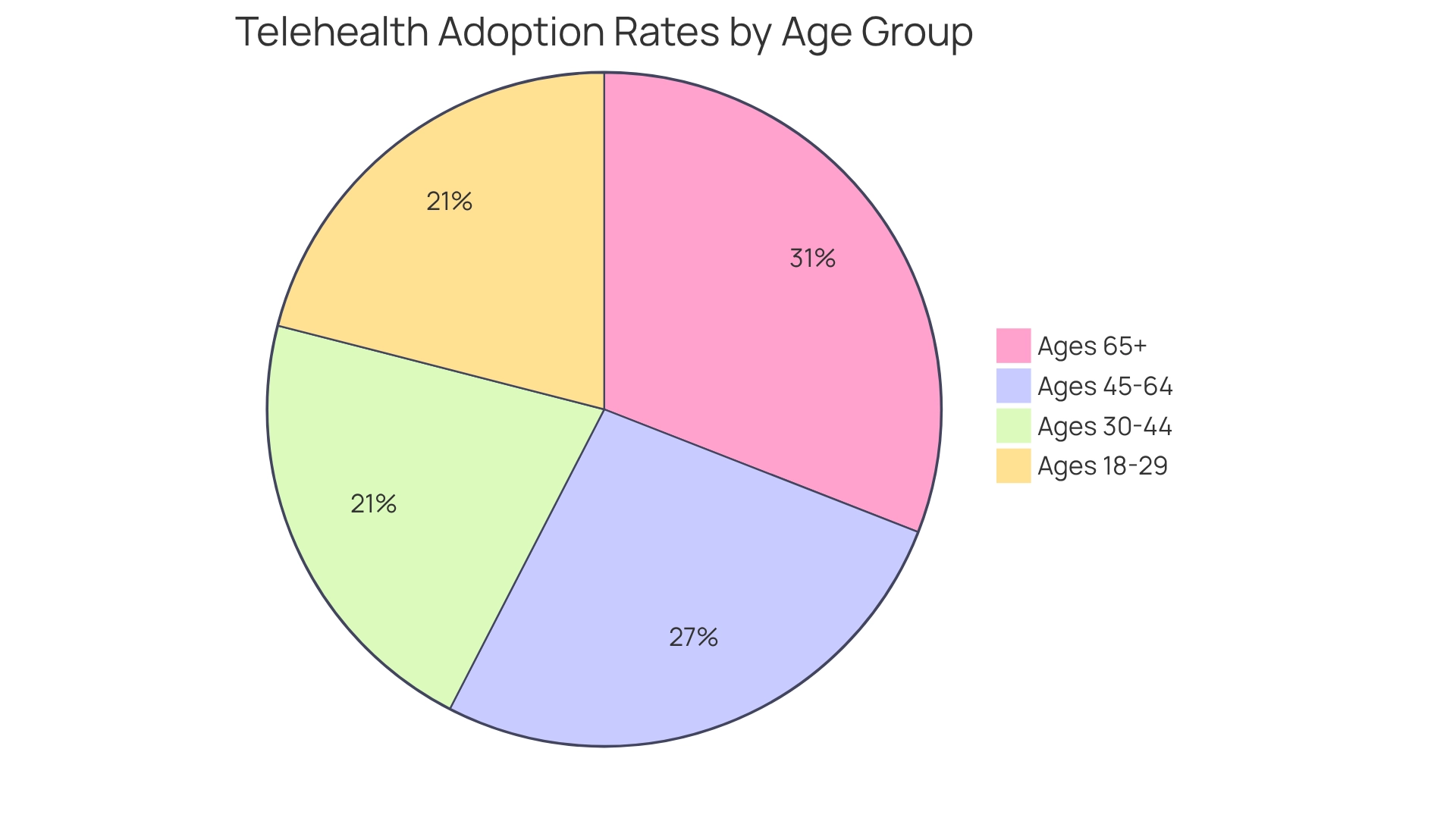
A recent study reveals that telemedicine usage varies by age, with adoption rates beginning at 29.4% among adults aged 18–29 and peaking at 43.3% for those aged 65 and older. This trend underscores the growing acceptance of telehealth across all age groups, especially among older adults who are increasingly embracing these services for their convenience and accessibility. The differing adoption rates also suggest that tailoring telehealth solutions to cater to various age demographics can further enhance operational efficiency and access for individuals.
Leveraging CareSet’s extensive Medicare data insights can empower stakeholders in the medical field to gain a deeper understanding of individual demographics and preferences, enabling them to customize telehealth services effectively. Expert insights indicate that the actual opportunity for telehealth is likely to be even more significant as stakeholders integrate it into standard practice. As noted by McKinsey, a leading global management consulting firm, “The actual opportunity is likely greater once stakeholders embed telehealth as the new normal.” This perspective reinforces the notion that telehealth is not merely a temporary solution but represents a profound transformation in the delivery of medical services.
Ultimately, the benefits of telehealth solutions extend beyond mere convenience; they play a crucial role in enhancing operations health and improving access for individuals, which ultimately leads to better health outcomes and a more effective medical system. By utilizing CareSet’s data insights, medical providers can refine their telehealth strategies to ensure they meet the evolving needs of the individuals they serve.
Employee Training: Equip Staff for Operational Excellence
Effective employee training programs are essential for cultivating a culture of operations health in the medical field. By investing in ongoing education and skills enhancement, entities can significantly improve service provision and care outcomes. Training initiatives should encompass critical areas such as compliance, client interaction, and technology utilization, ensuring that staff are well-equipped to navigate the evolving demands of the medical environment.
Statistics reveal that over 90% of employees affirm that the right kind of workplace training positively impacts their job engagement, underscoring the importance of tailored training programs. Moreover, organizations prioritizing employee training experience a 47% increase in workforce engagement, which directly correlates with improved patient care quality.
A recent case study titled ‘Training Goals and Employee Experience’ reinforces this notion, indicating that 92% of professionals in the medical field agree that aligning training goals with a positive employee experience fosters inclusivity and engagement. This alignment not only enhances operational efficiency but also contributes to a more motivated workforce.
Best practices for healthcare staff training in 2025 include:
- Developing comprehensive training modules that address both technical skills and soft skills, such as communication and empathy.
- Incorporating feedback mechanisms to refine training programs to better meet the needs of both staff and patients.
- Understanding how workers learn, as it lays the foundation for effective training programs that promote operations health and achieve operational excellence.
Healthcare leaders assert that a well-structured training program is foundational to operations health and operational excellence. As one expert noted, “Training is not just an expense; it’s an investment in our most valuable asset—our people.” Notably, training expenses in the US decreased by 3.7% to $98 billion in 2024, highlighting the necessity for companies to reevaluate their investment in training. By prioritizing employee training, medical organizations can ensure they are prepared to deliver high-quality care in an increasingly complex environment.
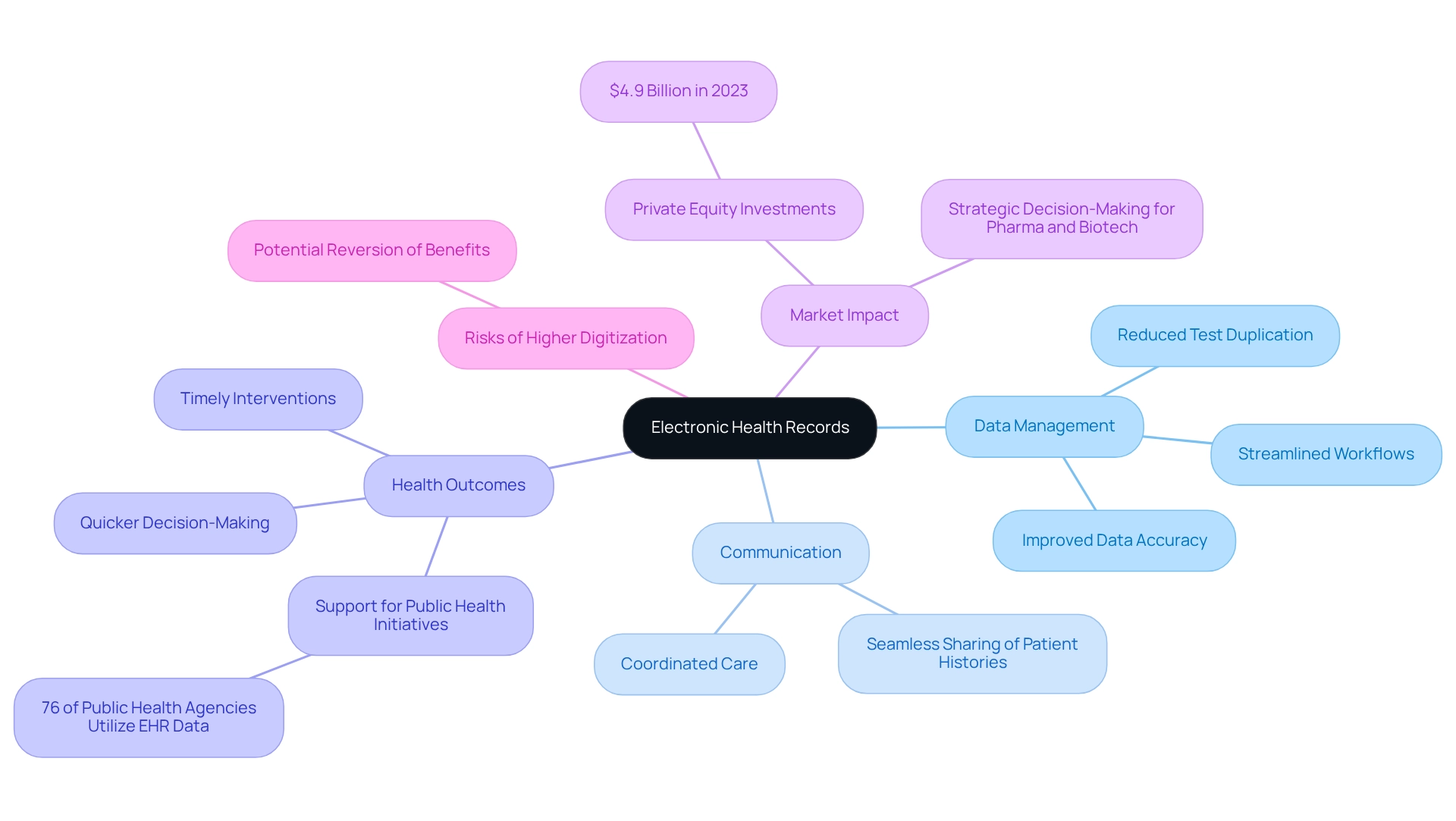
Electronic Health Records: Streamline Patient Data Management
Electronic Health Records (EHRs) play a pivotal role in enhancing information management within medical systems, particularly concerning Medicare. By digitizing client information, EHRs significantly improve data accuracy and reduce test duplication, which streamlines workflows and minimizes costs. Notably, by 2025, EHR implementation is projected to decrease the time required to access individual information by up to 80%, enabling quicker and more informed decision-making.
Furthermore, EHRs foster improved communication among healthcare providers, facilitating seamless sharing of patient histories and treatment plans. This interconnectedness is vital for coordinated care, which correlates with better outcomes for individuals. For instance, a study revealed that 76% of public health organizations utilize EHR information to monitor and manage health outbreaks, underscoring EHRs’ essential role in public health initiatives and emergency responses. The benefits of EHRs extend beyond operational efficiency; they also contribute to enhanced health outcomes. By providing real-time access to information, EHRs empower medical professionals to make timely interventions, ultimately improving the quality of care delivered.
Additionally, EHRs can integrate insights from CareSet’s extensive Medicare data, enabling stakeholders in the medical field to analyze provider interventions and individual patient journeys through ICD, NDC, and HCPCS frameworks. This integration supports strategic decision-making for pharmaceutical and biotech firms, enhancing their market access strategies.
Significantly, private equity investments in EHR companies reached $4.9 billion in 2023, highlighting the financial backing and importance of EHRs in the healthcare sector. However, it is crucial to recognize that higher levels of digitization may be associated with increased risks that could potentially reverse these benefits. As the medical landscape continues to evolve, the adoption of EHRs remains a cornerstone for effective client data management and operations health, particularly in navigating Medicare treatment pathways.
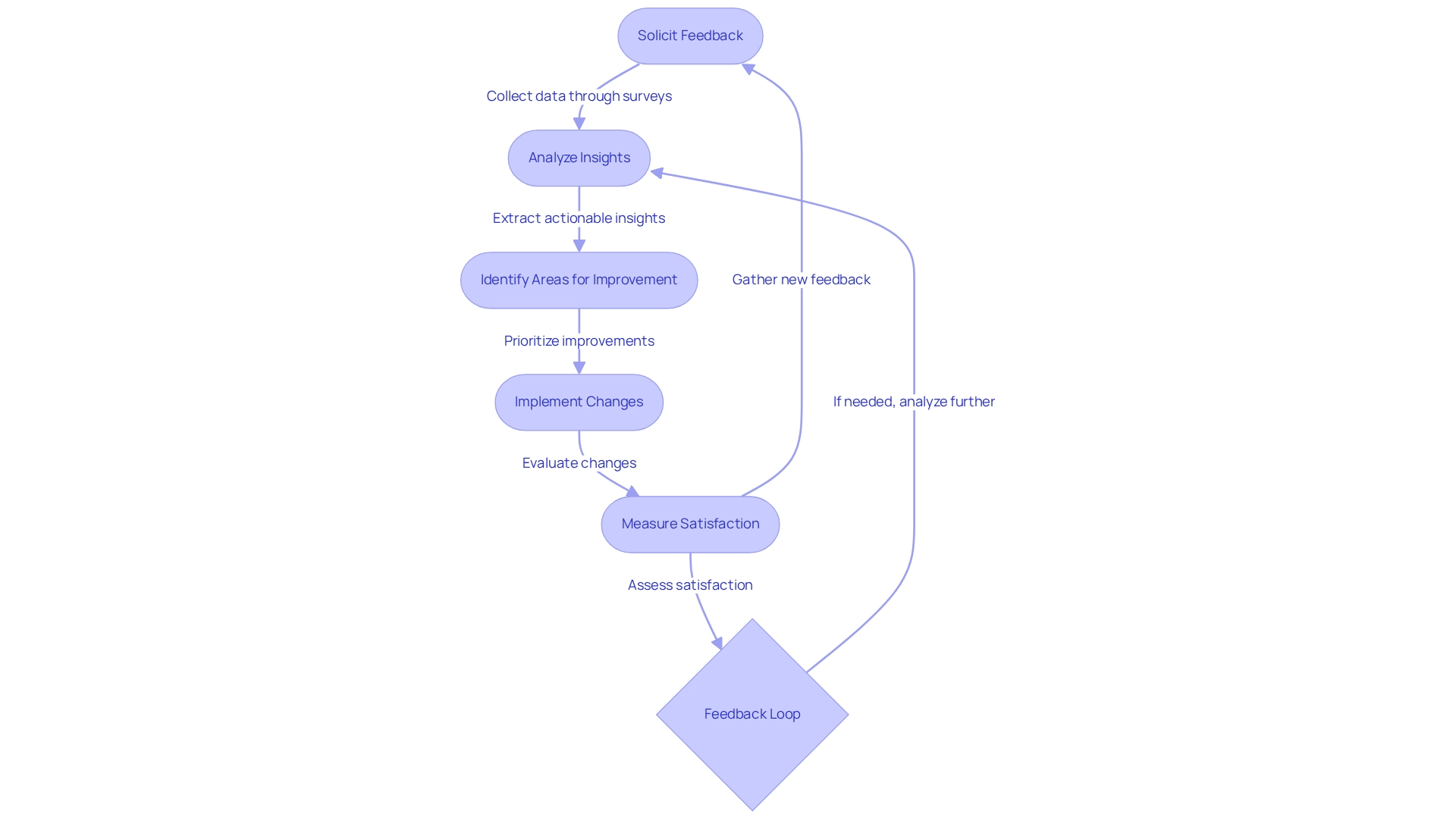
Patient Feedback Systems: Gather Insights for Continuous Improvement
Patient feedback systems are indispensable for acquiring insights that drive continuous enhancement in medical services. By actively soliciting input through surveys and various methods, organizations can pinpoint areas needing improvement and swiftly address client concerns. This proactive strategy not only elevates satisfaction among individuals but also cultivates a culture of accountability and responsiveness within medical teams, demonstrating that in 2025, the emphasis on engagement technology has shown that organizations employing these systems can significantly enhance operations health.
For instance, the NHS England initiative, which trialed Always Events, found that 85% of participating entities noted enhancements in specific aspects of user experience. This underscores how structured feedback can yield measurable improvements in service delivery.
Expert opinions underscore the significance of feedback systems from users. James Merlino, Chief Clinical Transformation Officer at Cleveland Clinic, asserts that prioritizing consumer experience is crucial for organizational success in today’s competitive healthcare landscape. He points out that organizations effectively leveraging client feedback systems have seen a 30% increase in satisfaction scores, highlighting the tangible benefits of these initiatives. Furthermore, adapting feedback collection methods to meet evolving client needs is vital for medical organizations aiming to remain relevant and efficient.
Concrete examples illustrate the impact of client feedback on service enhancement. A notable case involves a medical institution that implemented a feedback system, resulting in considerable improvements in care processes and a 25% increase in overall satisfaction scores within six months. Data indicates that healthcare organizations that prioritize operations health by actively engaging with client feedback systems experience significant advancements in service quality and operational efficiency. As we progress further into 2025, the importance of these systems cannot be overstated; they are not merely tools for gathering insights but are essential for fostering a culture of continuous improvement and excellence in patient care.
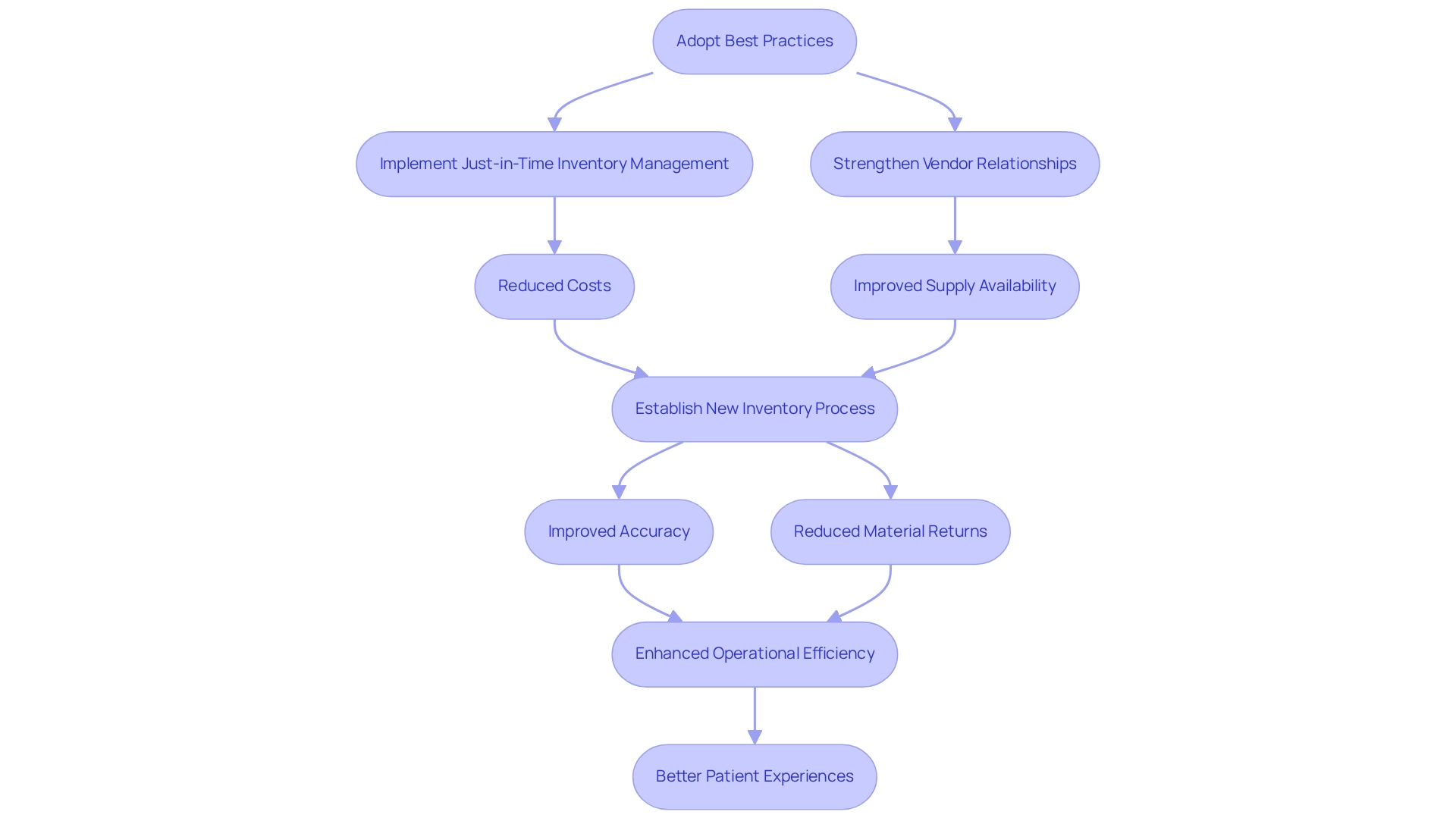
Supply Chain Management: Optimize Resources and Reduce Costs
Operations health in the medical field is crucial for the strategic coordination of resources, information, and finances, aimed at optimizing service delivery. By adopting best practices such as just-in-time inventory management and strong vendor relationship management, medical facilities can significantly lower expenses while ensuring that essential supplies are readily available. A recent case study on optimizing inventory management in operating rooms revealed that the establishment of a new process for updating preference cards and redefining inventory stock usage led to improved accuracy and reduced material returns, enhancing overall operational efficiency. An anesthesiologist involved in this project noted, “It has been such an educational process for me to work with the Renoir consulting group,” highlighting the collaborative effort that contributed to these improvements.
In 2025, the effect of supply chain optimization on medical expenses is becoming more apparent, with organizations reporting a 56% decrease in throughput time for individuals as a direct result of streamlined processes. Expert insights emphasize that ongoing performance improvement teams are vital for sustaining these enhancements, ensuring that systems and processes evolve to meet changing demands. These teams play a crucial role in driving continuous improvements, which are essential for adapting to the dynamic medical environment.
Furthermore, statistics show that effective supply chain strategies not only improve operational efficiency but also lead to better care outcomes. By concentrating on optimal methods in medical supply chain management, entities can enhance operations health while maneuvering through the intricacies of resource distribution, ultimately resulting in improved patient experiences and results.
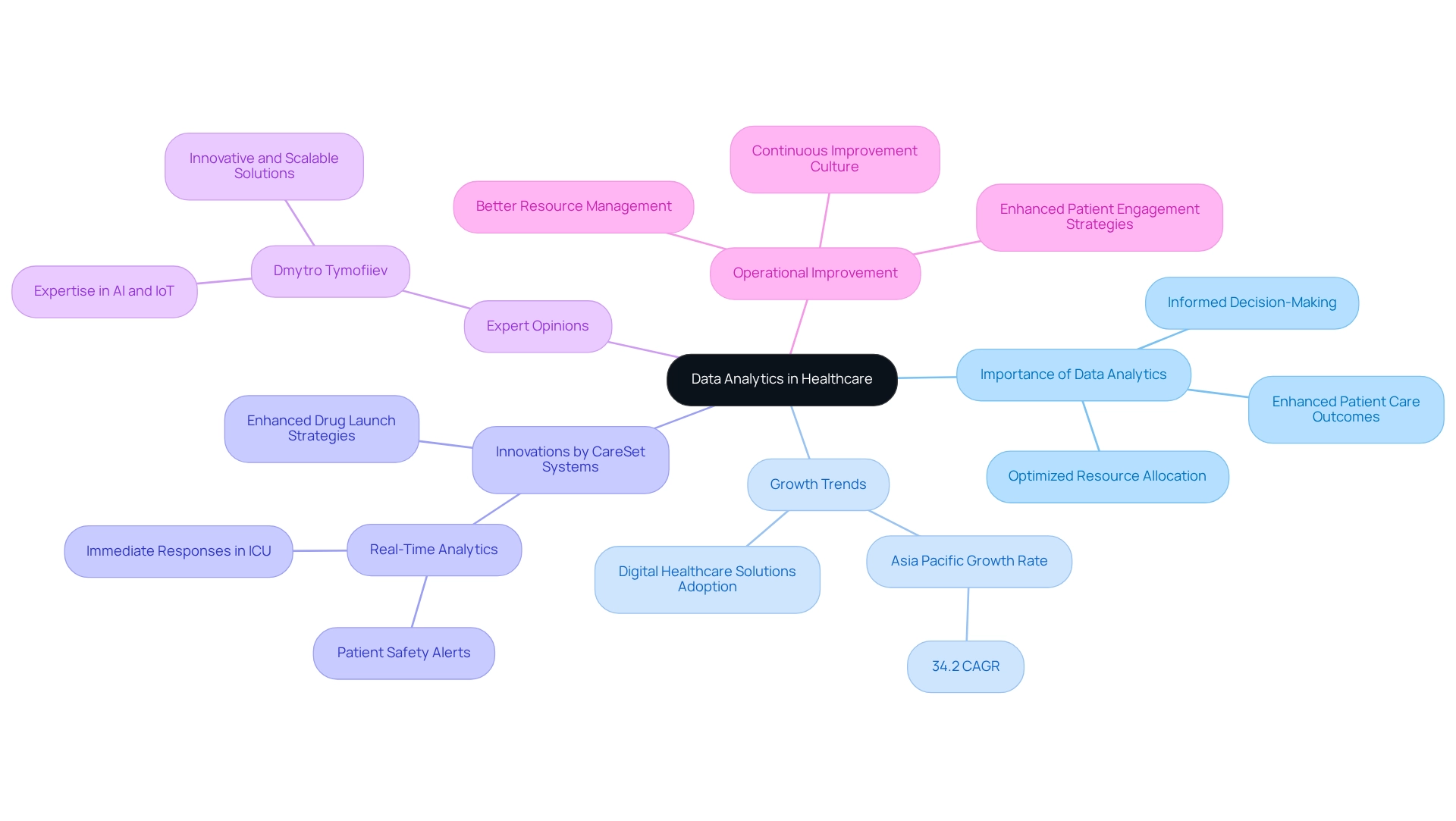
Data Analytics: Make Informed Decisions for Operational Improvement
Data analytics is crucial in the medical field, empowering organizations to sift through extensive datasets and extract actionable insights. By leveraging advanced analytics techniques, medical providers can discern trends, anticipate demand, and optimize resource allocation. This data-centric approach not only facilitates informed decision-making but also significantly enhances operations health and patient care outcomes.
In 2025, the influence of information analysis on medical decision-making is underscored by an anticipated growth rate of 34.2% in the Asia Pacific region, mirroring the wider trend in medical analytics propelled by the uptake of digital medical solutions. CareSet Systems has been leading this movement, introducing innovative analytical products aimed at enhancing drug launch strategies and improving healthcare insights. These products encompass features like real-time analytics, which processes information as it is produced to facilitate prompt reactions in crucial circumstances, such as monitoring individuals in an ICU. This capability enhances safety by alerting medical staff when an individual’s condition deteriorates, as demonstrated in the case study titled ‘Real-Time Analytics for Immediate Insights,’ showcasing the tangible benefits of analytics in operational settings.
Current trends indicate a strong emphasis on large information sets in healthcare, highlighting the analysis and utilization of emerging technologies to enhance industry practices. As organizations increasingly depend on analytics, they can anticipate enhancements in operations health, with statistics showing that effective utilization of information leads to better resource management and patient engagement strategies. CareSet’s leadership in sharing crucial information, such as COVID-19 hospital capacity details, further exemplifies their commitment to enhancing community understanding through information leadership.
Expert opinions emphasize the transformative role of information analysis in medical decision-making. Dmytro Tymofiiev, Delivery Manager at SPD Technology, notes, “Our experts have profound, cross-industrial expertise in Artificial intelligence and the Internet of Things, allowing us to develop innovative and scalable solutions from the ground up.” This integration of advanced analytics not only streamlines operations health but also fosters a culture of continuous improvement. By utilizing the strength of data, medical entities can make strategic choices that improve service delivery and enhance outcomes for individuals.
Culture of Continuous Improvement: Foster Ongoing Evaluation and Enhancement
Promoting a culture of ongoing enhancement within medical institutions is vital for improving operations health and the quality of care. This involves actively encouraging all staff members to engage in evaluating and refining processes. Regular training sessions, structured feedback mechanisms, and recognition programs for innovative ideas significantly contribute to this culture. By prioritizing ongoing enhancement, entities can more effectively adjust to the changing medical environment and consistently raise the standard of care provided to individuals.
Healthcare leaders emphasize the importance of ongoing evaluation. For instance, Matt Pollard, MD, MBOE, Vice President of Continuous Improvement at Intermountain Healthcare, acknowledges the potential for further enhancements, stating, “We have a long way to go here at Intermountain Healthcare, so many opportunities to improve, but we’re excited about what we have established thus far.” This sentiment reflects a broader recognition within the industry that continuous improvement is not just beneficial but necessary for sustaining high-quality care.
Moreover, case studies illustrate how effective change management can amplify continuous improvement strategies. The case study named ‘Putting Patients First’ demonstrates how CareSet’s extensive Medicare information insights enable medical providers to interact constructively with treatment choices, particularly enhancing prompt involvement with doctors concerning the 4th line of therapy for Gastrointestinal Stromal Tumor (GIST). By employing information from more than 62 million beneficiaries and 6 million providers, entities can improve their operations health by aligning their operational strategies with patient needs, ultimately enhancing care delivery.
Statistics suggest that organizations emphasizing operations health by fostering a culture of continuous improvement experience substantial advantages in quality of care. CareSet integrates more than 100 external data sources for comprehensive insights, demonstrating how data-driven approaches can enhance operational outcomes. Highlighting staff involvement in process assessment is expected to result in improved operations health, showing that when workers participate in enhancement efforts, the overall efficiency of service delivery rises. Ultimately, creating a culture of continuous improvement is vital for healthcare organizations aiming to thrive in a dynamic environment while ensuring the highest standards of patient care.
Conclusion
In the face of an ever-evolving healthcare landscape, the integration of data-driven strategies is not just beneficial but essential for enhancing operational efficiency and improving patient outcomes. By leveraging comprehensive Medicare data, healthcare organizations can uncover critical insights that inform decision-making and streamline processes. This article highlights how methodologies such as Lean and Six Sigma, alongside innovative solutions like telehealth and robust employee training programs, can drive continuous improvement and operational excellence.
As organizations grapple with rising inpatient admissions and the complexities of care coordination, it becomes increasingly clear that a multifaceted approach is necessary. By utilizing advanced analytics and fostering a culture of continuous improvement, healthcare providers can address immediate challenges while positioning themselves for long-term success. The emphasis on optimizing resources, enhancing patient engagement, and prioritizing employee training underscores the importance of a holistic strategy in navigating the complexities of today’s healthcare environment.
Ultimately, the commitment to leveraging data insights and operational strategies will pave the way for a more efficient, effective, and patient-centered healthcare system. By embracing these practices, organizations can ensure that they not only meet the demands of the present but also thrive in the future, delivering high-quality care that benefits both patients and providers alike.


