Overview
The article titled “9 Strategies for Success in Academic Medical Centers” identifies effective approaches that academic medical centers can adopt to enhance operational efficiency and patient care outcomes. It underscores the significance of:
- Leveraging data analytics
- Fostering collaboration with healthcare providers
- Adapting financial strategies
- Prioritizing patient-centered care
These elements are crucial for the success and sustainability of these institutions within a complex healthcare landscape, prompting further exploration of how they can be effectively implemented.
Introduction
In the rapidly evolving landscape of healthcare, academic medical centers (AMCs) confront a multitude of challenges and opportunities that necessitate innovative strategies for success. Navigating complex regulatory requirements, shifting reimbursement policies, and the imperative for enhanced patient engagement underscores the critical importance of leveraging comprehensive data insights.
By harnessing the power of advanced analytics, AMCs can achieve a profound understanding of treatment patterns, patient demographics, and operational efficiencies. This understanding ultimately leads to improved health outcomes and financial sustainability.
This article explores the pivotal role of data-driven decision-making and collaboration in shaping the future of AMCs, examining how strategic partnerships and robust compliance frameworks can cultivate growth and resilience in an increasingly competitive environment.
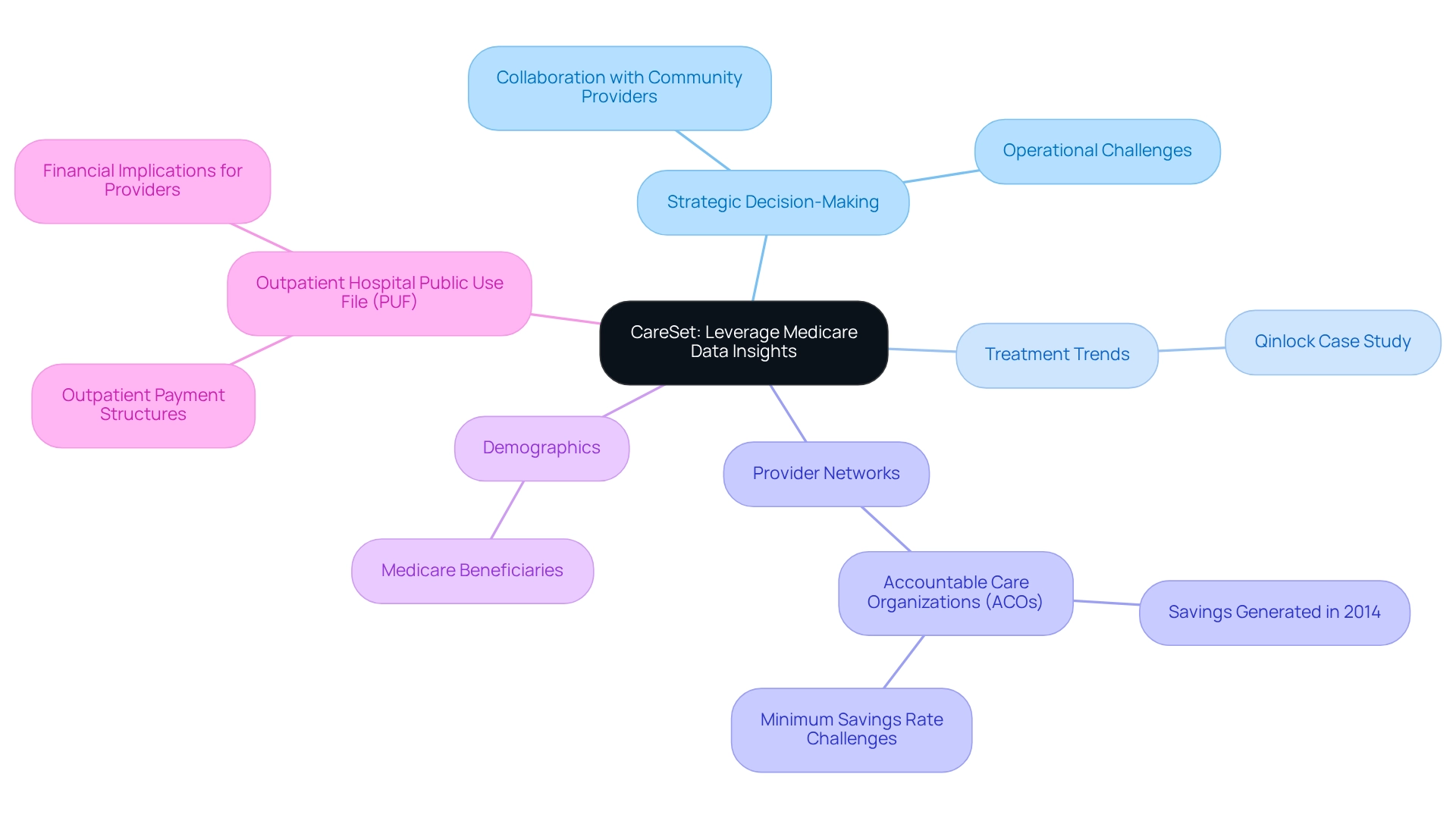
CareSet: Leverage Comprehensive Medicare Data Insights for Strategic Decision-Making
CareSet excels in extracting and interpreting intricate Medicare claims information, empowering academic medical centers to make informed decisions based on comprehensive insights. By examining more than $1.1 trillion in yearly claims, organizations can reveal essential insights about treatment trends, provider networks, and demographics of individuals. This information is crucial for strategic planning and resource distribution, allowing healthcare organizations to improve care for individuals and optimize operational efficiencies. The effective application of these insights not only results in better health outcomes but also promotes the financial sustainability of academic medical centers.
Recent studies suggest that organizations utilizing Medicare data insights have experienced notable enhancements in healthcare delivery. For example, the case study of an oncology treatment manufacturer focusing on the 4th line of therapy, Qinlock, for Gastrointestinal Stromal Tumor (GIST) illustrates how timely engagement with medical providers can enhance treatment options for patients. The early success of certain AMCs in the Medicare Shared Savings Program (MSSP) further illustrates the potential for collaboration with community providers, which can enhance care coordination for Medicare beneficiaries across the continuum of care. In 2025, Medicare claims data continues to significantly influence medical decision-making, with statistics showing that while 89 Accountable Care Organizations (ACOs) generated savings for Medicare in 2014, many did not meet the minimum savings rate, highlighting the need for robust data analysis to drive better outcomes.
Case studies, such as the Outpatient Hospital Public Use File (PUF), provide a detailed view of outpatient payment structures, allowing healthcare providers and policymakers to assess the financial implications of outpatient services. This level of insight is essential for asset management companies seeking to enhance cost management strategies and care for individuals. The findings from the PUF can directly influence accountable care organizations’ operational strategies by informing them about hospital-specific charges and payment structures.
Experts highlight the significance of Medicare claims information for academic medical centers, noting that organizations effectively utilizing this information can make strategic choices that improve engagement with individuals and enhance service delivery. As Benjamin M. Gerber, JD, vice president of Network & Payment Strategy at Jefferson Health, stated, ‘those academic medical centers that worked in collaboration with community providers appeared to achieve the most success during the 2014 performance year.’ By utilizing CareSet’s comprehensive Medicare data analysis, academic medical centers can effectively address immediate operational challenges while fostering long-term strategic growth, which ultimately leads to improved outcomes for individuals and a more sustainable model for health services.
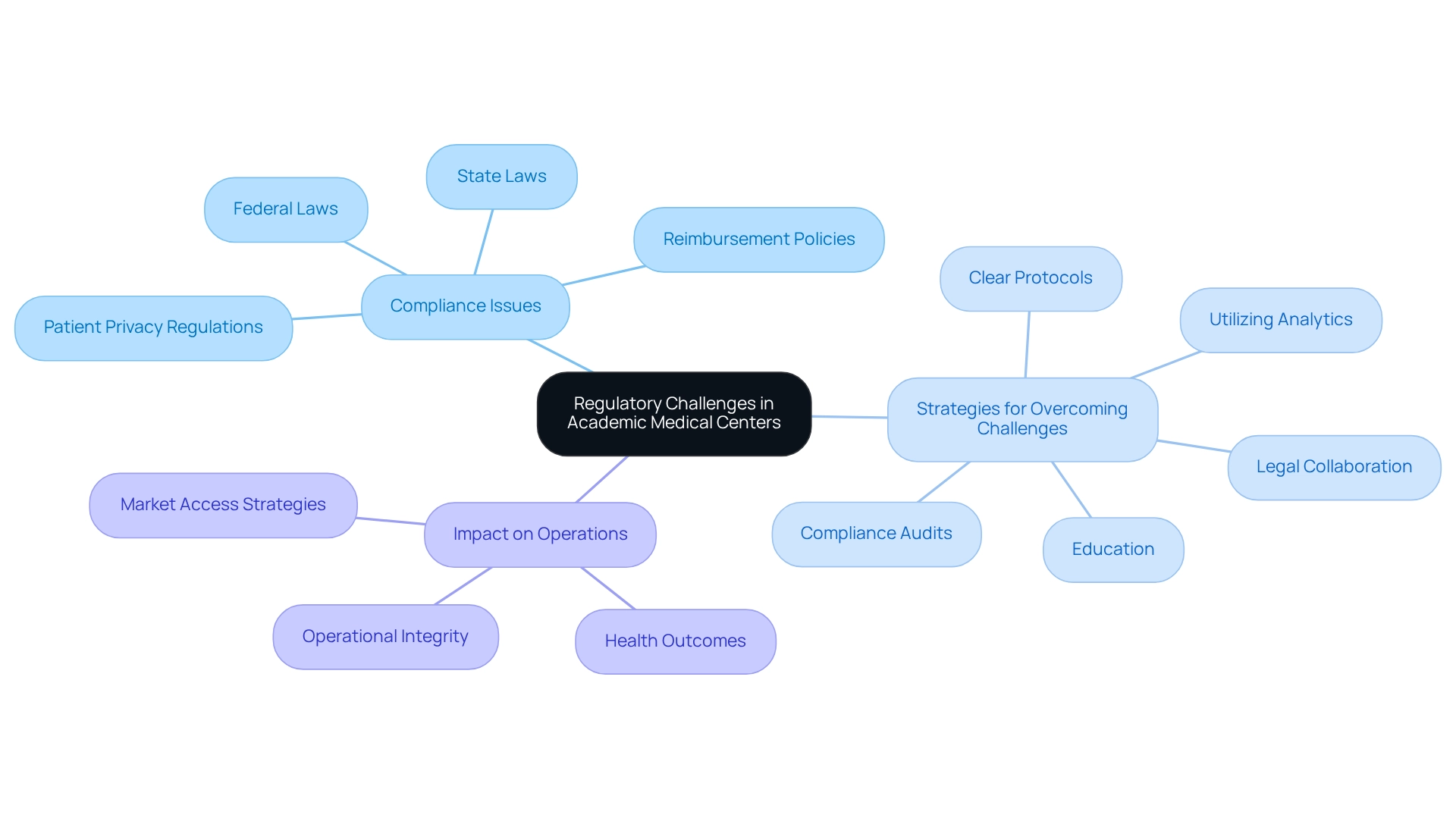
Identify and Overcome Regulatory Challenges in Academic Medical Centers
Academic medical centers encounter a multitude of regulatory challenges, including compliance with federal and state laws, reimbursement policies, and patient privacy regulations. Notably, in 2025, 11% of employees in healthcare organizations reported feeling pressured to approve engagements that presented unacceptable corruption risks. This statistic underscores the critical need for robust compliance strategies, as such pressures can lead to significant risks for asset management companies and their operational integrity.
To adeptly navigate these challenges, asset management firms must prioritize regular compliance audits and cultivate a culture of continuous education among staff. Establishing clear compliance protocols is imperative, as is collaboration with legal experts to ensure adherence to ever-evolving regulations. Richard Stevenson, a specialist in cybersecurity risk management, emphasizes the importance of creating effective compliance programs that meet security compliance standards, which are a necessity for academic medical centers and other healthcare organizations within today’s complex regulatory landscape. Utilizing analytics can proactively identify potential compliance challenges before they escalate, safeguarding operational integrity and allowing these organizations to focus on patient care. CareSet’s comprehensive approach to addressing immediate data needs while fostering long-term strategic growth can prove instrumental for asset management companies in leveraging data analytics for compliance strategies. By remaining informed about regulatory changes and adapting their strategies accordingly, asset management firms can enhance their compliance frameworks.
For example, the professionalization of intercollegiate athletics has raised concerns regarding sustainability in athletic programs, which may parallel the challenges faced by asset management firms in balancing compliance with operational demands. By implementing these strategies, asset management companies can not only fortify their compliance frameworks but also improve health outcomes and organizational resilience, ultimately positively influencing their market access strategies.
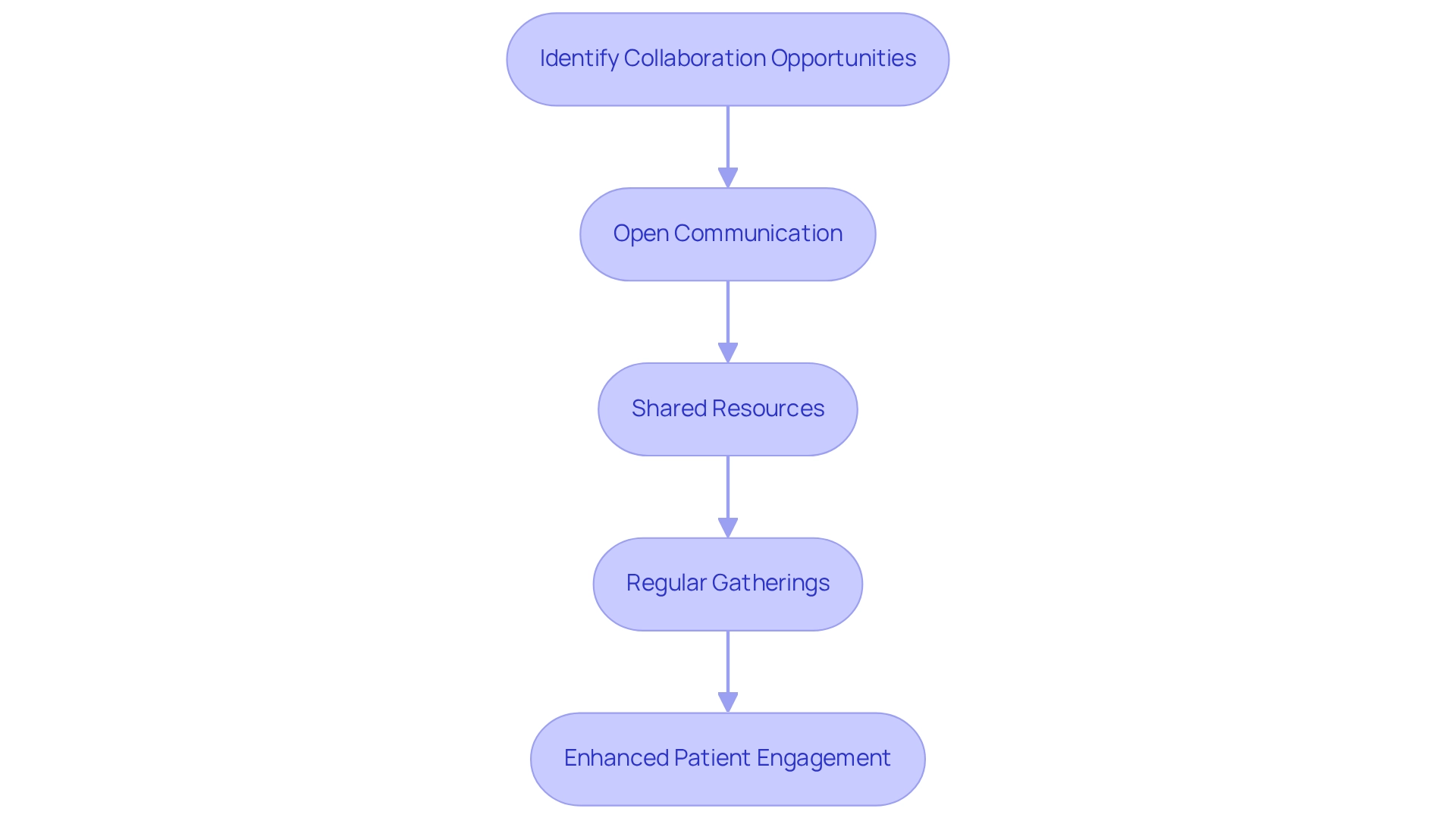
Foster Collaborative Relationships with Healthcare Providers and Payers
Fostering collaborative relationships with healthcare providers and payers is essential for academic medical centers to thrive in today’s healthcare landscape. These partnerships enable shared resources, streamline care delivery, and significantly enhance patient engagement. Asset management companies should emphasize open communication and transparency with their partners, employing analytical insights to identify collaboration opportunities. For instance, CareSet’s extensive Medicare information solutions, which include insights from over 62 million beneficiaries and 6 million providers, empower academic medical centers to effectively improve their engagement strategies. Regular gatherings and collaborative efforts not only foster trust but also guarantee alignment in objectives aimed at enhancing care and outcomes.
The American Hospital Association (AHA) stresses that concentrating on the human element of mergers and acquisitions is vital, underscoring the necessity for strategic alliances to tackle the financial difficulties that nearly 40% of hospitals are expected to encounter in 2025. This highlights the importance of collaboration to enhance operational viability and service delivery. Successful collaborations between payers and academic medical centers can lead to innovative care models that enhance experiences for individuals. Furthermore, statistics reveal that academic medical centers that integrate over 100 external data sources are able to better understand demographics and treatment patterns, thus facilitating more effective collaboration with healthcare providers. CareSet’s analytics solutions, which explore $1.1 trillion in yearly claims, enable asset management companies to identify key spending trends and resource requirements, further improving their capacity to engage with providers. Expert opinions indicate that enhancing client involvement through these partnerships is essential, as individuals themselves are invaluable sources of insight into care enhancements, as noted by rights advocate Regina Holliday. By establishing robust collaborative partnerships, these organizations can not only meet urgent data requirements but also promote sustained strategic development, ultimately resulting in improved patient outcomes.
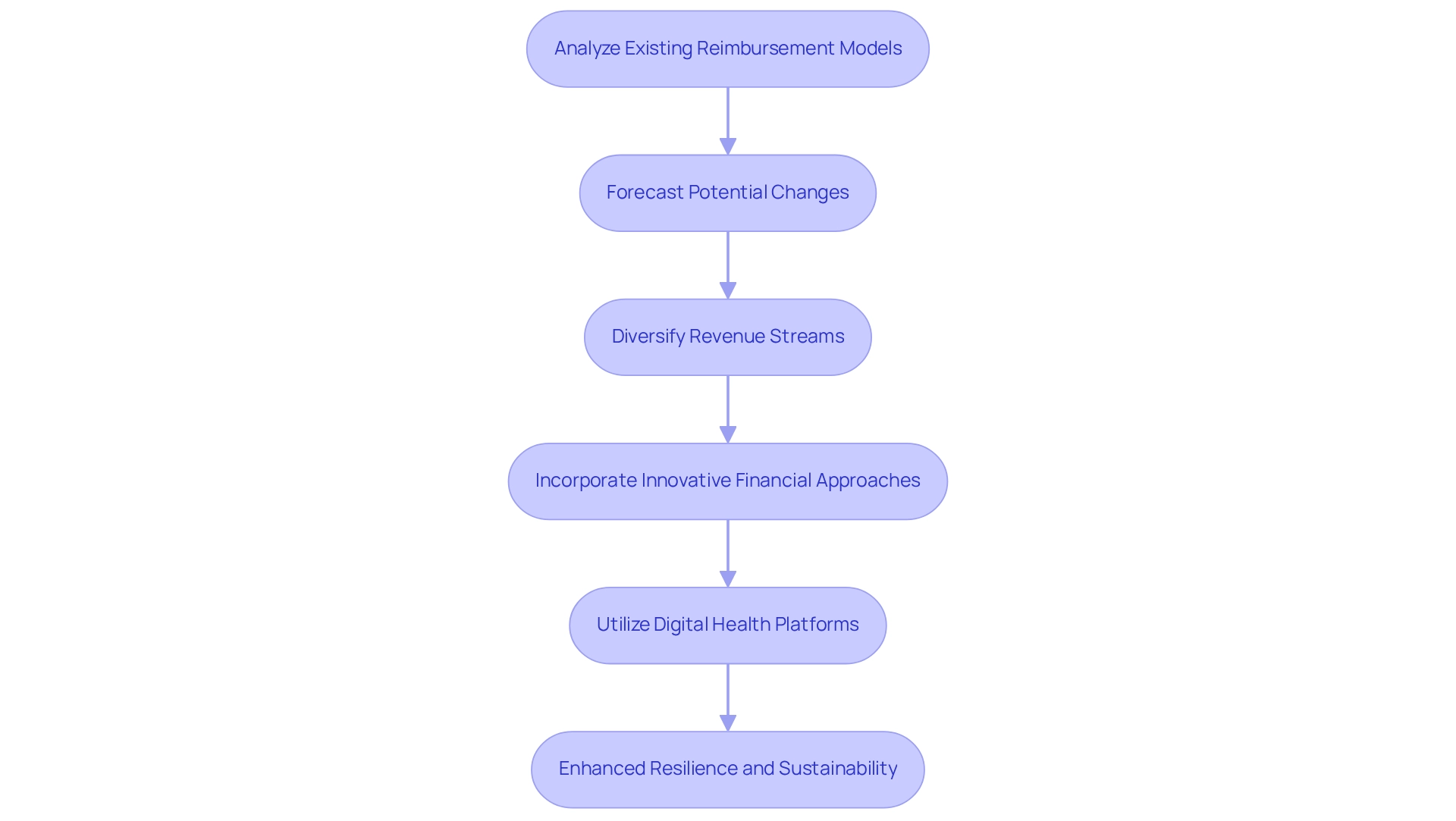
Adapt Financial Strategies to Evolving Reimbursement Policies
To thrive amidst the shifting landscape of reimbursement policies, academic medical centers must proactively adapt their financial strategies. This involves a thorough analysis of existing reimbursement models and forecasting potential changes to ensure alignment with new policies.
Healthcare organizations should consider diversifying their revenue streams, particularly through value-based care initiatives, which can significantly enhance financial stability. Regular financial evaluations and strategic planning meetings are crucial for sustaining agility and adaptability to the changing reimbursement landscape.
As the healthcare industry progresses, academic medical centers are increasingly incorporating innovative financial approaches to manage these transformations effectively, utilizing analytics and insights from CareSet’s extensive Medicare solutions, which cover over $900 billion in claims annually and more than 14 years of claims information. This information enables asset management companies to recognize trends and enhance resource distribution while acquiring a deeper insight into various demographic groups and pharmaceutical usage, ensuring they stay competitive.
The emergence of digital health platforms has transformed conventional models, encouraging academic medical centers to explore new opportunities for interaction and care delivery. These platforms not only enhance client access but also provide opportunities for academic medical centers to integrate clinical assets and medical devices into their financial strategies, thereby improving overall efficiency.
Statistics indicate that academic medical centers that implement robust financial planning in response to changing reimbursement policies are better positioned for long-term success. For instance, Cityblock Health’s combination of medical care with social services for underserved communities illustrates how creative financial strategies can result in enhanced health outcomes and financial stability.
Expert insights suggest that embracing value-based care, supported by comprehensive data insights from CareSet, not only improves patient outcomes but also stabilizes financial performance. As one financial analyst pointed out, ‘Value-based care is not merely a trend; it’s a fundamental change that can transform the financial success of academic medical centers.’
By adopting these strategies and leveraging CareSet’s insights, academic medical centers can enhance their resilience and ensure their sustainable growth in an increasingly complex healthcare landscape.
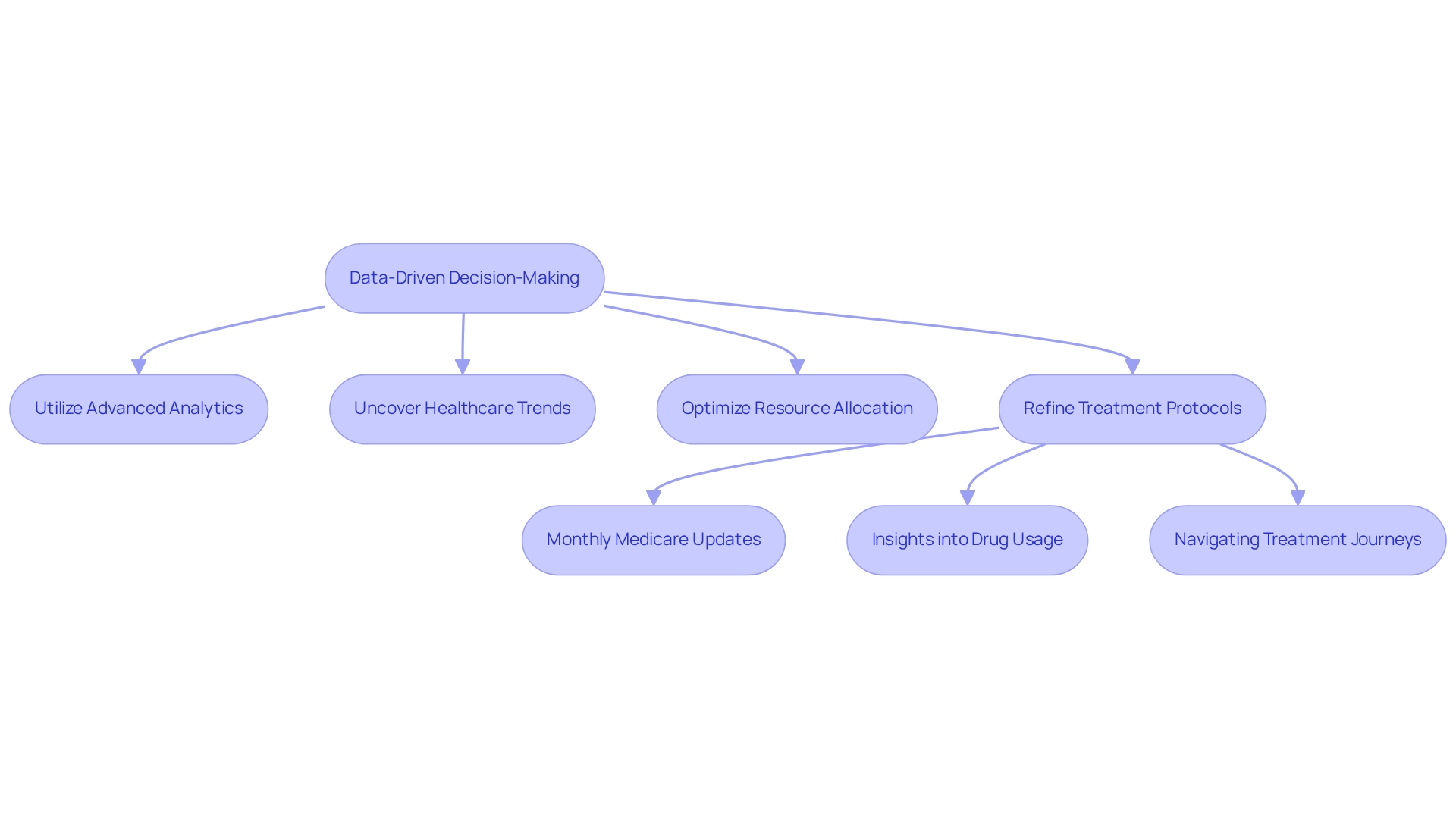
Implement Data-Driven Decision-Making for Enhanced Patient Outcomes
Establishing data-informed decision-making procedures is crucial for academic medical centers that are aiming to enhance outcomes for individuals. By utilizing advanced analytics, including CareSet’s innovative Medicare data solutions, AMCs can uncover trends in healthcare, optimize resource allocation, and refine treatment protocols. CareSet’s monthly Medicare updates offer essential insights into drug usage and treatment pathways, addressing key business questions such as:
- Which diseases providers diagnose and manage?
- How individuals navigate their treatment journeys?
- What treatments are being approved by Medicare Part D Plans?
These insights enhance provider engagement and enable healthcare professionals to navigate the complexities of patient journeys effectively.
A recent study shows that while 91% of organizations acknowledge the significance of information-driven decision-making, only 57% actually incorporate insights in their business strategies. This gap emphasizes the need for AMCs to cultivate a culture of information literacy among their staff. Investing in sturdy analytics tools, like those provided by CareSet, enables medical professionals to make informed choices, ultimately resulting in improved care and operational efficiencies.
As healthcare organizations increasingly utilize data analytics, they can propel innovations that change healthcare delivery, ensuring that outcomes are prioritized in every decision made. Entities excelling in analytics will prosper in a data-abundant setting, making it essential for asset management companies to embrace these practices to stay competitive and efficient.
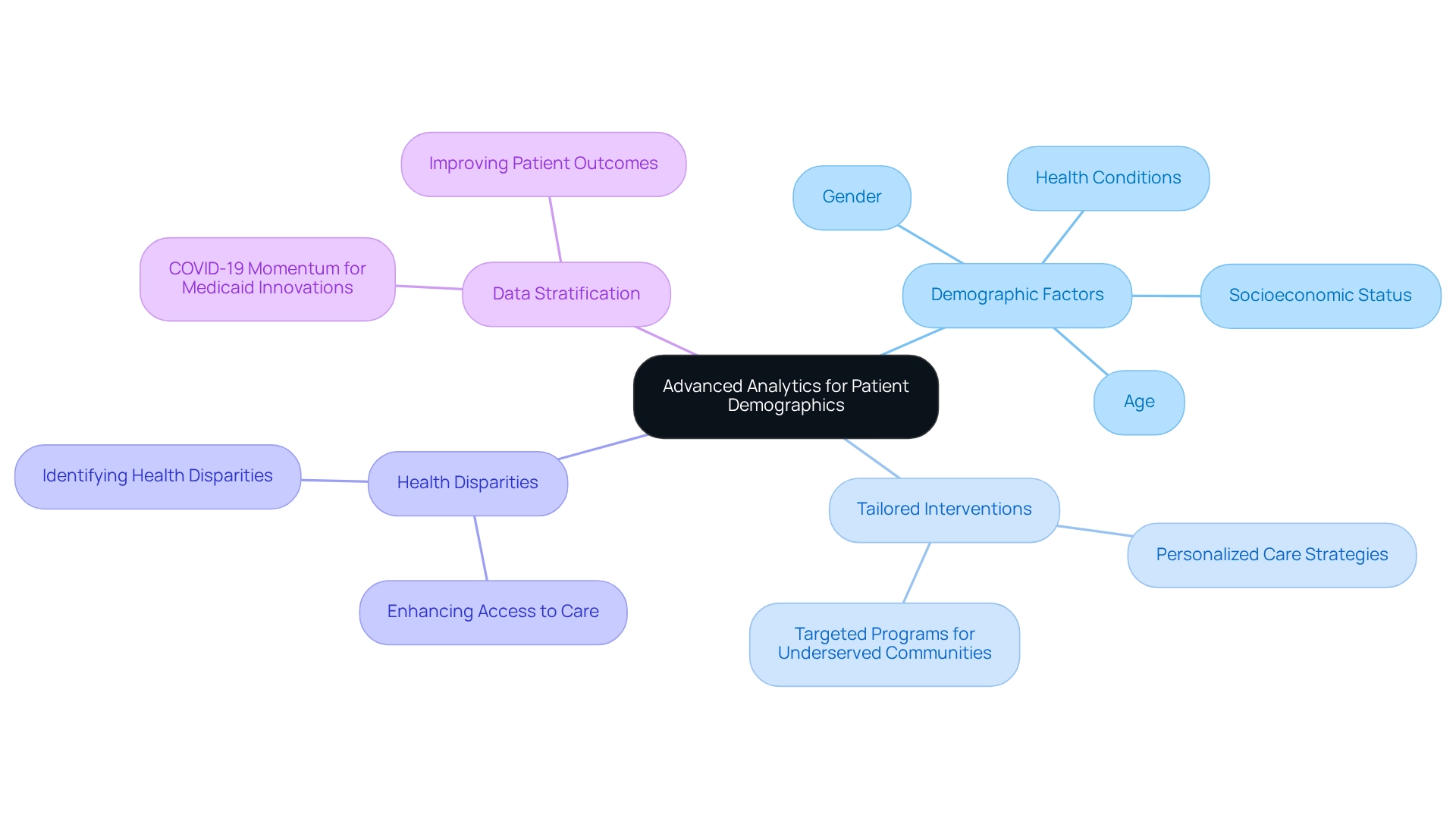
Utilize Advanced Analytics for Patient Demographic Insights
Academic medical centers must leverage advanced analytics to extract valuable insights into demographics, including factors such as age, gender, socioeconomic status, and health conditions. This thorough analysis empowers asset management companies to tailor interventions and personalize care strategies, effectively addressing the distinct needs of their diverse client groups. By utilizing demographic data, academic medical centers can identify health disparities and implement targeted programs aimed at enhancing access to care for underserved communities.
For instance, a recent study involving 674 individuals highlighted the critical role of demographic insights in shaping medical strategies, with 549 individuals ultimately participating in the research. This statistic emphasizes the importance of demographic insights in informing clinical practices and facilitating successful interventions that improve patient outcomes.
Shilpa Patel underscores the necessity of stratifying data to effectively customize medical efforts, suggesting that harnessing momentum from the COVID-19 pandemic can drive Medicaid innovations. This case study illustrates how demographic insights can lead to successful interventions in medical care.
Medical researchers assert that understanding the demographics of individuals is vital for enhancing operations and promoting person-centered care in academic medical centers within today’s complex medical landscape. By recognizing the significance of demographic information, organizations can devise innovative solutions that address health disparities and foster equitable access to care.
As CareSet’s extensive medical information insights reveal, “By acknowledging the significance of individual demographic information and utilizing its advantages, medical organizations can improve their operations, enhance outcomes for individuals, and provide individual-focused care in today’s intricate medical environment.”
As we move into 2025, the integration of advanced analytics for demographic insights will be essential in developing effective care strategies within academic medical centers. This focus on data-informed decision-making, supported by CareSet’s Medicare data solutions, will empower care providers to proactively respond to the evolving needs of their client populations, ultimately leading to improved health outcomes and a more equitable medical system. To explore how CareSet can deepen your understanding of patient demographics and strengthen your medical strategies, let’s initiate a conversation.
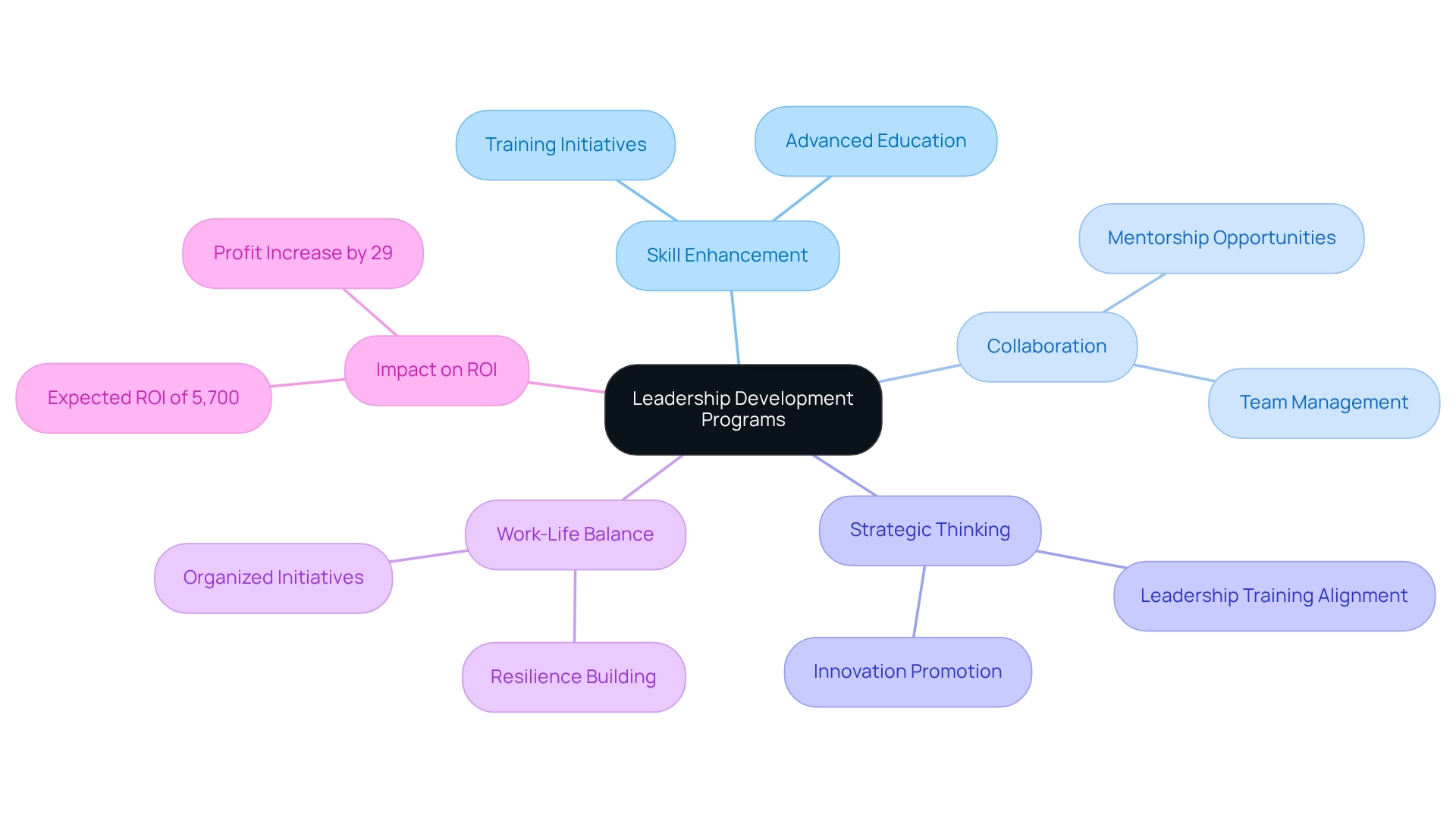
Invest in Leadership Development Programs for Continuous Growth
Investing in leadership development programs is essential for academic medical centers to foster a culture of continuous growth and innovation. These initiatives must prioritize the enhancement of leadership skills, encourage collaboration, and promote strategic thinking among leaders in the health sector. With 74% of leaders struggling to maintain a healthy work-life balance, targeted training can mitigate these challenges by equipping leaders with the necessary tools to thrive in a demanding environment. By addressing work-life balance through organized initiatives, organizations can cultivate a more resilient leadership team, better prepared to manage the complexities of contemporary medical services.
Continuous training and mentorship opportunities are vital for ensuring that leaders can navigate the evolving medical landscape, particularly as remote work gains prominence. Research indicates that companies investing in leadership development can expect an average return on investment (ROI) of 5,700% by 2030. This statistic underscores the profound impact of effective leadership on organizational success and profitability, particularly when academic medical centers implement specific training initiatives aligned with their strategic goals. Furthermore, successful leadership training initiatives in academic medical centers have shown that effective team management and recognition of individual strengths can result in organizational profits increasing by up to 29%. This highlights the significance of fostering innovation through well-structured leadership programs, which not only enhance individual capabilities but also drive overall institutional performance. The combination of advanced education with workplace training further solidifies the foundation for long-term success in leadership development. As we approach 2025, the emphasis on leadership development in medical organizations will only intensify. Expert opinions consistently affirm that strong leadership is a cornerstone of successful academic medical centers, allowing them to adapt to challenges and seize opportunities in a rapidly changing healthcare environment. By prioritizing leadership training, these organizations can cultivate innovative leaders prepared to guide their teams toward sustained success.
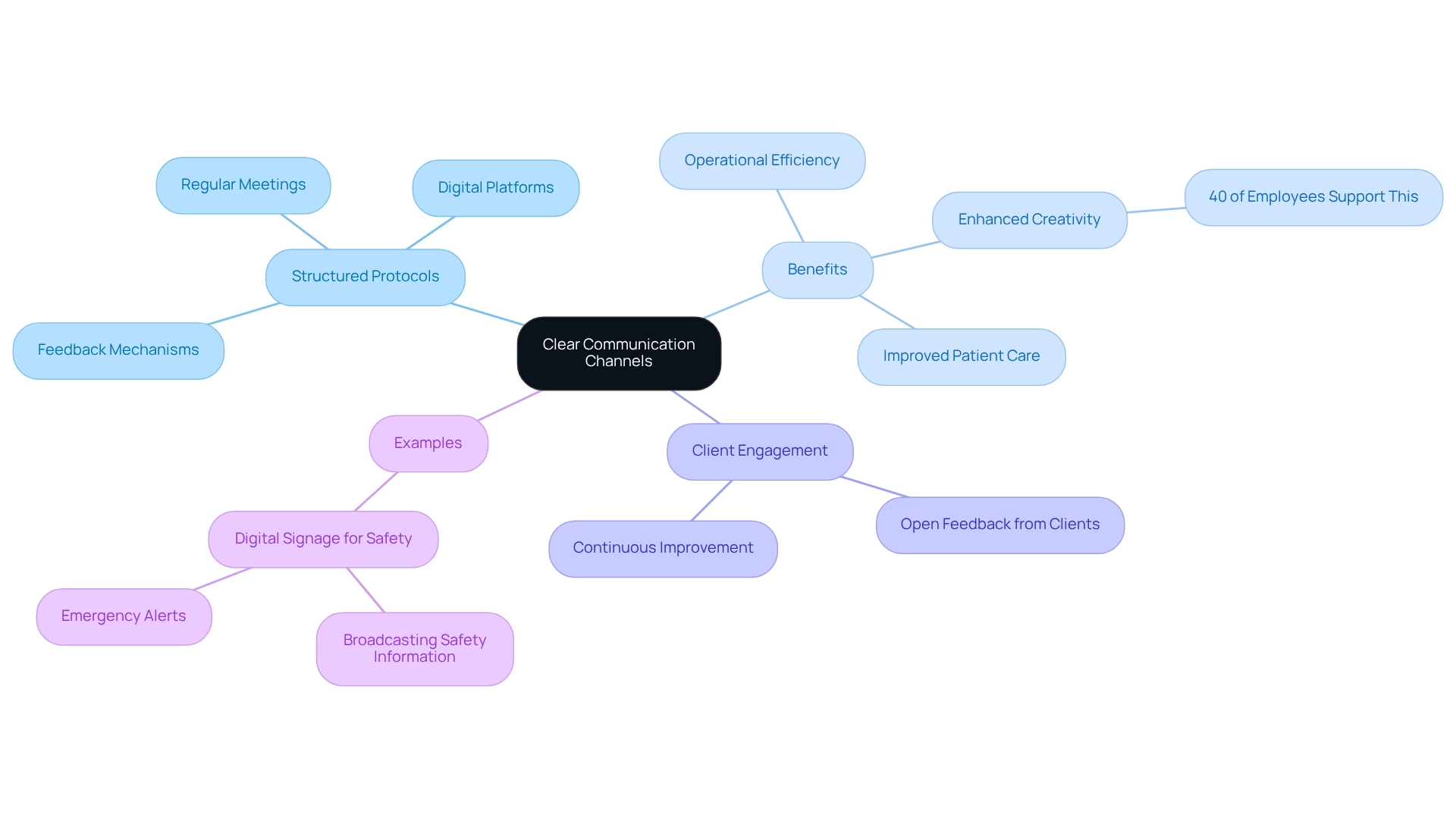
Establish Clear Communication Channels for Team Collaboration
Creating transparent communication pathways is essential for academic medical centers to boost team collaboration and enhance outcomes for individuals. Implementing structured communication protocols—such as regular meetings, digital communication platforms, and robust feedback mechanisms—facilitates effective information sharing among team members. This approach not only promotes open dialogue and transparency but also aligns staff objectives, leading to operational efficiency. In fact, studies indicate that 40% of employees believe regular communication enhances team creativity and innovation, underscoring the importance of fostering a communicative culture.
Furthermore, individuals spend an average of 8 minutes on the phone arranging appointments, often facing multiple transfers, which emphasizes the need for effective communication in interactions. Encouraging open feedback from clients and medical staff fosters an environment for continuous improvement in communication practices, further enhancing client engagement and satisfaction. Successful initiatives in academic medical centers have demonstrated that structured communication can significantly enhance team dynamics, ultimately benefiting patient care. As Ira Brooker notes, ‘Our in-house experts will develop a solution tailored to your practice’s specific needs while demonstrating personalized solutions to keep your communications timely, relevant, and accurate.’
By prioritizing effective communication strategies, these organizations can create an environment conducive to collaboration, ensuring that all team members are informed and engaged in their roles. For instance, the use of digital signage to broadcast safety information and emergency alerts in healthcare settings exemplifies how structured communication can enhance workplace safety and improve emergency responses. By integrating these strategies, asset management companies can ensure that communication remains a cornerstone of their operational success.
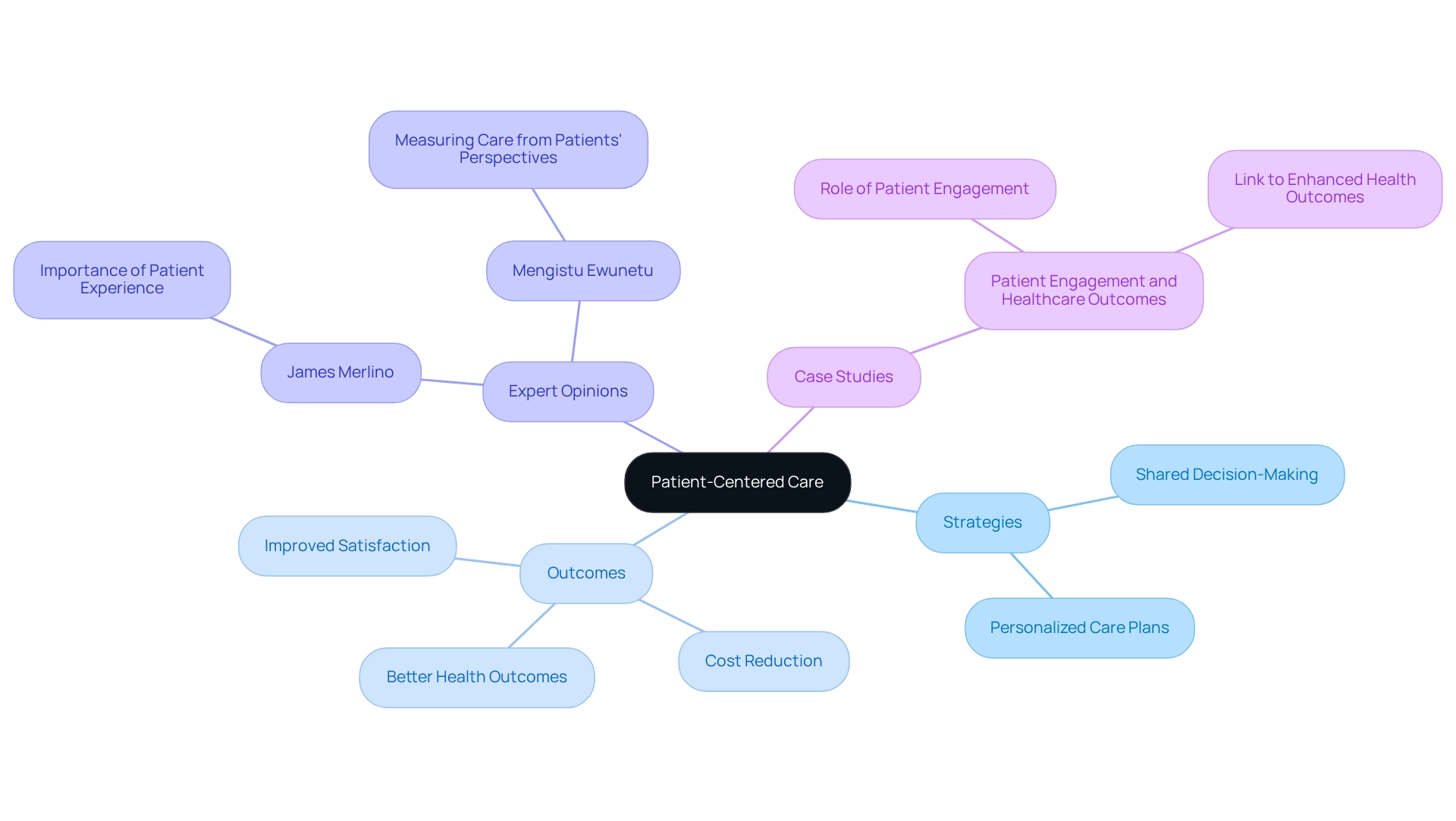
Prioritize Patient-Centered Care to Improve Satisfaction and Outcomes
Focusing on client-centered care is essential for academic medical centers that are striving to boost satisfaction and enhance health outcomes. This approach emphasizes the active participation of individuals in their care choices, ensuring that their preferences are recognized and incorporated into tailored treatment plans. To effectively promote client involvement, academic medical centers should adopt strategies such as:
- Shared decision-making
- The creation of personalized care plans
Statistics indicate that academic medical centers concentrating on client-centered care can significantly enhance treatment outcomes while lowering costs. A recent study highlights that improved engagement through person-centered care (PCC) is associated with better health outcomes, reinforcing the necessity for healthcare systems to adopt these approaches.
Expert opinions underscore the significance of this focus. James Merlino, Chief Clinical Transformation Officer at Cleveland Clinic, emphasizes that prioritizing the experience of individuals is vital for success in today’s competitive healthcare landscape. Furthermore, experts in client engagement advocate for assessing care from the clients’ viewpoints to recognize and prioritize areas requiring enhancement. Mengistu Ewunetu from the Department of Adult Health Nursing states, ‘Thus, measuring care centered around individuals’ perspectives is critical to identify and prioritize areas of health care where improvements are needed during delivery of services.’
Case studies illustrate the effectiveness of patient-centered initiatives. One significant study on individual involvement and medical outcomes shows that engaging individuals in their care processes results in better health outcomes and satisfaction. This research claims that individual-focused care can lead to improved treatment results and reduced expenses by actively involving individuals in their care processes. By applying these strategies, organizations can not only enhance the overall experience of individuals but also promote long-term advancements in health outcomes, ultimately benefiting both individuals and healthcare providers.
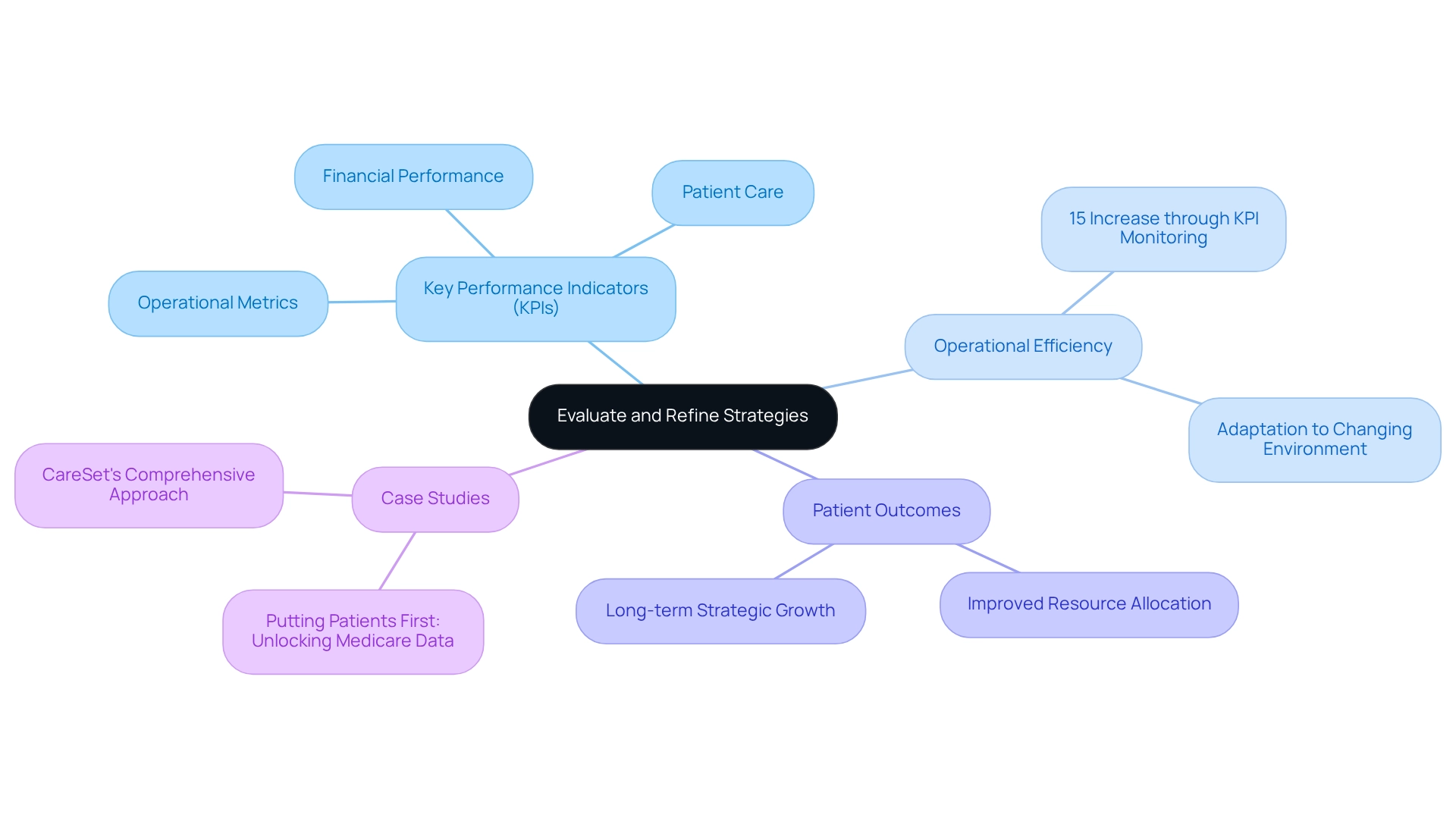
Evaluate and Refine Strategies Based on Performance Metrics
Academic medical institutions must prioritize the regular evaluation and refinement of their strategies through the lens of performance metrics. Establishing key performance indicators (KPIs) that focus on patient outcomes, operational efficiency, and financial performance enables academic medical centers to identify areas needing improvement and apply data-driven adjustments.
For instance, comprehensive analysis of KPIs reveals that asset management companies actively monitoring these metrics can achieve a 15% increase in operational efficiency over a three-year period. Ongoing observation and evaluation not only allow asset management companies to adapt to the changing medical environment but also enhance their overall efficiency. This proactive approach fosters long-term strategic growth, as evidenced by the case study ‘Putting Patients First: Unlocking Medicare Data to Empower HCP,’ which demonstrates that academic medical centers leveraging KPIs have significantly improved patient care and resource allocation.
CareSet’s comprehensive Medicare information solutions empower medical strategies by providing insights from over 62 million beneficiaries and 6 million providers, addressing immediate information needs while fostering long-term growth for its partners in the medical sector.
As industry analysts emphasize, ‘Defining a focused set of KPIs before launching campaigns can enhance analytics opportunities,’ underscoring the critical role of information in driving operational success. W. Edwards Deming noted, ‘Without data, you’re just another person with an opinion,’ highlighting the transformative power of data.
In 2025, the integration of performance metrics will be more vital than ever as academic medical centers strive to meet the demands of a rapidly changing healthcare environment.
Conclusion
In the face of an evolving healthcare landscape, academic medical centers (AMCs) must prioritize data-driven decision-making to navigate challenges and seize opportunities effectively. By leveraging comprehensive Medicare data insights, AMCs can enhance their understanding of treatment patterns, patient demographics, and operational efficiencies. The successful application of these insights not only leads to improved patient outcomes but also ensures financial sustainability amidst shifting reimbursement policies and regulatory challenges.
Collaboration emerges as a key theme throughout the strategies discussed. Fostering strong partnerships with healthcare providers and payers enables AMCs to streamline care delivery and enhance patient engagement. As demonstrated through various case studies, these collaborations yield innovative care models that significantly improve patient experiences and outcomes. Furthermore, investing in leadership development and establishing clear communication channels are critical components that empower AMC leaders to cultivate a culture of continuous growth and innovation.
As AMCs move forward, the integration of advanced analytics and performance metrics will be paramount. By continuously evaluating and refining strategies based on data insights, AMCs can proactively address operational challenges while enhancing patient-centered care. This holistic approach not only positions AMCs for long-term resilience but also reinforces their commitment to delivering high-quality healthcare in a competitive environment.
Ultimately, the successful navigation of this complex healthcare landscape hinges on AMCs’ ability to embrace data-driven strategies, foster collaborative relationships, and prioritize patient-centered initiatives. By doing so, they will not only improve health outcomes but also solidify their role as leaders in the healthcare sector as they adapt to the demands of the future.

