Overview
The article highlights nine essential guideline-directed medical therapy (GDMT) medications that are vital for effective heart failure management. It underscores the significance of these medications—including ARNIs, beta-blockers, and MRAs—backed by clinical evidence and real-world data. This focus illustrates their critical roles in improving patient outcomes and navigating the complexities of heart failure treatment. As we explore these medications, we recognize their impact on enhancing the quality of care for patients facing heart failure.
Introduction
In the evolving landscape of heart failure management, advancements in medical therapies are crucial, driven by the pressing need for improved patient outcomes. Healthcare professionals are dedicated to optimizing treatment strategies, leading to the emergence of a multitude of medications, each playing a critical role within the guideline-directed medical therapy (GDMT) framework.
From the groundbreaking Angiotensin Receptor Neprilysin Inhibitors (ARNIs) to the time-tested digitalis glycosides, this diverse array of options presents both opportunities and challenges for clinicians. This article delves into the essential components of heart failure treatment, examining the efficacy, benefits, and ongoing research surrounding these vital therapies.
By exploring the intricacies of each medication class, stakeholders can better navigate the complexities of heart failure management, ultimately enhancing patient care.
CareSet: Comprehensive Medicare Data Insights for GDMT Medications
CareSet distinguishes itself in the acquisition and analysis of intricate Medicare claims data, delivering comprehensive insights into gdmt medications for cardiac issues. By scrutinizing over $1.1 trillion in annual claims data, CareSet uncovers essential care patterns and identifies service gaps, empowering healthcare stakeholders with actionable insights derived from the experiences of more than 62 million beneficiaries and 6 million providers. This data-driven approach is crucial for enhancing care and improving outcomes in heart failure management.
Recent findings from the CHAMP-HF registry indicate that fewer than 1% of individuals received optimal care when accounting for sufficient dosages and the inclusion of mineralocorticoid receptor antagonists (MRAs). This alarming statistic underscores the urgent need for a strategic approach to gdmt medications, balancing therapeutic efficacy with care complexity.
As S Mollenkopf from Edwards Lifesciences articulates, ‘The absence of gdmt medications was independently associated with increased annual healthcare utilization, particularly in terms of annualized hospitalizations, hospital days, and emergency room visits.’ By leveraging extensive Medicare data insights, CareSet not only addresses immediate care needs but also fosters enduring advancements in cardiac management, ultimately enhancing patient outcomes.
Furthermore, the call for further investigation in the case study titled ‘Future Directions in Cardiac Insufficiency Management Research’ highlights the complexities inherent in managing this condition and the necessity for ongoing exploration of GDMT medications. CareSet’s dedication to providing actionable insights positions it as an essential partner for pharmaceutical market access managers aiming to optimize their practices for GDMT medications strategies.
Angiotensin Receptor Neprilysin Inhibitors (ARNIs): A Game Changer in Heart Failure Treatment
Angiotensin Receptor Neprilysin Inhibitors (ARNIs), particularly sacubitril/valsartan, have revolutionized the management of cardiac insufficiency. By combining the effects of an angiotensin receptor blocker with neprilysin inhibition, ARNIs not only reduce blood pressure but also enhance cardiac output and significantly lower hospitalization rates. Clinical trials have consistently shown that ARNIs lead to a substantial decrease in the risk of cardiovascular mortality and heart failure-related hospital admissions, solidifying their status as a cornerstone of GDMT medications for heart failure and reduced ejection fraction (HFrEF) patients. Evidence supports the incorporation of ARNIs into care guidelines, underscoring their vital role in healthcare.
For instance, a retrospective cohort study focusing on individuals with HFrEF who were naïve to renin–angiotensin–aldosterone system inhibitor (RAASi) therapy indicated that those initiating treatment with sacubitril/valsartan experienced markedly lower rates of all-cause hospitalization compared to those starting on traditional angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARB). While the rates of cardiac hospitalizations were comparable between the two groups, the overall clinical and economic burden was significantly reduced for patients treated with sacubitril/valsartan.
As we look towards 2025, ongoing clinical trials continue to affirm the effectiveness of ARNIs in managing cardiac conditions, with emerging data highlighting their beneficial impact on cardiovascular outcomes. Data from the Affiliated Hospital of North Sichuan Medical College, although not publicly accessible, corroborates these findings. This evidence emphasizes the critical role that GDMT medications, including ARNIs, play in enhancing patient care and outcomes in cardiac diseases. As Rachel Studer noted, ‘The incorporation of ARNIs into treatment protocols has been a game changer for managing cardiac issues effectively.
Beta-Blockers: Essential for Heart Failure Management
Beta-blockers, particularly carvedilol and metoprolol succinate, are pivotal in treating cardiac dysfunction due to their capability to decrease pulse rate, lower blood pressure, and enhance left ventricular performance. These medications have demonstrated significant benefits in reducing both mortality and hospitalization rates among individuals with heart failure with reduced ejection fraction. Recent studies indicate that patients on beta-blockers experience improved real-world outcomes, underscoring their importance in clinical care protocols.
Current clinical guidelines endorse the inclusion of beta-blockers as a fundamental component of GDMT medications. This recommendation is substantiated by evidence showing that beta-blockers not only bolster cardiac function but also enhance the overall quality of life for patients. A comparative effectiveness study titled ‘Comparative Effectiveness of Beta-Blockers Across Demographics’ highlighted the differential effects of beta-blockers among various demographic groups. While both black and white individuals benefit from these interventions, the reduction in mortality is less pronounced in black individuals. As noted by Stephen S. Gottlieb, M.D., “Black individuals with hypertension do not respond as effectively as whites to therapy with beta-adrenergic blockers,” emphasizing the necessity for tailored therapeutic strategies and further investigation into the factors driving these disparities.
Data from recent studies reveal a marked decrease in hospitalization rates for patients with cardiac conditions on beta-blockers, accentuating their critical role in the effective management of cardiac issues. As the treatment landscape for cardiac dysfunction evolves, beta-blockers remain an essential element, supported by ongoing research and expert insights that continue to shape clinical practice and guidelines. Furthermore, the findings from the comparative effectiveness study may inform future guidelines for managing myocardial infarction, reflecting the broader implications of this research. It is noteworthy that this study received support from grant 18059186 from the Japan Agency for Medical Research and Development, which adds credibility to its conclusions.
ACE Inhibitors: A Cornerstone of GDMT for Heart Failure
Angiotensin-converting enzyme (ACE) inhibitors, particularly lisinopril and enalapril, are pivotal components of gdmt medications for managing cardiac dysfunction. These medications operate by inhibiting the renin-angiotensin-aldosterone system (RAAS), leading to vasodilation and a reduction in both preload and afterload, which together enhance cardiac output.
Research consistently demonstrates their effectiveness in lowering morbidity and mortality rates among patients with cardiac conditions. For example, a meta-analysis underscored the strengths of ACE inhibitors, highlighting a substantial sample size and high representativeness, while also noting limitations such as the reliance on aggregate data and variations among populations. Importantly, no evidence of publication bias was identified (p = 0.721), further affirming the reliability of these findings.
Expert opinions underscore the vital role of gdmt medications, including ACE inhibitors, in heart failure management, with studies confirming their efficacy in reducing hospitalizations and improving outcomes for patients. Real-world examples illustrate the success of lisinopril and enalapril in clinical practice, demonstrating significant reductions in morbidity among treated individuals.
Furthermore, ongoing research into the efficacy and safety outcomes of these therapies is crucial for ensuring their sustained effectiveness. Insights and critical comments from specialists, including Dr. Michael Fu, emphasize the importance of continual assessment in cardiac management. As research progresses in exploring treatment efficacy and safety outcomes, ACE inhibitors remain a cornerstone in the therapeutic landscape for cardiac insufficiency.

Angiotensin II Receptor Blockers (ARBs): Key Alternatives in GDMT
Angiotensin II receptor blockers (ARBs), such as losartan and valsartan, are effective alternatives for individuals who cannot tolerate ACE inhibitors due to side effects like persistent cough. These gdmt medications not only contribute to lowering blood pressure but also significantly improve symptoms of cardiac insufficiency, making them integral to guideline-directed medical therapy. Recent research indicates that ARBs can be particularly advantageous for patients with cardiac issues coupled with hypertension, enhancing overall management strategies.
Statistics reveal that ARBs demonstrate comparable effectiveness to ACE inhibitors in reducing morbidity and mortality among individuals with cardiac conditions. Clinical evidence supports that the use of losartan and valsartan as gdmt medications can lead to improved outcomes for those intolerant to ACE inhibitors, thereby expanding care options for this demographic. Additionally, the consideration of a ventricular assist device (VAD) as a bridge to transplantation is crucial for patients listed for cardiac transplantation who become inotrope-dependent, showcasing advanced management alternatives in cases of cardiac distress.
Expert insights underscore the importance of integrating individual preferences into care strategies, particularly when assessing ARB alternatives. Healthcare professionals advocate for ARBs due to their similar therapeutic benefits while minimizing adverse effects. It is also critical to acknowledge that the administration of digoxin should not hinder the initiation of other effective mortality-reducing medications, highlighting the importance of comprehensive treatment approaches in managing cardiac conditions.
Moreover, case studies have suggested that N-3 polyunsaturated fatty acids may slightly reduce mortality and cardiovascular admissions in individuals receiving optimal therapy for cardiac issues, emphasizing the need for a holistic strategy in managing these conditions. As we approach 2025, the field of heart failure management is continuously evolving, with ongoing research into the efficacy of ARBs. Incorporating patient values and preferences remains vital, ensuring that care plans are tailored to individual needs, ultimately leading to improved health outcomes. Notably, as stated by Konstam, M.A., no reduction in rehospitalization or mortality has been demonstrated, reinforcing the necessity for careful consideration in treatment decisions.
Mineralocorticoid Receptor Antagonists (MRAs): Vital for Heart Failure Patients
Mineralocorticoid receptor antagonists (MRAs), such as spironolactone and eplerenone, are pivotal in managing cardiac dysfunction with reduced ejection fraction (HFrEF). These medications are essential for preventing cardiac remodeling and alleviating fluid retention, which are critical for enhancing outcomes for affected individuals. Clinical studies consistently demonstrate that MRAs significantly reduce both mortality and hospitalization rates among patients with cardiac conditions, underscoring their importance as gdmt medications.
Recent findings reveal a troubling rise in the prevalence of heart failure with preserved ejection fraction (HFpEF), particularly attributed to an aging population. This trend accentuates the need for effective strategies, including the application of MRAs. Evidence from real-world scenarios indicates that spironolactone and eplerenone not only improve cardiac function but also contribute to better overall health outcomes for patients. As noted by John J V McMurray, the integration of MRAs into care plans is supported by extensive clinical evidence, enhancing their credibility in the field.
Furthermore, a case study titled “Evaluation of Bias in Heart Failure Studies” emphasizes the necessity of evaluating potential biases in clinical trials, ensuring the reliability of data that supports the efficacy of MRAs. Insights from specialists also highlight the significance of incorporating MRAs into management plans for cardiac insufficiency, particularly for individuals with diminished ejection fraction. The clinical evidence affirming the effectiveness of these agents in improving cardiovascular outcomes is robust, with numerous studies validating their role in GDMT medications.
As the landscape of cardiovascular issues evolves, MRAs remain a fundamental element in enhancing care and improving therapeutic effectiveness. To fully leverage the benefits of MRAs, healthcare professionals should adopt personalized care and monitoring strategies tailored to individual patient needs, thereby ensuring optimal outcomes.
Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors: Emerging Leaders in Heart Failure Therapy
Sodium-glucose cotransporter-2 (SGLT2) blockers, notably empagliflozin and dapagliflozin, have emerged as pivotal in the management of cardiac insufficiency. Originally developed for diabetes control, these medications have exhibited significant cardiovascular benefits, including a remarkable reduction in cardiac hospitalizations and improved renal outcomes. Recent studies indicate that SGLT2 inhibitors can lower the risk of hospitalization due to cardiovascular complications by up to 30%, underscoring their critical role in contemporary treatment protocols for these conditions.
The integration of SGLT2 inhibitors into gdmt medications marks a significant shift towards holistic treatment approaches that consider diverse aspects of individual health. The Kansas City Cardiomyopathy Questionnaire (KCCQ), frequently employed to assess health status in heart failure patients, shows that higher scores correlate with enhanced quality of life. Secondary outcomes from clinical trials have revealed improvements in KCCQ scores among patients receiving SGLT2 inhibitors, further affirming their contribution to overall well-being. As Udaya S Tantry noted, “Although constrained by inter-study heterogeneity, our findings support the existing guidelines concerning the use of SGLT2i, especially in individuals with HF.”
Expert perspectives bolster the efficacy of SGLT2 inhibitors in cardiac care. Clinical investigations consistently reveal their cardiovascular advantages, with findings endorsing their use in patients across various ejection fraction categories. Notably, statistical analysis techniques, such as logistic regression and Cox proportional hazards models, have been employed to evaluate the association between SGLT2 inhibitors and reduced hospitalization rates for cardiac conditions, ensuring the reliability of these conclusions. For instance, the study titled “Statistical Analysis Techniques in SGLT2 Inhibitor Study” utilized these methods to provide a thorough examination of the data, reinforcing the robustness of the conclusions regarding SGLT2 inhibitors.
Real-world evidence further illustrates the positive impact of empagliflozin and dapagliflozin on cardiac management. Data indicates that patients undergoing these therapies experience fewer hospitalizations and improved overall health status. As the landscape of cardiac dysfunction treatment evolves, SGLT2 inhibitors are positioned as a cornerstone of effective gdmt medications, offering both immediate and enduring benefits for individuals navigating this complex condition.
Diuretics: Essential for Symptom Management in Heart Failure
Diuretics, particularly loop diuretics such as furosemide, play a crucial role in managing symptoms associated with fluid overload. By promoting diuresis, these medications effectively alleviate symptoms such as dyspnea and edema, significantly enhancing comfort for individuals. Although diuretics do not directly influence mortality rates, their well-documented contribution to improving the quality of life for those with cardiac issues is noteworthy. Recent studies indicate that the outpatient increase of oral diuretics is common among individuals with cardiac insufficiency and reduced ejection fraction (HFrEF), underscoring their importance in ongoing management. The variability in diuretic response among patients with cardiac insufficiency necessitates a stepwise diuretic approach, as diuretic resistance correlates with serious clinical adverse outcomes. Current data demonstrate that effective diuretic use can lead to substantial relief from dyspnea and edema, which are vital for individual well-being. For instance, a recent evaluation identified key characteristics associated with an increase in diuretic doses, such as previous cardiac hospital admissions and elevated baseline diuretic doses, providing significant insights into optimizing management strategies.
In clinical practice, the effectiveness of furosemide in addressing fluid overload has been highlighted in numerous case studies, showcasing its practical applicability. Healthcare professionals assert that while diuretics are frequently utilized alongside other gdmt medications, their unique role in symptom management remains indispensable. As evidenced by the Change the Management of Individuals with Heart Failure Registry, outpatient escalation of oral diuretics is prevalent in the care of patients with HFrEF, reinforcing their essential function in therapeutic regimens. Consequently, diuretics remain a fundamental component in the medical toolkit for cardiac dysfunction, ensuring that individuals experience an improved quality of life throughout their ongoing care journey.
Hydralazine and Nitrates: Important Adjuncts in Heart Failure Treatment
Hydralazine and nitrates, particularly isosorbide dinitrate, serve as vital supplements in the management of cardiac dysfunction, especially for patients with reduced ejection fraction. This combination therapy has demonstrated significant benefits in specific populations, notably African Americans, where research indicates improved outcomes compared to traditional methods. By promoting vasodilation and decreasing preload, these gdmt medications enhance the overall effectiveness of guideline-directed medical therapy. Recent clinical trials underscore the efficacy of hydralazine and nitrates in treating cardiac conditions, revealing that their combined application can lead to better patient outcomes.
For instance, a study employing inverse probability weighting found no substantial associations between H-ISDN therapy and enhanced outcomes, highlighting the importance of thorough statistical analysis in evaluating treatment effects. This finding is essential for recognizing the limitations of the therapy’s advantages and the need for careful evaluation in clinical practice.
Furthermore, ongoing dialogues within the medical community are investigating whether hydralazine or nitrates alone can achieve the benefits seen with combination therapy. As we approach 2025, real-world evidence continues to affirm the effectiveness of isosorbide dinitrate in patients with cardiac issues, reinforcing its significance in comprehensive care strategies. Expert opinions, including insights from Dr. Hernandez, who has consulted for major pharmaceutical companies, emphasize the necessity for tailored strategies in cardiac management, particularly for diverse demographic groups, ensuring that treatments are both effective and equitable.
It is also vital to recognize the diversity among demographic groups, as evidenced by the 2000 Census, which revealed that 7 million individuals identified as belonging to multiple races. This statistic underscores the imperative for healthcare providers to address the unique treatment requirements of various demographic segments, particularly when implementing therapies such as hydralazine and nitrates.
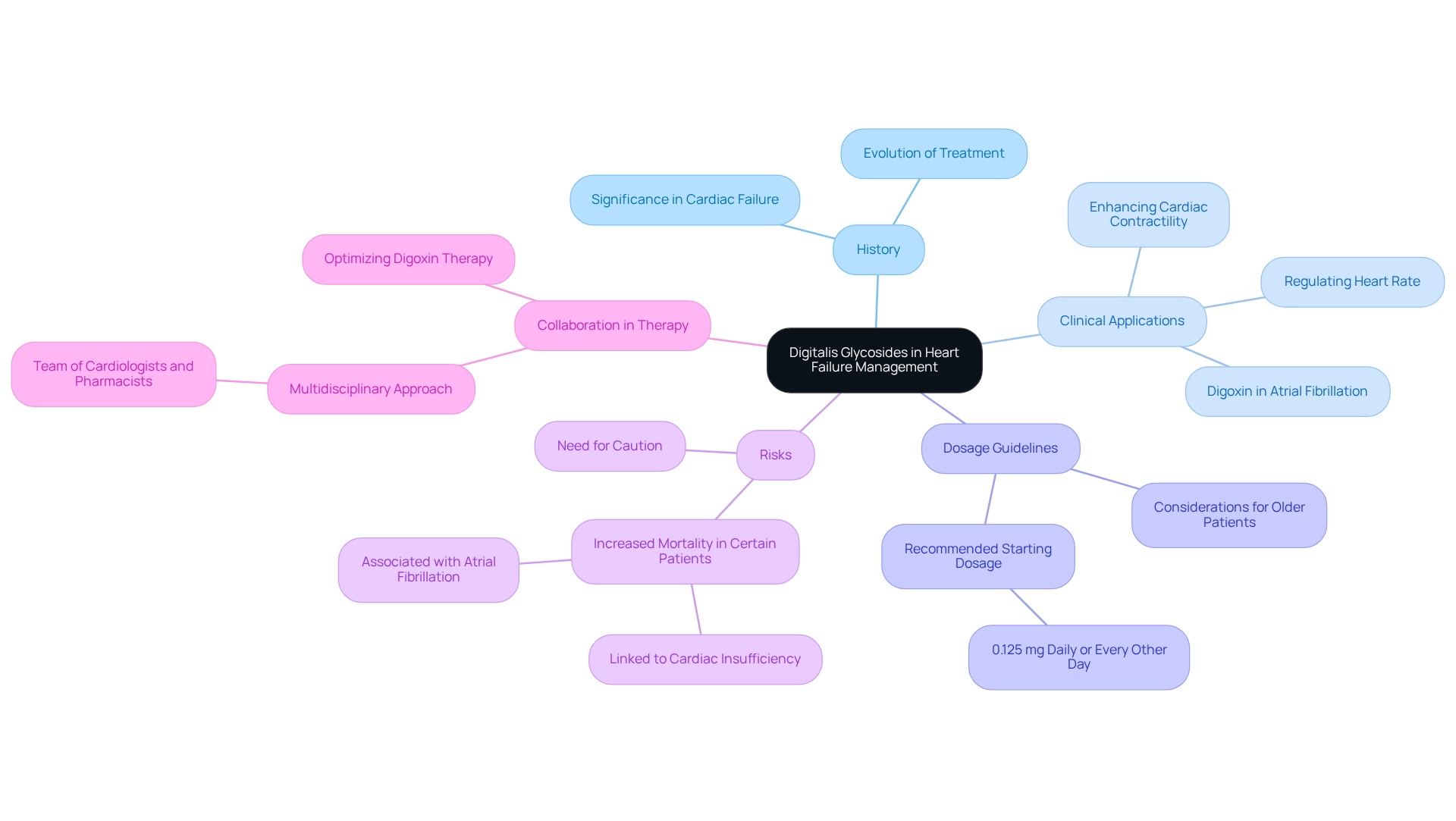
Digitalis Glycosides: Historical Yet Relevant in Heart Failure Management
Digitalis glycosides, particularly digoxin, have a significant history in treating cardiac failure, especially in patients with atrial fibrillation. These medications not only enhance cardiac contractility but also help regulate heart rate, proving their value in specific clinical scenarios. Despite the introduction of newer treatments, digoxin continues to hold importance for particular groups, especially those who exhibit inadequate responses to other gdmt medications.
A critical component of digoxin management involves a recommended low starting dosage of 0.125 mg daily or every other day for individuals aged 70 or older. This tailored approach underscores the necessity for careful consideration in treatment protocols. Although digoxin has been associated with increased mortality in patients with atrial fibrillation or cardiac insufficiency—an observation noted by cardiologist Mate Vamos, who stated, “This updated meta-analysis confirms that digoxin use is associated with increased mortality in individuals with AF or cardiac issues”—it has also demonstrated the ability to reduce hospitalizations related to exacerbated cardiac conditions, as evidenced by recent ancillary trial results.
Collaboration among healthcare professionals is essential for optimizing digoxin therapy and enhancing patient outcomes. A recent case analysis highlighted a multidisciplinary approach, where a team of cardiologists and pharmacists worked together to adjust digoxin dosages based on individual responses, resulting in improved management of cardiac symptoms and reduced hospital readmissions. As we progress through 2025, the relevance of digitalis glycosides in heart failure management remains evident, with ongoing discussions among cardiologists regarding their role in specific populations. Current expert opinions suggest that while caution is warranted, digoxin can still be a valuable component of management strategies that include gdmt medications for certain individuals. This sustained focus on digoxin emphasizes the necessity for healthcare professionals to remain informed about its benefits and risks, ensuring that patient care remains the priority in treatment strategies.
Conclusion
The management of heart failure has evolved into a sophisticated discipline, characterized by a diverse array of medications available to healthcare professionals. Each class of medication, from Angiotensin Receptor Neprilysin Inhibitors (ARNIs) to diuretics, plays a critical role within the framework of guideline-directed medical therapy (GDMT). Comprehensive data analysis, such as that from CareSet, underscores the importance of understanding treatment patterns and identifying gaps in care, ultimately driving improvements in patient outcomes.
ARNIs have revolutionized treatment approaches, significantly reducing hospitalization rates and cardiovascular mortality. Beta-blockers and ACE inhibitors remain essential, improving both survival and quality of life for patients with reduced ejection fraction. Meanwhile, ARBs and MRAs provide effective alternatives and enhancements to existing therapies, particularly for patients who experience side effects from traditional medications. The emergence of SGLT2 inhibitors further emphasizes the evolution of heart failure management, showcasing their ability to lower hospitalization risks and improve overall health status.
While diuretics offer immediate symptom relief, adjunct therapies like hydralazine and nitrates are critical for specific populations. Digitalis glycosides, despite their historical roots, continue to find relevance in targeted treatment scenarios. The commitment to ongoing research and refinement of treatment strategies is vital in addressing the complexities of heart failure management.
As the landscape of heart failure therapy continues to evolve, integrating these diverse medications into personalized treatment plans is essential. By prioritizing patient outcomes and leveraging data-driven insights, healthcare professionals can navigate the intricacies of heart failure management, ultimately enhancing the quality of care for patients facing this challenging condition.


