Overview
This article examines crucial billing guidelines for healthcare providers concerning the G2211 code, underscoring the necessity of precise documentation and compliance to enhance reimbursement strategies. It articulates best practices and highlights the critical role of comprehensive training and technology integration in optimizing billing efficiency. By doing so, it ensures that healthcare professionals adeptly navigate the intricacies of Medicare invoicing, ultimately fostering an environment conducive to improved financial outcomes.
Introduction
In the intricate world of healthcare billing, the introduction of the G2211 code by the Centers for Medicare & Medicaid Services (CMS) represents a pivotal moment for providers navigating the complexities of reimbursement for office and outpatient evaluation and management services.
This add-on code acknowledges the unique challenges faced by healthcare professionals managing patients with serious or chronic conditions, providing a pathway to improved compensation for the resources expended in complex care.
As healthcare providers contend with evolving regulations and the nuances of billing practices, grasping the implications of G2211 becomes essential—not only for financial sustainability but also for enhancing patient outcomes.
Through a comprehensive exploration of best practices, technological solutions, and collaborative strategies, stakeholders can optimize their approach to G2211 billing, ensuring that the intricacies of patient care are accurately reflected in their reimbursement processes.
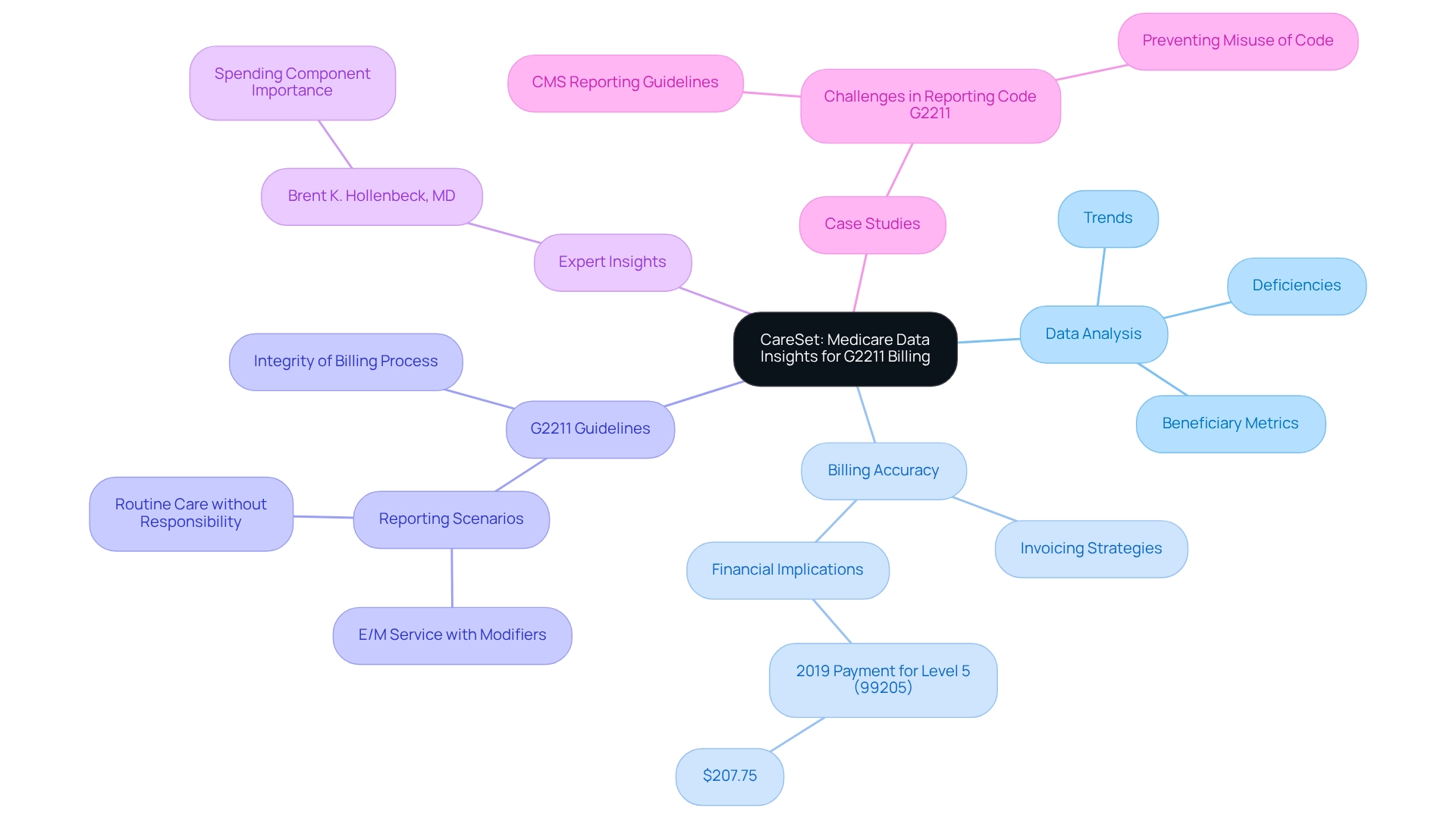
CareSet: Comprehensive Medicare Data Insights for G2211 Billing
CareSet excels in extracting and interpreting complex Medicare claims data, offering healthcare professionals vital insights into reimbursement strategies related to G2211. By examining over $1.1 trillion in yearly claims information, CareSet identifies treatment trends and data deficiencies, enabling practitioners to enhance their utilization of the add-on. This data-driven approach not only improves invoicing accuracy but also empowers providers to manage the complexities of Medicare invoicing with confidence.
The significance of the physician-patient relationship is underscored in the context of continuous care for serious and intricate conditions, making precise invoicing essential. Recent statistics reveal that the total payment for new patient level 5 (99205) in 2019 was $207.75, emphasizing the financial implications of effective invoicing practices.
Expert opinions highlight the increasing importance of spending metrics at the beneficiary level. As noted by Brent K. Hollenbeck, MD, as Medicare intensifies the weight of the spending component, it increasingly influences policy outcomes. CareSet’s insights into G2211 billing guidelines are further enriched by case studies that clarify the appropriate application of G2211. For instance, the G2211 billing guidelines outlined by CMS specify situations where this identifier should not be reported, such as when an E/M service is billed with certain payment modifiers or when the care provided is routine without ongoing responsibility. These clarifications aim to prevent misuse of the code, ensuring the integrity of the payment process for complex care.
Moreover, the recent changes in time descriptors do not affect how practices report E/M service levels based on total time, providing additional context for healthcare professionals navigating payment practices. By leveraging extensive Medicare data analysis, CareSet not only enhances billing strategies but also fosters long-term growth for healthcare professionals, ultimately improving patient outcomes. This comprehensive approach empowers healthcare stakeholders with insights derived from the experiences of over 62 million beneficiaries and 6 million providers, ensuring that CareSet remains a leading provider of Medicare data analysis and patient care insights.
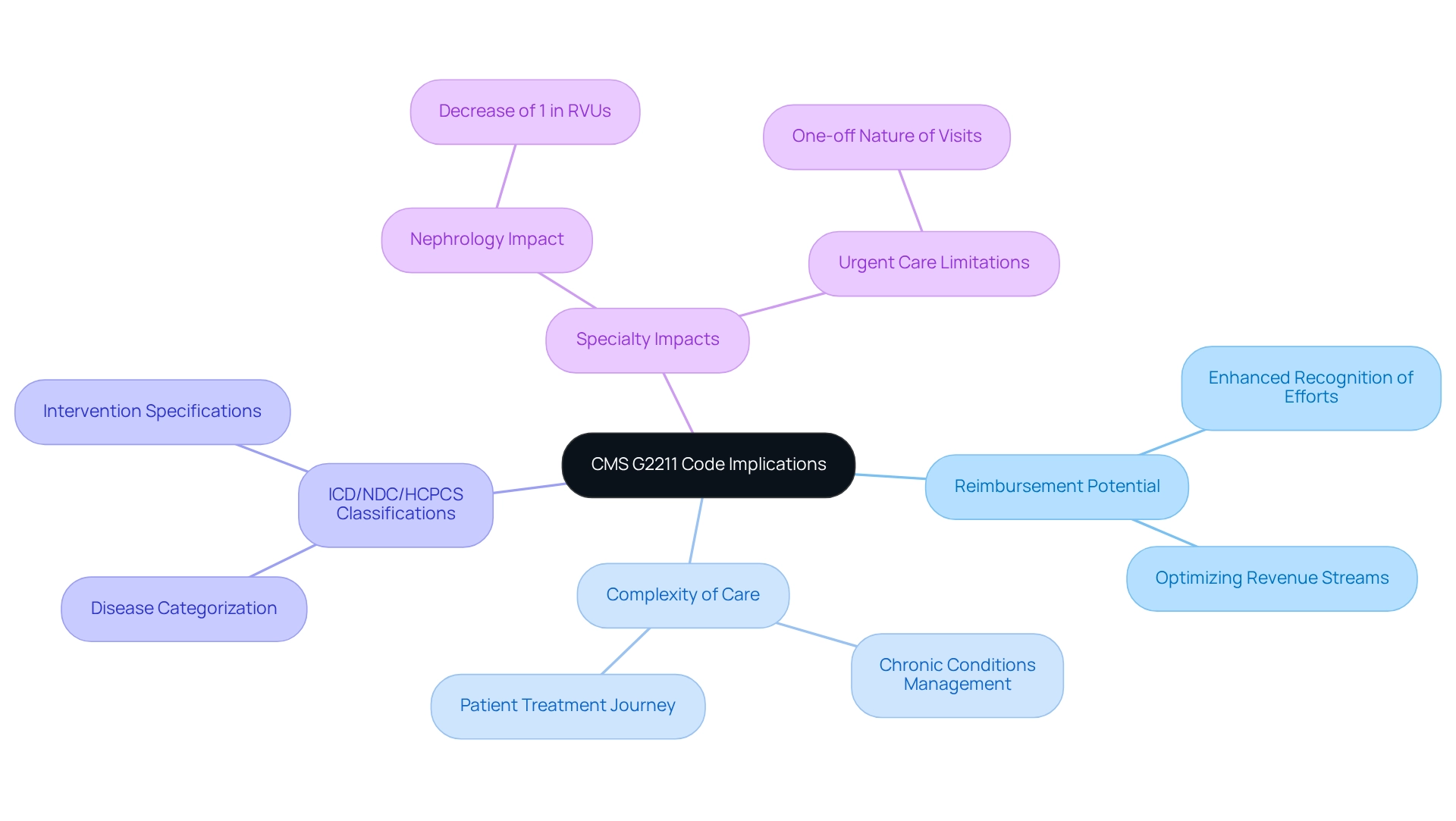
CMS G2211 Code: Key Implications for Healthcare Providers
The G2211 designation, introduced by the Centers for Medicare & Medicaid Services (CMS), serves as an add-on for office and outpatient evaluation and management (E/M) services. It acknowledges the complexity of care provided during these visits, particularly for patients with serious or chronic conditions. This complexity is elucidated through the application of ICD classifications that categorize diseases, alongside NDC and HCPCS identifiers that specify particular interventions. For healthcare providers, this translates to the potential for additional reimbursement for the time and resources dedicated to managing complex patient needs throughout their treatment journey. Recent updates indicate that the implementation of this system is expected to enhance recognition of the efforts involved in managing such patients, thereby improving reimbursement rates. Notably, the anticipated effect on Nephrology suggests a reduction of 1% in relative value units (RVUs), highlighting the nuanced impacts of this classification across various specialties and the importance of understanding how different classifications interact within the therapeutic domain.
However, it is essential to note that this classification may not apply to the majority of urgent care center visits, given the distinct nature of those encounters, as outlined by CMS. Understanding the intricacies of the g2211 billing guidelines is vital for healthcare professionals aiming to ensure compliance and optimize their revenue streams. As the healthcare landscape evolves, staying informed about the g2211 billing guidelines and the implications of new legislation, particularly regarding Medicare claims data and treatment approvals, will be crucial for maximizing reimbursement opportunities and effectively managing the complexities of patient care. Furthermore, CMS has finalized changes to the coding and valuation of E/M services, which are anticipated to enhance the acknowledgment of the work involved in managing complex patients and improve reimbursement for providers.
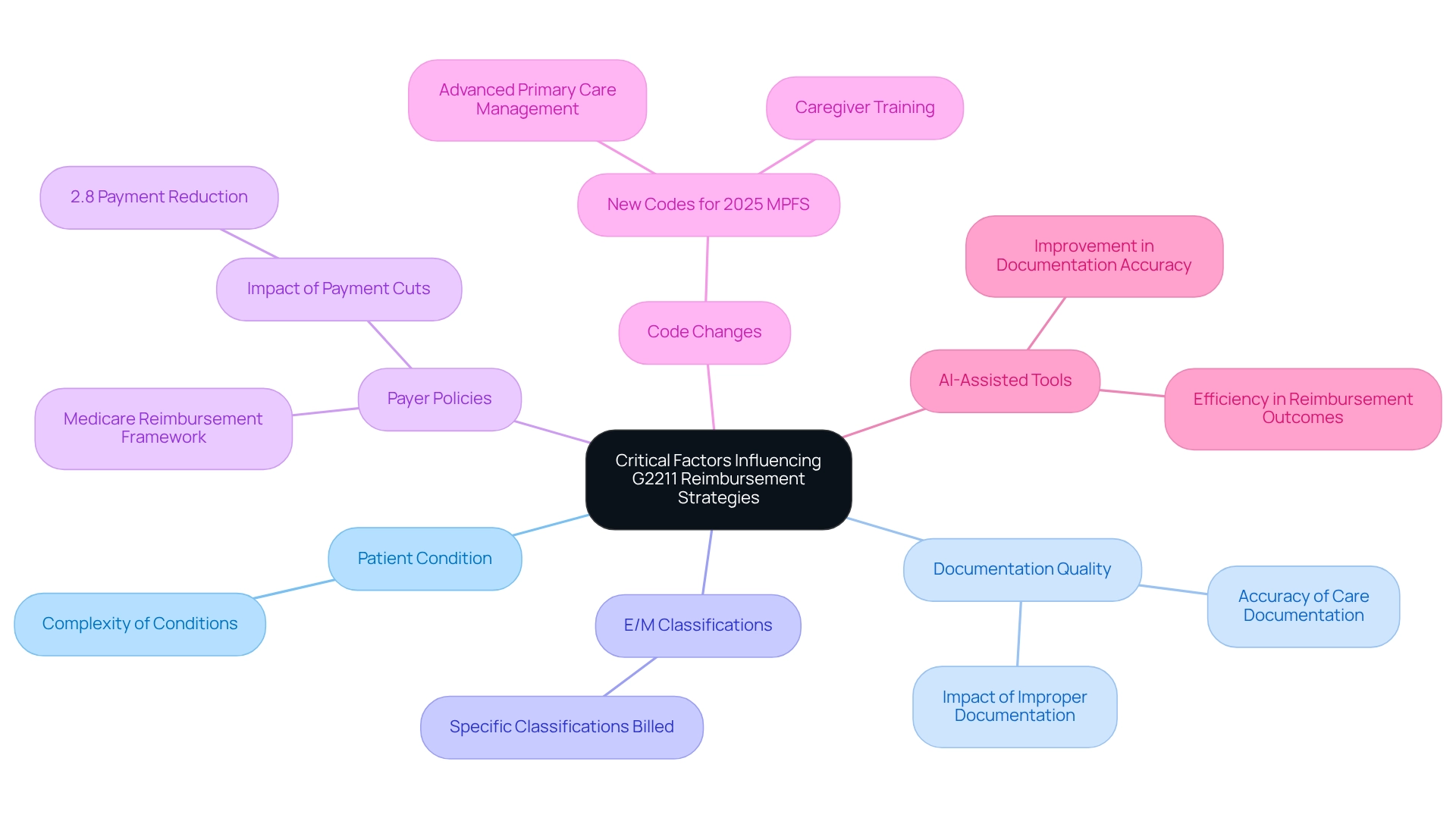
Critical Factors Influencing G2211 Reimbursement Strategies
Multiple essential elements influence the g2211 billing guidelines for reimbursement strategies. These include the intricacy of the patient’s condition, the comprehensiveness of care documentation, and the specific Evaluation and Management (E/M) classifications billed according to the g2211 billing guidelines. Accurate documentation is paramount; it must clearly illustrate the ongoing patient-provider relationship and the intricacies of the care delivered. In 2025, the introduction of new codes for Advanced Primary Care Management and caregiver training under the Medicare Physician Fee Schedule (MPFS) presents both opportunities and challenges. While these changes can enhance revenue potential, they also necessitate robust practice management systems to navigate the accompanying administrative complexities.
Moreover, understanding payer policies and the nuances of Medicare’s reimbursement framework is essential for optimizing revenue. For instance, the recent 2.8% decrease in Medicare physician payments, representing the fifth consecutive reduction, underscores the urgency for practitioners to enhance their charging strategies. Industry experts emphasize that such reductions can jeopardize practice viability and exacerbate physician workforce shortages, ultimately impacting patient access to care.
Documentation accuracy is another pivotal aspect, with statistics indicating that improper documentation can lead to significant revenue losses. Optimal procedures for this code invoicing, in line with g2211 billing guidelines, involve maintaining thorough documentation of patient interactions, treatment strategies, and any pertinent clinical information that justifies the need for the services provided. Case studies reveal that practices employing AI-assisted tools for documentation have seen improvements in both accuracy and efficiency, further enhancing their reimbursement outcomes. By prioritizing these factors, healthcare professionals can better navigate the complexities of billing and enhance their financial sustainability.
Utilizing the G2211 Add-On Code: Best Practices for Billing Accuracy
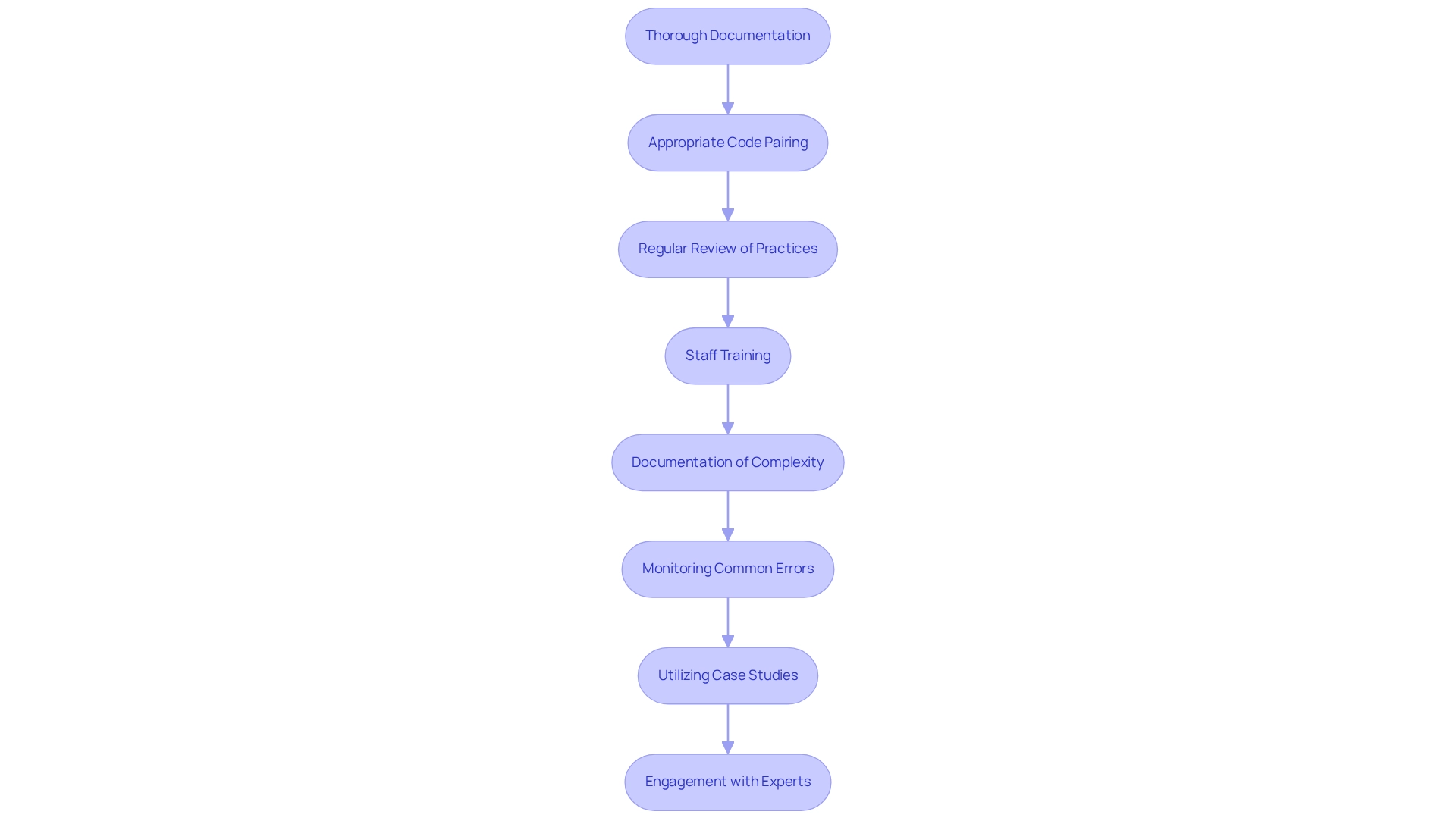
To effectively utilize the G2211 add-on code, healthcare providers must adhere to the following best practices:
-
Thorough Documentation: It is imperative to clearly document the patient’s condition and the complexity of care provided. This is essential for validating the application of the specific designation and ensuring appropriate reimbursement.
-
Appropriate Code Pairing: Bill the G2211 code alongside pertinent Evaluation and Management (E/M) codes (99202-99215) to qualify for additional reimbursement, thereby enhancing the overall accuracy of charges.
-
Regular Review of Practices: Continuously review and update invoicing practices to ensure compliance with the latest CMS guidelines and payer requirements. This proactive approach can help mitigate the risk of denials.
-
Staff Training: Provide comprehensive training for personnel on the intricacies of the specified invoicing system. Such training will assist in reducing mistakes and enhancing the overall efficiency of the invoicing process.
-
Documentation of Complexity: Clearly indicate the complexity of care in the documentation to support the use of the specific code, particularly in team-based and urgent care settings.
-
Monitoring Common Errors: Be vigilant about frequent mistakes in this specific invoicing, such as insufficient documentation or erroneous code pairing, as these can significantly affect reimbursement outcomes.
-
Utilizing Case Studies: Learn from real-world examples of successful practices in the specified area to identify effective strategies and avoid pitfalls. For instance, the case study titled ‘CMS Guidance on G2211 Billing Guidelines’ discusses challenges in documentation and the implications of the G2211 billing guidelines in team-based care.
-
Engagement with Experts: Consult with billing experts to gain insights into best practices and stay informed about evolving regulations and compliance requirements. PYA provides on-demand webinars on the CMS 2025 proposed rules, which can serve as a valuable resource for practitioners.
By utilizing this system appropriately, providers can ensure proper reimbursement and contribute to the overall understanding of patient care complexities.
Integrating G2211 with Existing Billing Codes: A Practical Guide
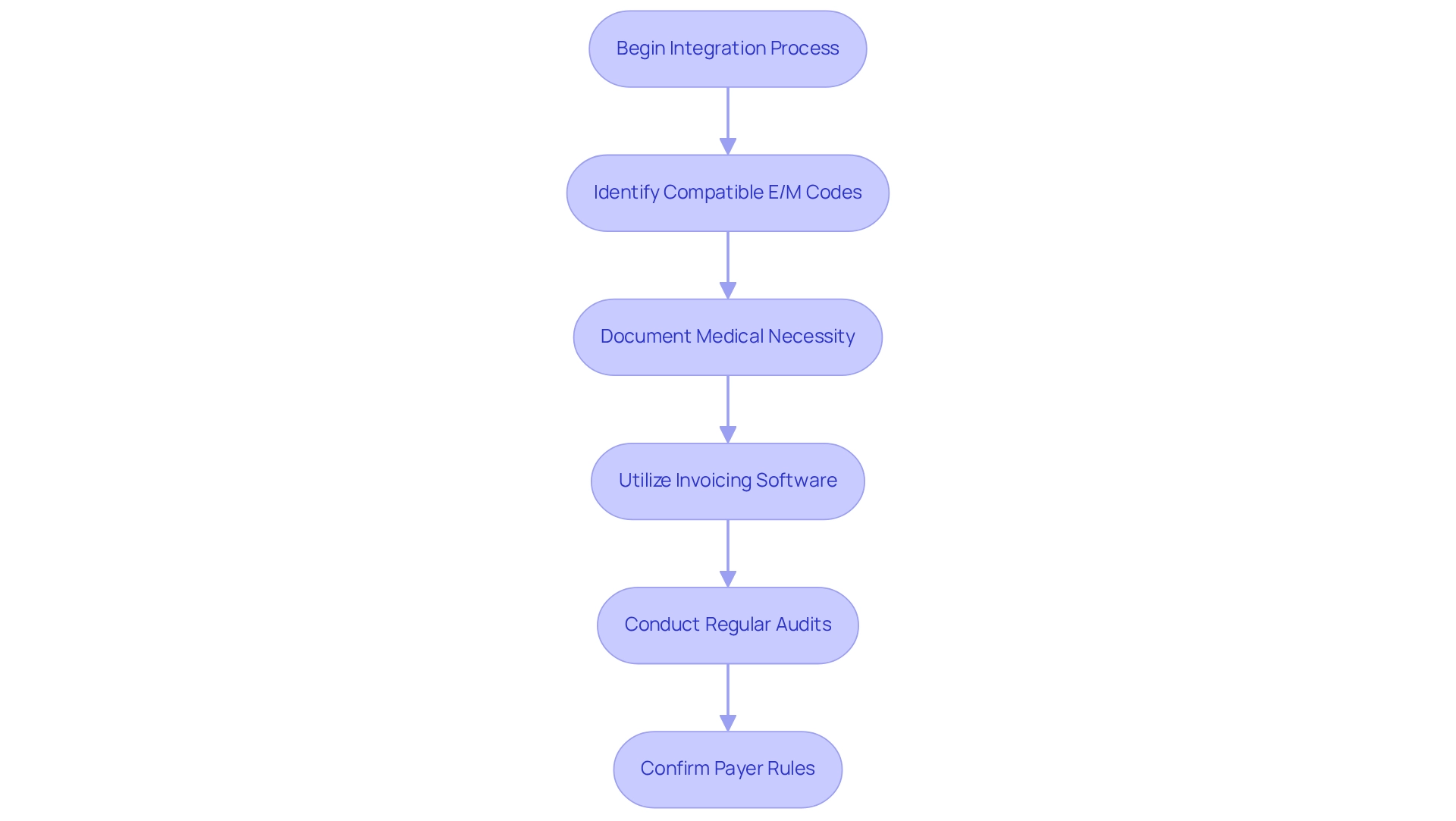
Incorporating this designation with current billing systems necessitates a systematic approach to enhance efficiency and adherence. Statistics indicate that the integration of specific services with Evaluation and Management (E/M) classifications is increasingly significant, with an anticipated rise in overall RVU output by 1% for urology services. This underscores the necessity of adapting to new billing classifications.
To begin, identify compatible E/M codes by determining which can be billed alongside the specified code. This step is crucial for ensuring that all services rendered are appropriately captured. Next, document medical necessity clearly for both the E/M service and the additional add-on. This documentation not only facilitates invoicing but also conforms to payer requirements, thereby minimizing the risk of denials while following the g2211 billing guidelines. Utilizing supportive invoicing software can greatly enhance the integration of G2211 with other codes. Such tools streamline the invoicing process, making claims management and tracking reimbursements more efficient. Additionally, conducting regular audits is essential for maintaining adherence to payment practices and identifying areas for improvement. These audits assist healthcare providers in adapting to modifications in payment guidelines and enhancing their overall revenue cycle management.
Case studies illustrate the positive impact of this treatment on physician payments, demonstrating how its introduction addresses the complexities of managing chronic conditions. As Mark Edney, MD, noted, Medicare anticipates that RVU adjustments for urology will lead to this rise alongside a comparable volume of services, including the introduction of the new code. By embracing a structured method for integration, healthcare professionals can navigate the evolving reimbursement landscape more effectively. It is imperative to confirm all information with specific payer rules to ensure compliance and precision in invoicing practices.
Staying Compliant: Navigating Changes in G2211 Billing Regulations
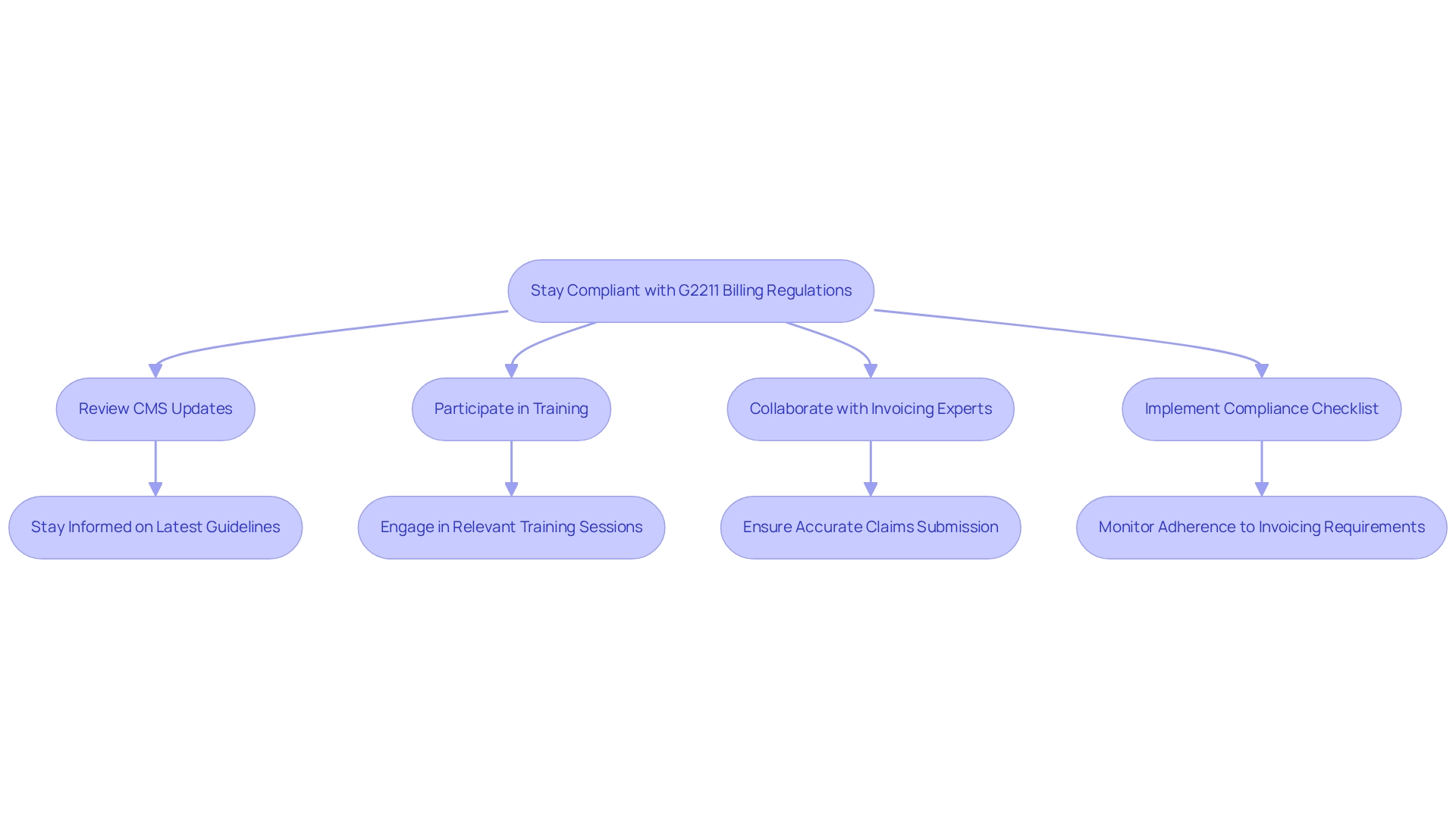
Healthcare professionals must stay abreast of changes in payment regulations to ensure compliance and optimize reimbursement. Recent updates to coding aim to more effectively recognize the complexities of primary care services, ensuring appropriate compensation for those managing patients’ comprehensive health needs. Key strategies include:
- Regularly Reviewing CMS Updates: It is essential to remain informed about the latest guidelines from the Centers for Medicare & Medicaid Services (CMS) to navigate the evolving landscape of coding effectively.
- Participating in Training Sessions: Engaging in training sessions and webinars focused on relevant practices equips providers with the necessary knowledge to adapt to regulatory changes.
- Collaborating with Invoicing Experts: Close collaboration with invoicing specialists guarantees that all claims are submitted accurately and in compliance with current regulations, thereby minimizing errors.
- Implementing a compliance checklist aids in monitoring adherence to invoicing requirements, facilitating a systematic approach to managing g2211 billing guidelines.
Moreover, the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) established the Quality Payment Program (QPP), underscoring the importance of adherence in invoicing practices. A case study on Medicare Improper Payment Review highlights the critical need for precise invoicing to reduce improper payments and ensure effective utilization of Medicare funds.
These strategies not only bolster compliance but also enhance the overall efficiency of financial operations, ultimately contributing to improved patient care and financial performance. For optimal outcomes, providers should routinely evaluate their compliance strategies and adapt them based on the latest CMS updates and industry best practices.
Staff Training: Essential G2211 Billing Guidelines for Healthcare Teams
To ensure accurate g2211 billing guidelines, healthcare teams must engage in thorough training that covers several key components. First, comprehending the classification is essential. Teams should grasp the significance of this classification, particularly its application to office and outpatient evaluation and management (E/M) visits, including numbers 99202-99205 and 99211-99215.
Second, best practices for documentation must be emphasized. Training should focus on effective documentation strategies that align with specified requirements, ensuring compliance and precision in invoicing. As Mark Painter notes, “If documentation supports a modifier -22 may be added to the 52353 or 52356 if multiple stones are treated on the same side using a laser to treat both stones,” highlighting the importance of precise documentation in complex cases.
Third, integration with other charge codes is crucial. Staff must become familiar with how G2211 interacts with other charge codes, particularly in complex cases such as vasectomy procedures, where coding confusion often arises. This knowledge gap is essential for efficient invoicing practices.
Lastly, regular training refreshers are vital. Ongoing education helps keep staff updated about changes in regulations and payment practices, particularly considering recent modifications finalized by CMS to enhance access to services.
Incorporating case studies on successful staff training initiatives can further illustrate the effectiveness of these programs. For example, a recent study named “Cost RVU Changes in Urology” suggested that practices adopting organized training experienced a significant rise in invoicing precision and efficiency. Anticipated alterations to Relative Value Units (RVUs) are expected to lead to a 1% increase in total RVU output.
Furthermore, expert perspectives from healthcare instructors highlight that effective coding education not only improves compliance but also increases overall team confidence in financial practices.
Statistics indicate that organizations emphasizing training related to g2211 billing guidelines experience a notable decrease in invoicing mistakes. This underscores the importance of thorough education for healthcare teams in 2025 and beyond. By concentrating on these crucial training aspects, healthcare professionals can enhance their invoicing methods and improve patient care results.

Technology Solutions: Enhancing G2211 Billing Efficiency
Healthcare providers can significantly enhance their efficiency by leveraging advanced technology solutions in accordance with the G2211 billing guidelines.
Electronic Health Record (EHR) Systems: EHRs specifically designed to support invoicing streamline documentation and ensure compliance with invoicing guidelines. These systems facilitate accurate coding and reduce the risk of errors, ultimately enhancing revenue cycle management. The inclusion of the new code as part of the Medicare 2024 Physician Fee Schedule underscores the importance of EHR systems in adapting to the complexities of ongoing patient care. Implementing invoicing software that automates the integration of the G2211 billing guidelines with other pertinent references can significantly reduce manual entry mistakes and accelerate the invoicing process. This technology ensures that all essential codes are captured effectively, thereby enhancing overall accuracy in charges.
Data Analytics Tools: Employing data analytics tools allows healthcare providers to track financial trends and identify areas for enhancement. By examining invoicing data, organizations can uncover inefficiencies and refine their invoicing practices, leading to improved financial outcomes.
Staff Training Programs: Investing in comprehensive training for staff on the use of these technologies is crucial. Ensuring that team members are proficient in utilizing EHR systems and invoicing software maximizes the effectiveness of these tools and enhances overall financial efficiency. Expert opinions indicate that adopting these technologies not only aids adherence to new coding standards but also promotes long-term financial well-being for healthcare organizations.
The adoption of EHR systems has been shown to substantially improve invoicing processes, as evidenced by various case studies that showcase successful transitions to more effective invoicing practices. For example, the case study titled

Data Analysis: Evaluating G2211 Billing Practices for Continuous Improvement
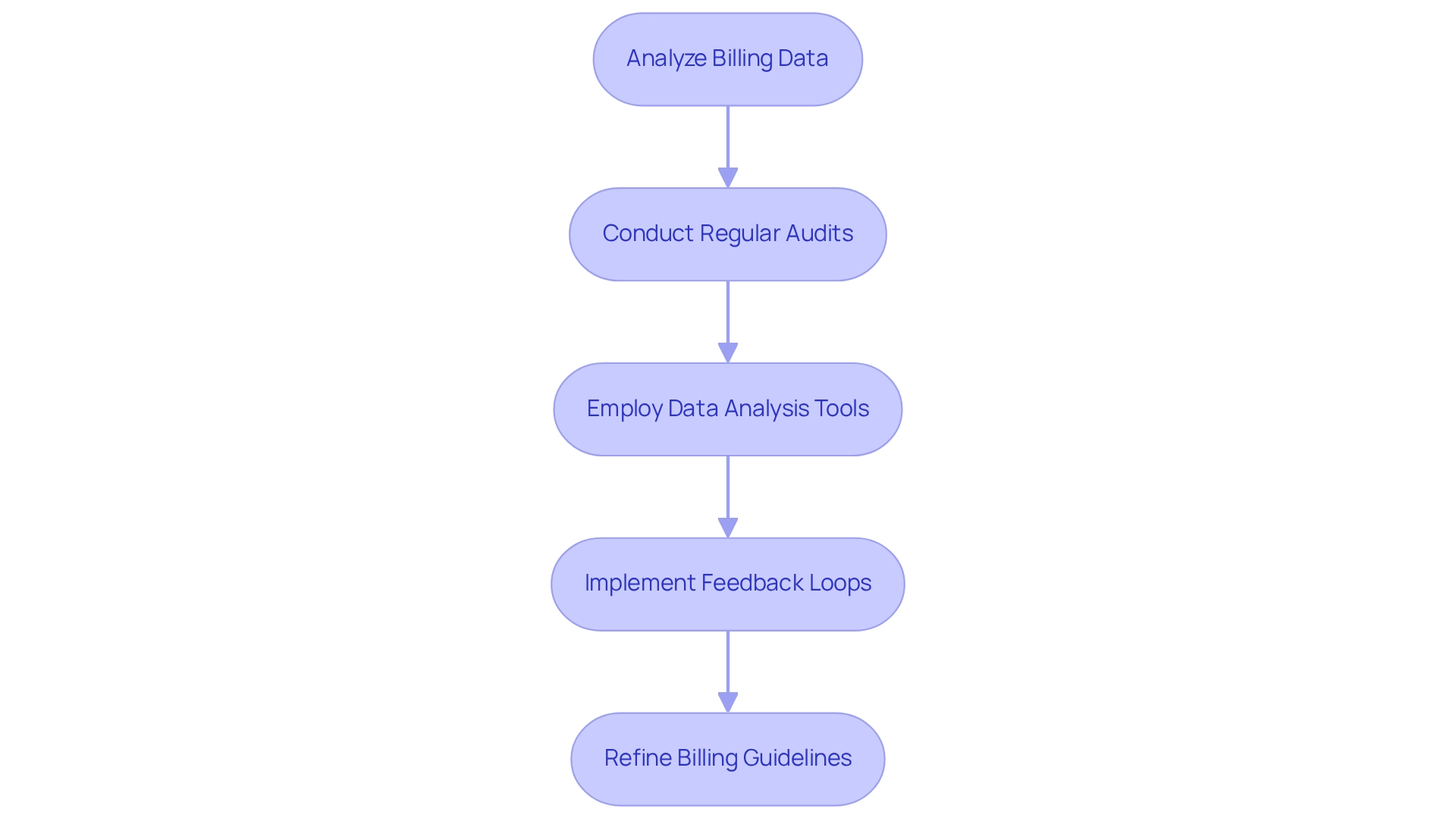
To effectively assess financial practices, healthcare professionals must adopt a systematic method that leverages innovative Medicare data solutions from CareSet. This approach enhances pharmaceutical strategies through comprehensive insights and patient journey mapping. Key steps include:
- Analyzing billing data in accordance with g2211 billing guidelines to identify trends in usage and reimbursement rates, revealing patterns that inform strategic adjustments. CareSet’s monthly Medicare updates deliver critical insights into drug utilization and treatment pathways, enabling providers to make informed decisions about patient navigation from diagnosis to treatment.
- Conducting regular audits to assess the accuracy of claims under the g2211 billing guidelines ensures compliance and minimizes the risk of denials. As Stephani Scott, vice president of AAPC Services, emphasizes, accurate health information management is crucial for compliance.
- Employing sophisticated data analysis tools, supported by CareSet’s combination of more than 100 external data sources, to pinpoint specific areas for enhancement in invoicing practices. This allows for focused interventions that improve efficiency.
- Implementing feedback loops that facilitate the ongoing improvement of invoicing strategies based on real-time data insights, fostering an adaptive management approach. As Tim O’Reilly noted, “We’re entering a new world in which data may be more important than software.”
By concentrating on these methods, healthcare providers can refine their g2211 billing guidelines for charges, ultimately enhancing patient outcomes and boosting financial performance. This comprehensive approach not only addresses immediate data needs but also fosters long-term strategic growth for healthcare partners, as illustrated in various case studies demonstrating the practical impact of CareSet’s solutions.
Stakeholder Collaboration: Optimizing G2211 Billing Strategies
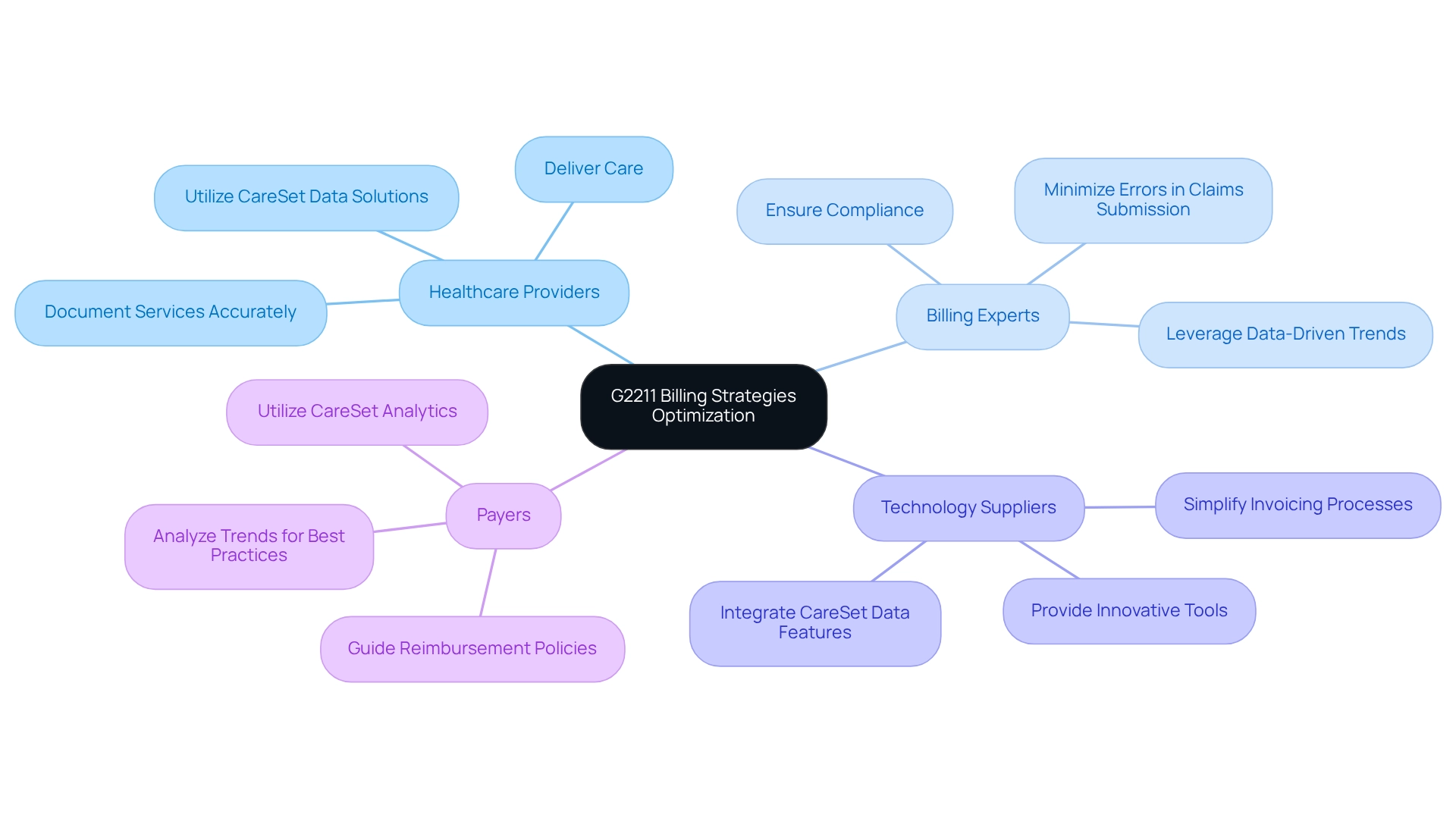
Effective optimization of financial strategies according to the G2211 billing guidelines hinges on robust collaboration among key stakeholders, each playing a vital role in the process.
-
Healthcare Providers are responsible for delivering care and accurately documenting services, ensuring that the charges reflect the true nature of patient interactions. Insights from CareSet’s extensive Medicare data solutions can assist healthcare professionals in grasping payment intricacies and enhancing documentation precision.
-
Billing Experts concentrate on compliance and precision in claims submission, navigating the complexities of invoicing regulations to minimize errors. Data-driven trends from CareSet can inform their strategies, leading to more effective claims management.
-
Technology Suppliers offer innovative tools and software that simplify invoicing processes, making it easier for practitioners and claims specialists to handle claims effectively. CareSet’s data integration features improve these tools, ensuring they align with the most recent payment practices.
-
Payers provide insights into reimbursement policies and trends, guiding stakeholders on best practices for invoicing and ensuring that practitioners are compensated fairly. CareSet’s analytics on over 62 million beneficiaries and 6 million providers offer valuable context for payers to refine their reimbursement strategies.
Fostering open communication among these groups is essential. Recent modifications in CPT coding descriptions for E/M services, which outline minimum durations for each service level, emphasize the necessity for clear communication to guarantee that all parties comprehend the consequences for payment practices. Statistics suggest that up to 38 percent of all E/M services in 2024 will include charges, highlighting the need for stakeholders to collaborate efficiently. Effective communication techniques can result in better financial outcomes, as demonstrated by case studies showcasing increased clarity in payment processes and equitable compensation for practitioners based on the time spent with patients.
Incorporating expert opinions on stakeholder collaboration can further illuminate effective strategies. Healthcare leaders stress that optimizing invoicing processes necessitates not only precise documentation but also a commitment to continuous communication among providers, payment specialists, technology vendors, and payers. This collaborative approach ultimately enhances the success of the G2211 billing guidelines and improves patient care outcomes.
Conclusion
The introduction of the G2211 code signifies a transformative shift in the billing practices for office and outpatient evaluation and management services. This code acknowledges the complexities inherent in managing patients with serious or chronic conditions, thereby enhancing reimbursement opportunities and underscoring the necessity for accurate documentation and compliance with evolving regulations.
Key strategies for optimizing G2211 billing have been outlined, emphasizing the critical need for thorough documentation, regular reviews of billing practices, and the integration of technology solutions. By leveraging tools such as Electronic Health Records and automated billing software, healthcare providers can streamline processes, minimize errors, and ensure that all services rendered are accurately captured. Moreover, the significance of staff training and stakeholder collaboration is paramount, as these elements are essential for fostering an environment of compliance and efficiency.
Ultimately, the successful implementation of the G2211 code relies on a proactive approach to billing practices. By adopting best practices, embracing technological advancements, and collaborating effectively with all stakeholders, healthcare providers can navigate the complexities of G2211 billing while enhancing patient care outcomes and ensuring financial sustainability. As the healthcare landscape evolves, remaining informed and adaptable will be crucial for maximizing the benefits of this pivotal coding change.


