Overview
The article delves into the implications and key insights of the 3-Day Hospital Stay Medicare Rule, a critical determinant for eligibility in skilled nursing facilities (SNFs) that significantly impacts healthcare costs. Understanding inpatient status, exceptions to the rule, and the categorization of hospital stays is essential, as these factors profoundly influence patient care and access to necessary services within the Medicare system. As we explore these elements, it becomes clear that a comprehensive grasp of this rule is vital for navigating the complexities of Medicare and ensuring optimal patient outcomes.
Introduction
In the intricate landscape of Medicare, the 3-Day Hospital Stay Rule stands as a pivotal factor that significantly influences patient access to skilled nursing facilities and the broader healthcare system. CareSet is at the forefront of Medicare data analysis, offering invaluable insights derived from extensive claims data. This empowers stakeholders to adeptly navigate the complexities surrounding this rule. Given its profound implications for patient care, coverage eligibility, and healthcare costs, a nuanced understanding of inpatient and outpatient statuses is more essential than ever.
As the healthcare community confronts evolving regulations and disparities in care access, this article explores the intricacies of the 3-Day Rule, its exceptions, and the classifications of hospital stays. Ultimately, it illuminates how these elements shape the future of Medicare coverage and patient outcomes.
CareSet: Comprehensive Medicare Insights on the 3-Day Hospital Stay Rule
CareSet has positioned itself as a leader in healthcare data analysis, particularly regarding the complexities of the 3 day hospital stay medicare rule. By meticulously analyzing extensive claims data from over 62 million beneficiaries and 6 million providers, CareSet provides stakeholders with actionable insights that are essential for navigating the intricacies of Medicare coverage. This expertise is increasingly vital as the 3 day hospital stay medicare significantly influences access to skilled nursing facilities (SNFs) and affects overall healthcare costs.
Recent discussions within the healthcare community underscore the transformative nature of this rule, with experts highlighting its considerable implications for individual treatment and facility operations. CareSet’s unwavering commitment to transparency and precision ensures that clients receive reliable information, empowering them to make informed decisions that enhance health outcomes and optimize resource allocation.
Through its comprehensive approach, CareSet not only addresses immediate data needs but also supports long-term strategic development for healthcare partners, ultimately fostering improved individual wellbeing and operational efficiency.
Inpatient Status: Importance and Implications for Medicare Coverage
Inpatient status is critical for health insurance coverage, significantly influencing eligibility for various benefits, including skilled nursing facility (SNF) services. To qualify for coverage of SNF services, patients must have a 3 day hospital stay Medicare as inpatients for at least three consecutive days. This requirement ensures that the assistance provided is medically necessary, justifying the associated costs. As we approach 2025, understanding this distinction is increasingly vital, as it directly affects treatment decisions and financial responsibilities for both healthcare providers and patients.
Current data indicates that a substantial number of Medicare beneficiaries qualify for skilled nursing facility services, underscoring the importance of precise documentation of inpatient status. For example, socioeconomic factors have demonstrated a correlation with hospitalization rates, revealing that individuals in lower-income communities face a 19% higher hospitalization rate compared to their wealthier counterparts. This disparity highlights the urgent need for targeted interventions and the critical importance of ensuring that individuals secure appropriate inpatient status to access essential care.
Statistics show that the average inflation-adjusted charges per hospital stay have surged, reflecting the escalating costs of healthcare. This trend emphasizes the significance of inpatient status not only for individual treatment but also for effectively managing healthcare costs, particularly concerning the 3 day hospital stay Medicare. Healthcare providers must adeptly navigate these complexities to optimize benefits for their patients, ensuring compliance with necessary criteria for coverage while also addressing the financial ramifications of inpatient admissions.
Exceptions to the 3-Day Hospital Stay Rule: What You Should Know
While the 3 day hospital stay Medicare rule serves as a standard requirement, notable exceptions exist that can facilitate access to skilled nursing services, particularly within the intricate treatment pathways of Medicare. For example, during public health crises like the COVID-19 pandemic, the Centers for Medicaid Services (CMS) enacted waivers that allowed beneficiaries to access skilled nursing facility (SNF) care without meeting the three-day inpatient requirement. This flexibility is crucial, as it empowers providers to navigate client journeys more effectively, ensuring timely access to essential services. Additionally, certain Advantage plans may bypass this rule under specific conditions, underscoring the importance of understanding these exceptions.
By analyzing healthcare claims data alongside associated codes (ICD, NDC, HCPCS), providers can enhance care delivery and guarantee that patients receive necessary services without unnecessary delays.
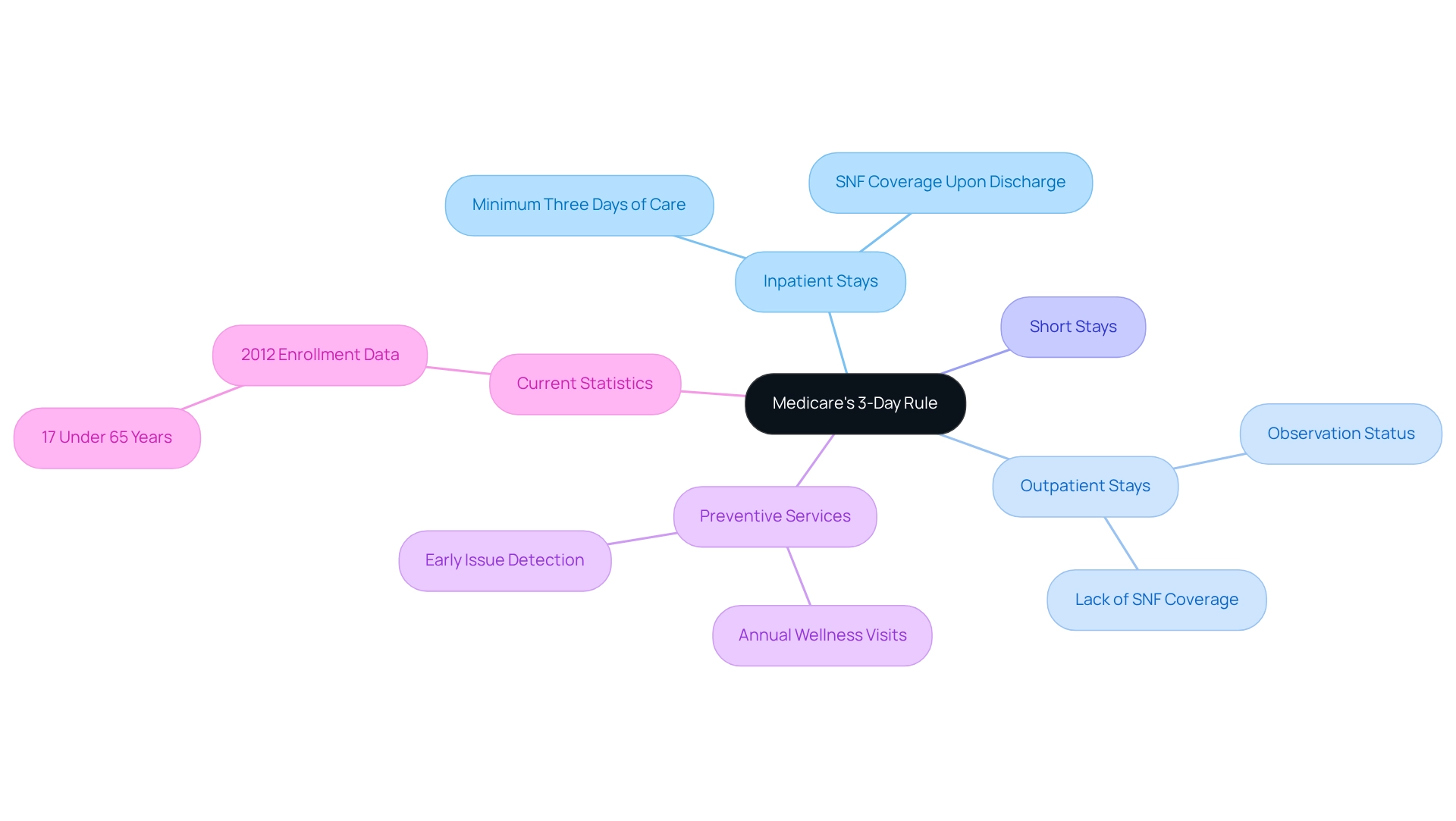
Categories of Hospital Stays: Navigating Medicare’s 3-Day Rule
Navigating the 3-Day Hospital Admission Rule necessitates a comprehensive understanding of how the health insurance program categorizes hospital visits. Medicare distinctly differentiates between inpatient and outpatient periods, each carrying significant implications for coverage. Inpatient admissions occur when an individual is officially admitted and requires a minimum of three days of care, which qualifies them for 3 day hospital stay Medicare coverage for skilled nursing facility (SNF) upon discharge. In contrast, outpatient stays may involve observation status, which does not fulfill the criteria for SNF coverage, potentially leaving individuals without essential benefits.
As we move into 2025, the classification of hospital stays continues to evolve, with certain hospitalizations categorized as ‘short stays’ or ‘observation stays.’ These classifications can complicate eligibility for healthcare benefits, making it crucial for both patients and providers to grasp the nuances of these categories. For instance, a case study on optimizing healthcare benefits underscores the importance of utilizing preventive services, such as annual wellness visits, to maintain health and identify potential issues early.
Current statistics reveal that in 2012, individuals under 65 years enrolled in the program represented 17 percent of the overall population, emphasizing the diverse demographic reliant on these classifications. Expert opinions underscore that understanding the distinctions between inpatient and outpatient stays is vital for effectively navigating Medicare coverage. As healthcare analysts observe, the implications of these distinctions can profoundly impact patient care and access to necessary services.
Conclusion
The complexities surrounding the 3-Day Hospital Stay Rule are integral to understanding Medicare coverage and patient access to essential healthcare services. CareSet’s extensive analysis of claims data provides crucial insights that empower stakeholders to navigate these intricacies effectively. Recognizing the importance of inpatient status for skilled nursing facility eligibility underscores significant implications for patient care and financial responsibilities within the healthcare system.
Exceptions to the 3-Day Rule, particularly during public health emergencies, illustrate the flexibility required in Medicare’s approach to care delivery. Understanding these exceptions, alongside the categorization of hospital stays, is vital for both patients and providers to ensure timely access to necessary services. As healthcare continues to evolve, staying informed about these nuances will be essential for optimizing care and managing costs.
In conclusion, a nuanced understanding of the 3-Day Hospital Stay Rule and its implications is indispensable for improving patient outcomes and navigating the Medicare landscape. Stakeholders must remain informed and proactive in their approach to ensure that patients receive the care they need without unnecessary barriers. The future of Medicare coverage and patient care hinges on this knowledge, making it imperative for all involved to prioritize education and advocacy in this critical area of healthcare.


