Overview
The article highlights the crucial insights surrounding the significance of attaining a 5-star rating in the CMS (Centers for Medicare & Medicaid Services) Star Ratings system, a vital component for healthcare success. It asserts that organizations that adeptly utilize comprehensive Medicare data and implement effective quality improvement strategies can markedly elevate their ratings. This enhancement not only leads to improved patient outcomes but also results in increased revenue and a competitive advantage in the healthcare landscape.
Introduction
In the intricate realm of healthcare, attaining high CMS Star Ratings stands as a pivotal goal for providers intent on enhancing patient care and ensuring financial viability. These ratings not only shape consumer decisions but also have a direct bearing on reimbursement rates and market competitiveness.
With the advent of sophisticated data analytics, organizations now have the capacity to extract invaluable insights from extensive Medicare claims data, enabling them to pinpoint performance deficiencies and refine care delivery.
As the healthcare landscape continues to evolve, grasping the nuances of the CMS Five-Star Quality Rating System and harnessing comprehensive data insights will be crucial for organizations striving to elevate their ratings and improve patient outcomes.
The path to excellence in healthcare is laden with challenges; however, the strategic application of data offers a transformative opportunity for providers to enhance their services and succeed in an increasingly competitive arena.
CareSet: Comprehensive Medicare Data Insights for CMS Star Ratings
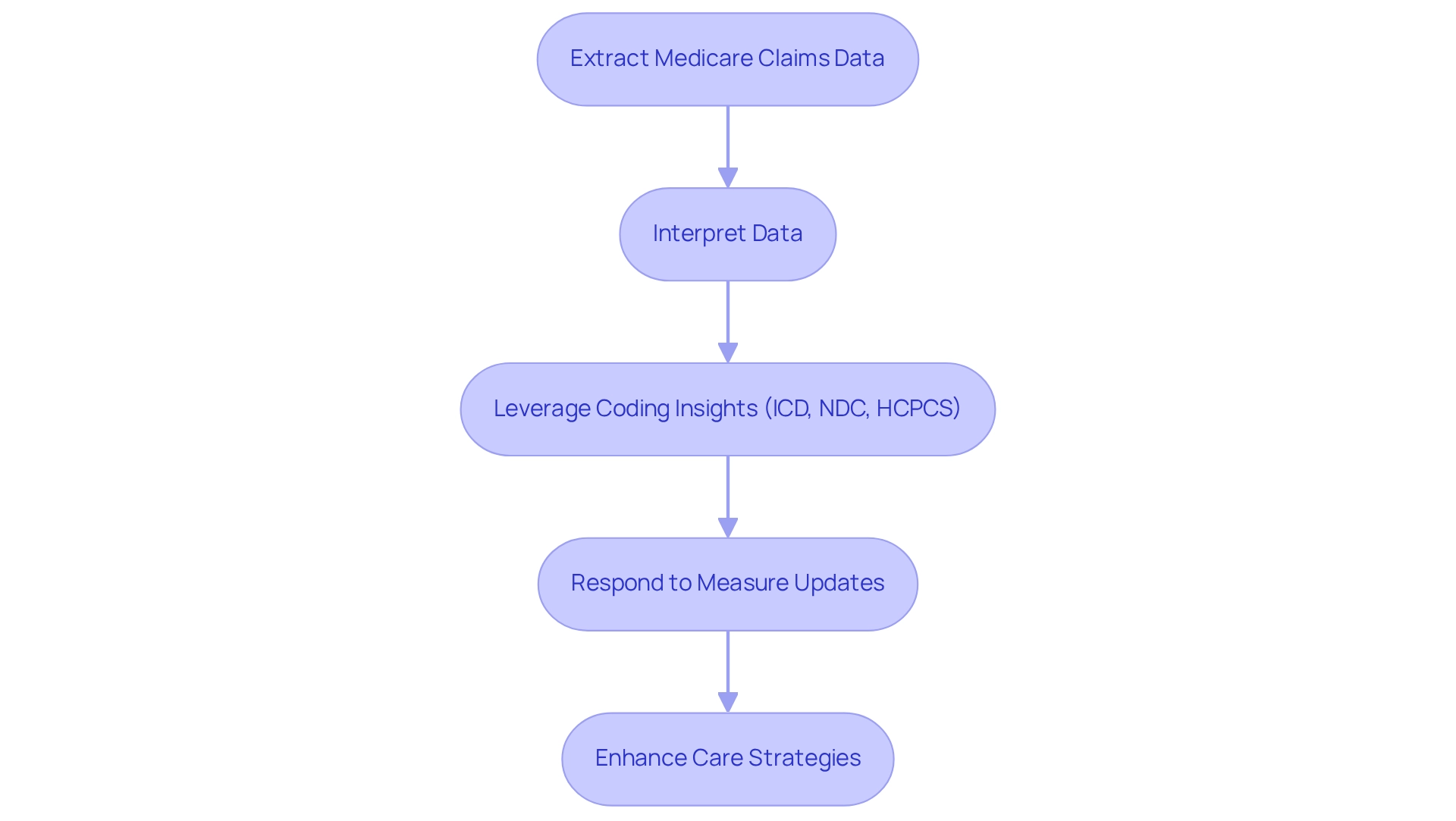
CareSet excels in extracting and interpreting complex Medicare claims information, offering stakeholders vital insights into treatment patterns and provider networks. By examining over $1.1 trillion in annual claims information and incorporating more than 100 external sources, CareSet equips healthcare organizations with the tools necessary to make informed decisions that significantly impact their 5 star rating cms. This data-driven approach not only uncovers gaps in care but also enhances experiences for individuals, both of which are crucial for achieving a 5 star rating cms.
As providers navigate the intricate pathways from diagnosis to treatment, leveraging insights from ICD, NDC, and HCPCS codes becomes increasingly critical. With the recent updates to measures for 2025, including the removal of the Medication Therapy Management measure and the introduction of new measures, the ability to leverage comprehensive Medicare information is essential for organizations aiming to enhance their performance and improve health outcomes. According to healthcare analysts, organizations that effectively utilize Medicare claims data can significantly enhance their care strategies and improve their chances of achieving a 5 star rating cms.
CMS Five-Star Quality Rating System: Importance and Impact on Healthcare Facilities
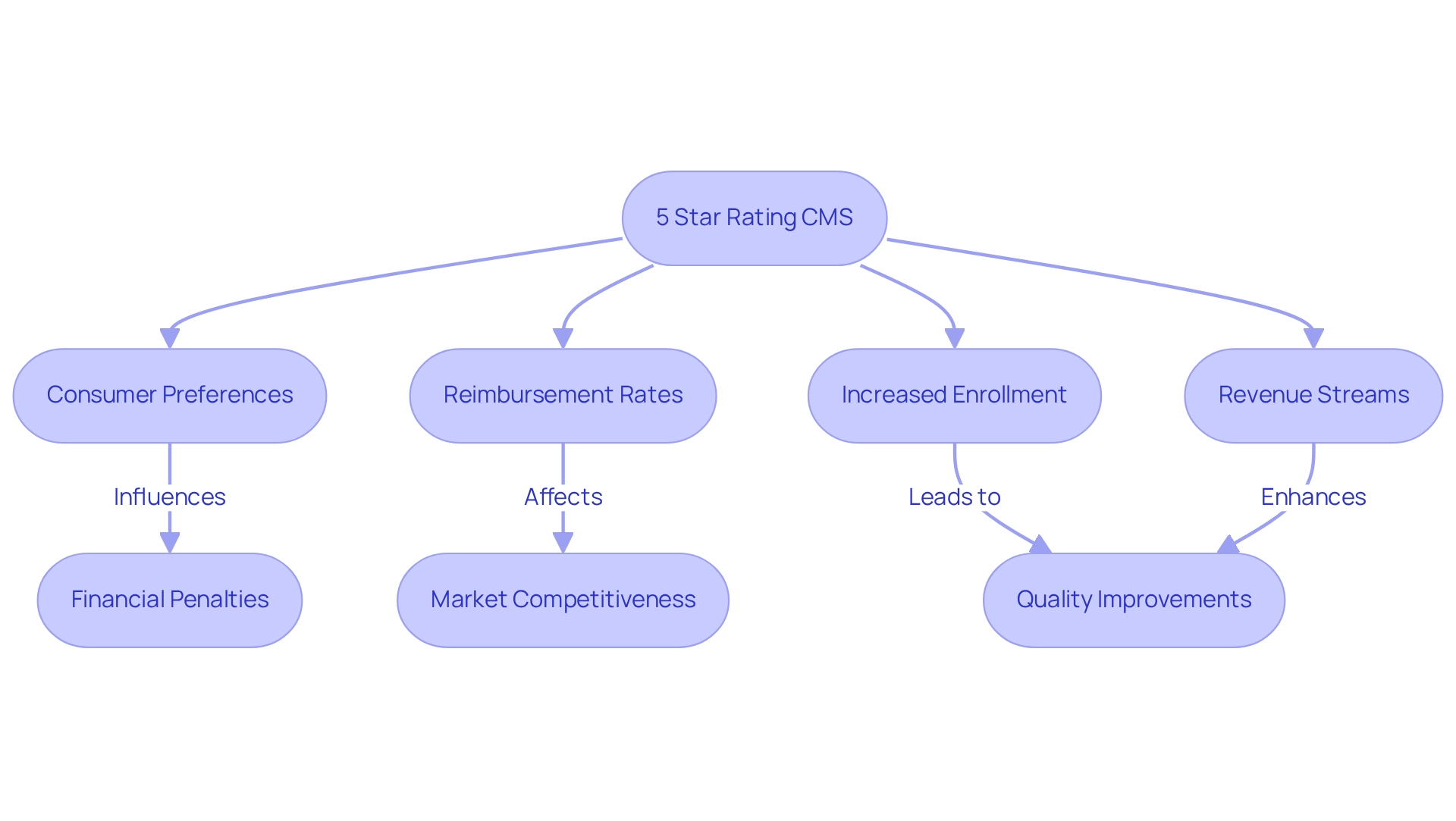
The 5 star rating cms serves as a vital resource for consumers evaluating the quality of Medicare health and drug plans. Its impact extends beyond individual choices, influencing healthcare facilities by shaping consumer preferences, reimbursement rates, and overall market competitiveness. Facilities that achieve a 5 star rating cms not only attract more individuals but also experience increased enrollment and revenue streams. For instance, organizations involved in the Medicare Shared Savings Program (MSSP) reported modest savings, with a notable $1.8 billion saved in 2022. This underscores the financial advantages of improved quality ratings that are directly associated with the 5 star rating cms.
Furthermore, the Centers for Medicare & Medicaid Services (CMS) has indicated financial penalties for hospitals failing to achieve at least 50% engagement in preoperative and postoperative evaluations. This highlights the significance of these ratings as a benchmark for accountability and performance. As the healthcare landscape continues to evolve, understanding and enhancing the 5 star rating cms is essential for providers aiming to elevate service quality and achieve operational success.
Notably, Jessica Walradt, Medical Director of Orthopedic Surgery at Northwestern Memorial Hospital, remarked, “The newly enacted Medicare Drug Price Negotiation Program is poised to lower prices of certain high-cost drugs covered under Medicare Part D beginning in 2026.” This statement reflects the shifting dynamics in Medicare that healthcare facilities must adeptly navigate. Moreover, CareSet’s comprehensive healthcare data insights, particularly from its case studies, empower healthcare stakeholders to make informed decisions that enhance care and drive business success. For example, a case study on an oncology treatment manufacturer emphasizes the critical need for timely engagement with physicians regarding treatment options like Qinlock for Gastrointestinal Stromal Tumor (GIST).
With CMS aiming for the entire Medicare program to transition to value-based payments by 2030, the urgency for healthcare organizations to prioritize their strategies regarding the 5 star rating cms will only intensify. It is imperative for them to align their market access strategies and engagement initiatives accordingly.
Calculation of CMS Star Ratings: Key Components and Methodology
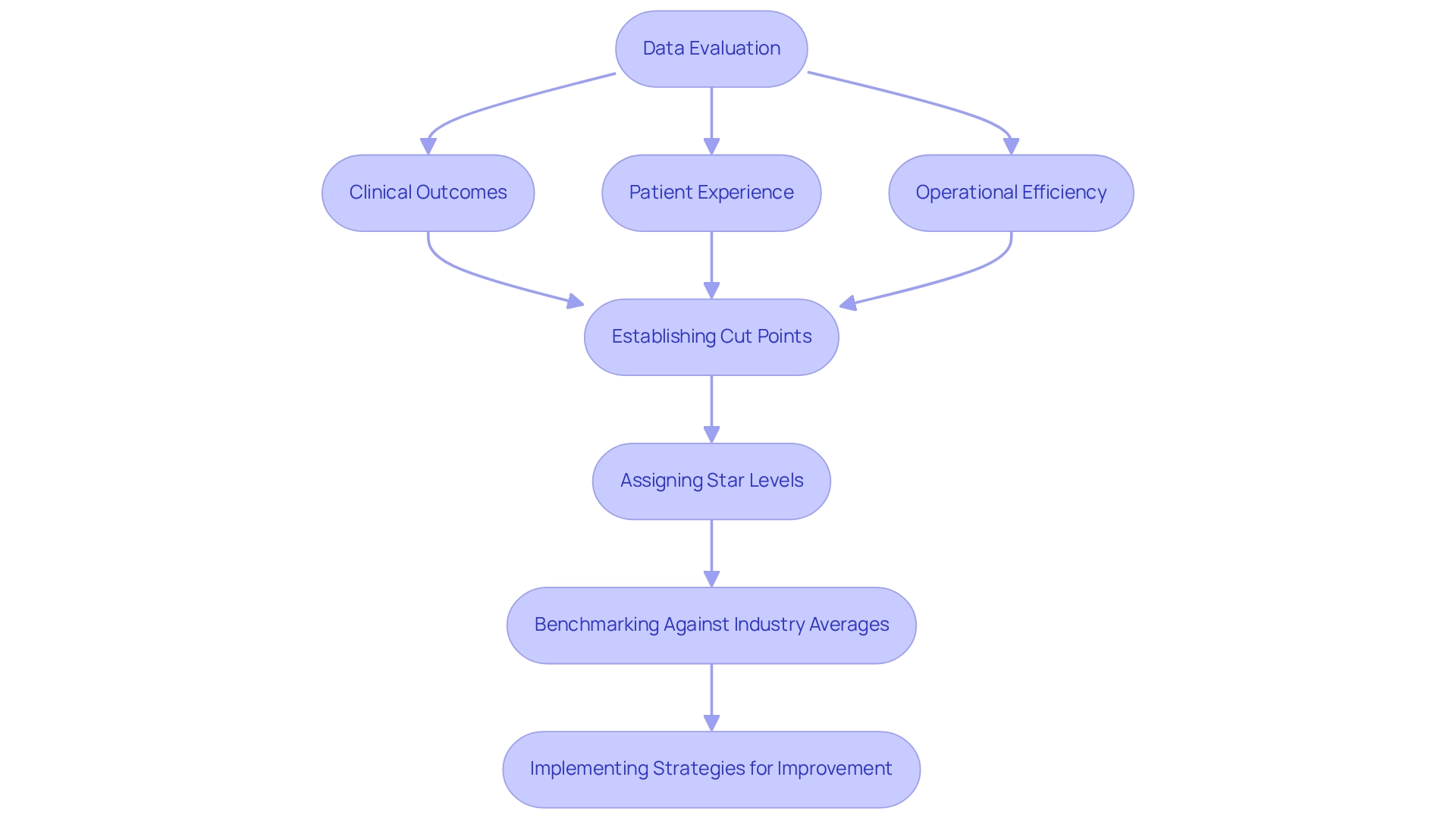
The determination of CMS ratings, such as the 5 star rating cms, is based on a comprehensive evaluation of various performance measures, including clinical outcomes, patient experience, and operational efficiency. The calculation methodology aggregates data from diverse sources and employs advanced statistical techniques to ensure precision. Establishing cut points is crucial, as these thresholds dictate the star levels assigned to healthcare facilities. While specific components such as health inspections and staffing levels are commonly discussed in the context of quality measures, focusing on the performance metrics that directly influence Ratings is essential.
For instance, a case study on colorectal cancer screening optimization revealed that health plans could significantly boost screening rates by implementing tailored communications and collaborating with providers. This approach led to a 4.3% higher rate of gap closure among members who received targeted outreach compared to those who were not engaged. Such examples underscore the importance of strategic initiatives in improving performance measures.
Moreover, consistently low performance can deter beneficiary enrollment and result in penalties from the Centers for Medicare & Medicaid Services (CMS). As CMS has pointed out, raising measure-level cut points complicates the ability of plans to attain a 5 star rating cms, making it essential for healthcare facilities to comprehend these challenges. Therefore, benchmarking performance against industry averages can provide insights into areas needing improvement, enabling healthcare facilities to refine their strategies effectively.
To enhance performance metrics, healthcare facilities should consider implementing targeted outreach programs, collaborating closely with providers, and continuously monitoring their performance against industry benchmarks. By leveraging CareSet’s comprehensive healthcare data insights, facilities can identify specific areas for improvement and develop tailored strategies that align with their goals. These practical approaches can assist facilities in managing the intricacies of the CMS evaluation system and enhance their overall scores.
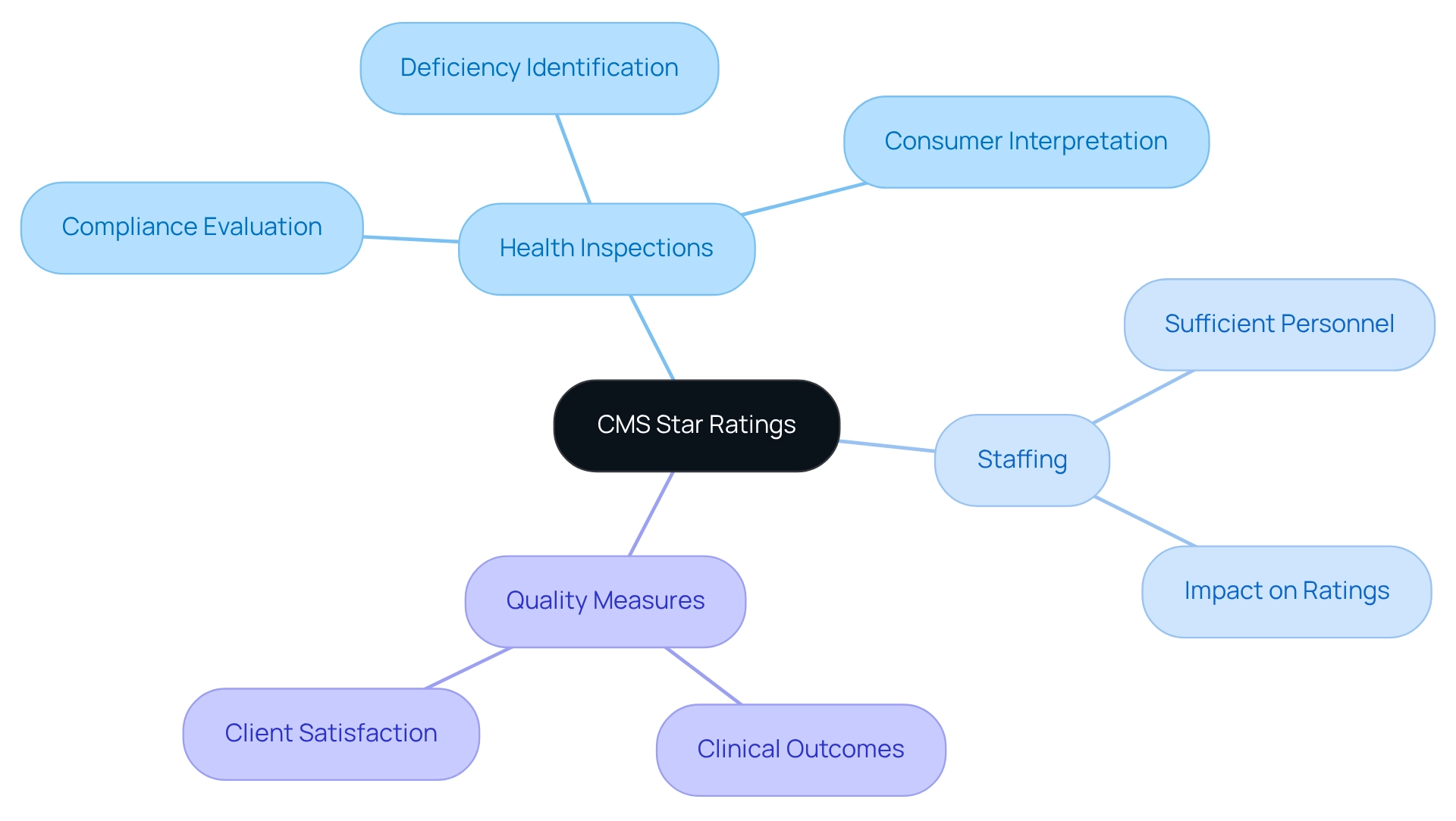
Key Metrics Influencing CMS Star Ratings: Health Inspections, Staffing, and Quality Measures
The key metrics influencing CMS Rating systems encompass health inspections, staffing levels, and various quality measures. Health inspections are critical as they evaluate compliance with federal regulations and the overall quality of care provided in facilities. These inspections not only identify deficiencies but also highlight areas for improvement, significantly affecting a facility’s rating. For instance, nursing homes that receive a 1-star rating are deemed to have quality levels much below average, underscoring the necessity of maintaining high standards. Compounding the challenge, consumers often struggle to interpret health inspection reports from Nursing Home Compare, emphasizing the need for clearer reporting.
Staffing metrics play a crucial role in evaluating whether facilities possess sufficient personnel to effectively meet the needs of those receiving care. Research indicates that improved staffing levels correlate with better outcomes for individuals and higher Star Ratings. For example, facilities that have increased their nursing staff have reported significant improvements in their ratings, demonstrating that adequate staffing is essential for delivering quality care.
Quality measures include clinical outcomes and client satisfaction, serving as indicators of a facility’s performance. Monitoring the use of antipsychotic medications among long-stay residents is particularly crucial due to the associated risks; facilities that manage these metrics effectively can enhance their ratings. As Francis Peabody aptly stated, “The secret of the care of the individual is in caring for the individual.” This encapsulates the essence of patient-centered care, integral to achieving high quality measures.
A case study on the Five-Star Nursing Home Quality Rating System illustrates that while these ratings are valuable tools for selecting a nursing home, they should not be the sole basis for decision-making. Personal assessments and site visits are essential to ensure that the chosen facility meets specific needs, particularly for specialized care such as dementia.
In summary, by concentrating on health inspections, staffing sufficiency, and quality measures, healthcare facilities can greatly enhance their performance and achieve a 5 star rating cms in their evaluations, ultimately leading to better care and outcomes for individuals.
Benefits of High CMS Star Ratings: Enhanced Patient Experience and Increased Revenue
Attaining a 5 star rating cms offers numerous benefits, particularly in enhancing experiences for individuals and driving revenue growth. Facilities that achieve a 5 star rating cms are often recognized as providers of exceptional quality care, leading to increased satisfaction and loyalty among individuals. This perspective is crucial, as content individuals are more likely to engage with healthcare services and recommend them to others. Moreover, achieving a 5 star rating cms in performance scores can lead to improved reimbursement rates and eligibility for quality bonus payments, significantly bolstering a facility’s financial stability. For instance, organizations that effectively streamline additional benefits and focus on essential medical services, as highlighted in the case study, have witnessed notable revenue growth, exemplifying the financial impact of prioritizing quality enhancements.
In 2025, the advantages of high CMS performance scores extend beyond financial metrics; they also enhance the overall experience for individuals. Facilities dedicated to delivering a unique omnichannel experience are better positioned for member retention and competitive differentiation. Insights from healthcare economists indicate that improved performance scores correlate with better financial outcomes, particularly as CareSet integrates over 100 external data sources to provide comprehensive insights into treatment patterns and demographics. To leverage these insights effectively, Pharmaceutical Market Access Managers can utilize CareSet’s data solutions to pinpoint key areas for improvement within their facilities. By focusing on data-driven strategies, they can elevate healthcare quality and drive business success.
Additionally, a significant development in March 2024 involved CMS reevaluating Elevance Health’s contract ratings, resulting in an additional $190 million bonus payout for the organization. This serves as a tangible illustration of the financial advantages associated with high CMS performance scores, underscoring the importance of quality care in achieving sustainable growth.
Case studies reveal that organizations with high performance scores not only improve client satisfaction but also reap substantial financial rewards. By investing in quality enhancements and leveraging CareSet’s extensive healthcare data insights, healthcare facilities can construct a compelling argument for prioritizing 5 star rating cms performance scores, which ultimately leads to improved outcomes for individuals and organizational success.
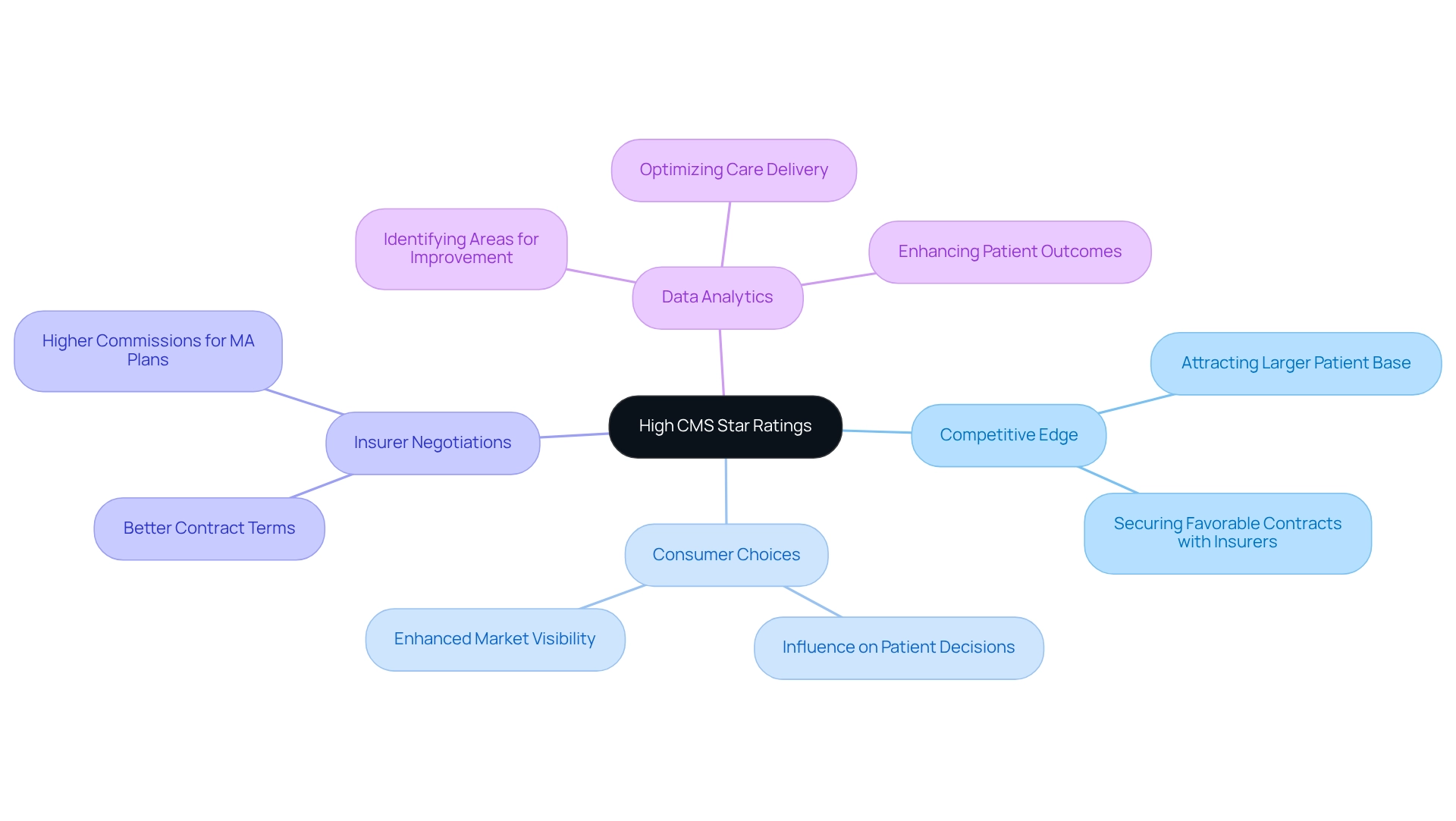
Strategic Advantages of High CMS Star Ratings: Competitive Edge in Healthcare Market
Achieving high scores in 5 star rating cms provides a significant competitive edge in the healthcare environment. Organizations that achieve a 5 star rating cms not only set themselves apart from their competitors but also attract a larger patient base and secure more favorable contracts with insurers. Hospitals must report at least three measures across different groups to meet the minimum thresholds for performance scores, ensuring that their evaluations reflect accurate assessments of care quality. This approach balances inclusivity with the necessity for reliable data, enhancing the credibility of the ratings.
In 2025, the impact of high Star Ratings is particularly pronounced, as they influence consumer choices and insurer negotiations. Facilities with high ratings, such as those with a 5 star rating cms, are often viewed as more reliable, as CMS star ratings indicate performance in clinical outcomes, experience of individuals, and efficiency of care delivery, fostering confidence and loyalty. Moreover, these ratings can significantly enhance an organization’s market visibility, leading to increased patient engagement and improved financial outcomes. Commissions for MA plans are presently greater than for stand-alone drug plans and Medigap, emphasizing the financial consequences of attaining high performance scores.
Healthcare organizations that focus on attaining a 5 star rating cms can utilize CareSet’s extensive Medicare insights to gain a competitive advantage. By utilizing data analytics, organizations can identify areas for improvement, optimize care delivery, and enhance outcomes for individuals, ultimately leading to better ratings. Those with strong ratings are better positioned to negotiate contracts with insurers, as these ratings serve as a testament to their quality of care. This dynamic not only benefits the organizations themselves but also contributes to improved patient outcomes across the board.
Expert opinions underscore the importance of Star Ratings in shaping strategic initiatives. As mentioned by industry leaders, “Our advanced tools and skilled team guarantee that health plans obtain the most precise and actionable insights,” highlighting the importance of reliable information in attaining high-quality care. By concentrating on improving their ratings with the assistance of CareSet’s insights, healthcare organizations can secure ongoing growth and achievement in a constantly changing environment.
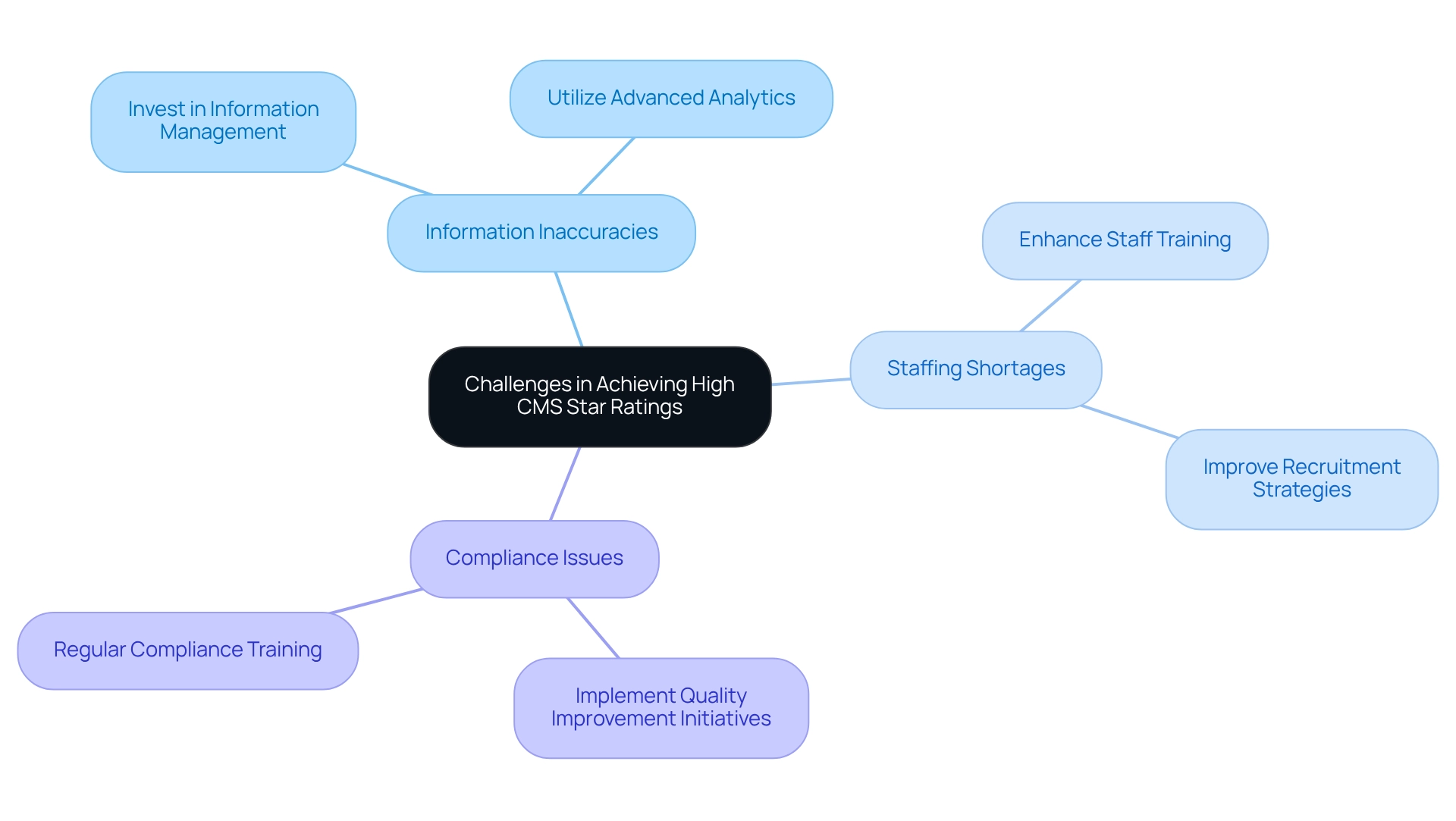
Challenges in Achieving High CMS Star Ratings: Common Obstacles and Solutions
Healthcare organizations encounter numerous challenges in attaining a 5 star rating cms, as information inaccuracies, staffing shortages, and compliance issues rank among the most significant obstacles. These factors can severely impede performance and negatively impact ratings. For instance, errors in information reporting may lead to misunderstandings of care quality, ultimately affecting outcomes and individual satisfaction. In 2025, a decline in the number of Medicare Advantage plans achieving 4+ star ratings is anticipated, potentially restricting bonus payments and funding for supplemental benefits, which complicates the landscape further. This trend heightens competition among Medicare Advantage plans, necessitating improved overall performance to retain members.
To effectively address these challenges, organizations should prioritize investments in robust information management systems that guarantee accuracy and reliability. CareSet’s advanced Medicare analytics solutions can substantially enhance provider targeting and insights regarding individuals, enabling organizations to identify key spending trends and resource needs. By analyzing over $1.1 trillion in annual claims and leveraging 14 years of continuously updated claims data, CareSet offers a comprehensive view of the healthcare market, which is vital for improving Star Ratings. Indeed, CareSet identified 15% additional targets, leading to a remarkable 250% increase in individuals recommended for treatment.
Moreover, enhancing staff training is essential, as well-trained personnel are better equipped to navigate compliance requirements and improve patient interactions. Implementing continuous quality improvement initiatives can foster a culture of excellence, empowering facilities to adapt to evolving standards and expectations. As Gabe Isaacson, an associate partner at McKinsey, observes, “These trends force a need for brokers to upgrade their capabilities, expand their best practices, and commit to higher standards to meet evolving demands and expectations.”
Real-world examples underscore the effectiveness of these strategies. Organizations that have adopted extensive data analytics tools, such as those offered by CareSet, have reported significant improvements in their performance scores, highlighting the importance of precise data in promoting quality care. By proactively addressing these issues, healthcare facilities can enhance their quality of care and achieve a 5 star rating cms, positioning themselves for success in an increasingly competitive environment. Furthermore, as payers face rising expenses in 2025, balancing clinical measures with member experience will be crucial for improving performance scores. To discover more doctors and accounts, consider leveraging CareSet’s analytics solutions.
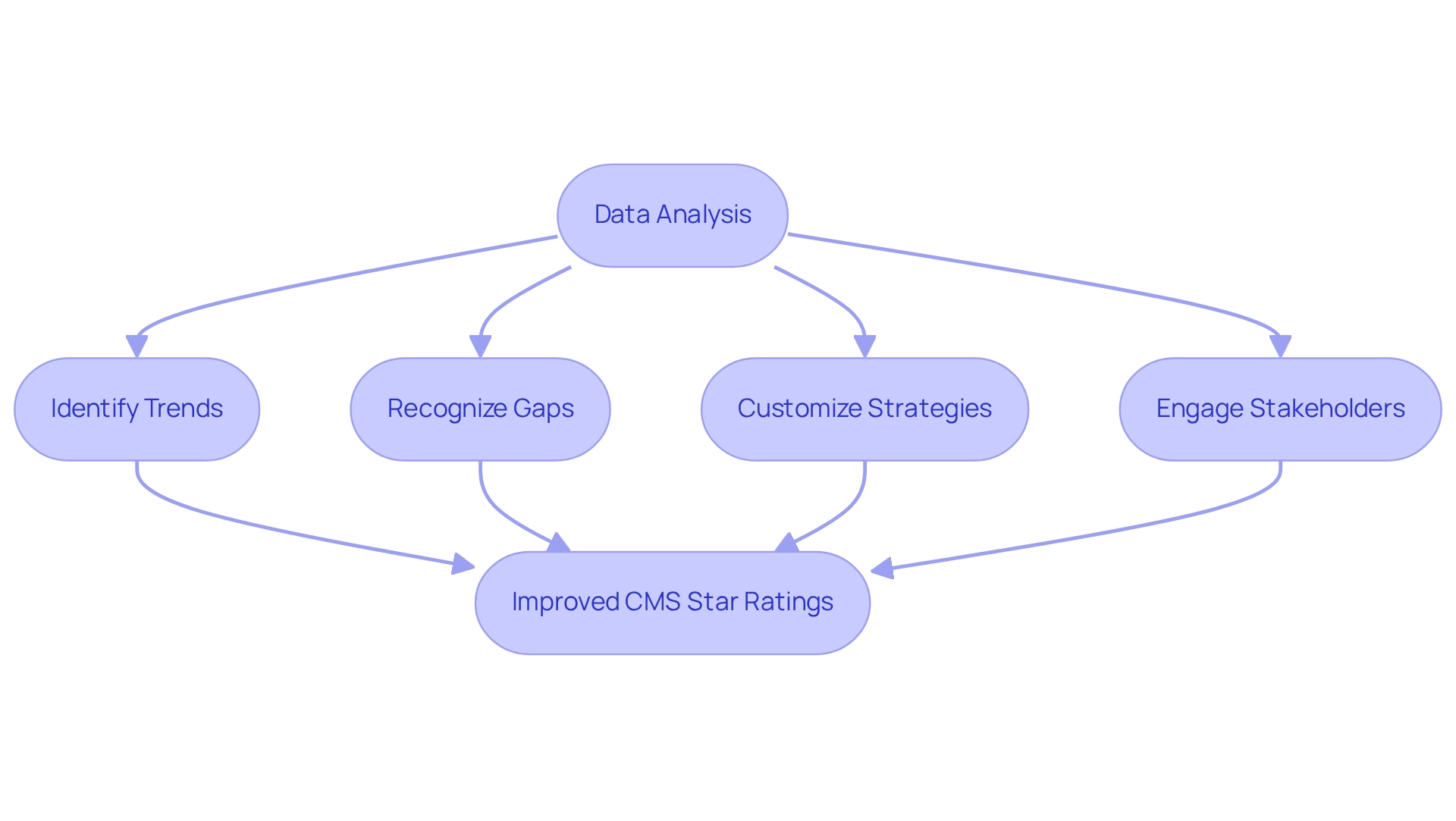
Role of Data Analysis in Enhancing CMS Star Ratings: Insights from CareSet
Data analysis is pivotal for enhancing CMS performance evaluations, yielding actionable insights into performance metrics and patient outcomes. CareSet’s expertise in Medicare information analysis enables healthcare organizations to identify trends, recognize gaps, and uncover avenues for improvement. By leveraging advanced analytics, these organizations can customize their strategies to tackle specific challenges, ultimately resulting in superior quality care and improved performance scores.
Recent case studies illustrate how health plans have adeptly navigated changes in performance evaluation methods by employing analytics to engage stakeholders and enhance outcomes. This proactive strategy has been instrumental in achieving elevated Star Ratings and delivering quality care.
As of 2025, organizations leveraging CareSet’s insights have reported notable improvements in their 5 star rating cms. With plans evaluated using a 5 star rating cms on a scale from one to five stars, the emphasis on data-driven strategies has become increasingly crucial. Significantly, Trella Health’s recent milestone of reaching 90% of all individuals in the U.S. aged 65 and older underscores the necessity of comprehensive information in this context, as it facilitates a clearer understanding of patient demographics and needs.
Moreover, insights from information analysts underscore the significance of actionable intelligence for healthcare performance. Carter Bakkum, a Senior Data Analyst in Healthcare Insights, noted, “Following the substantial shifts in the significance of analytics during the pandemic, it is essential to explore the figures further to reveal the narratives that influence our experience.” By pinpointing trends and gaps through meticulous Medicare data analysis, organizations can make informed decisions that lead to improved outcomes and optimized care delivery.
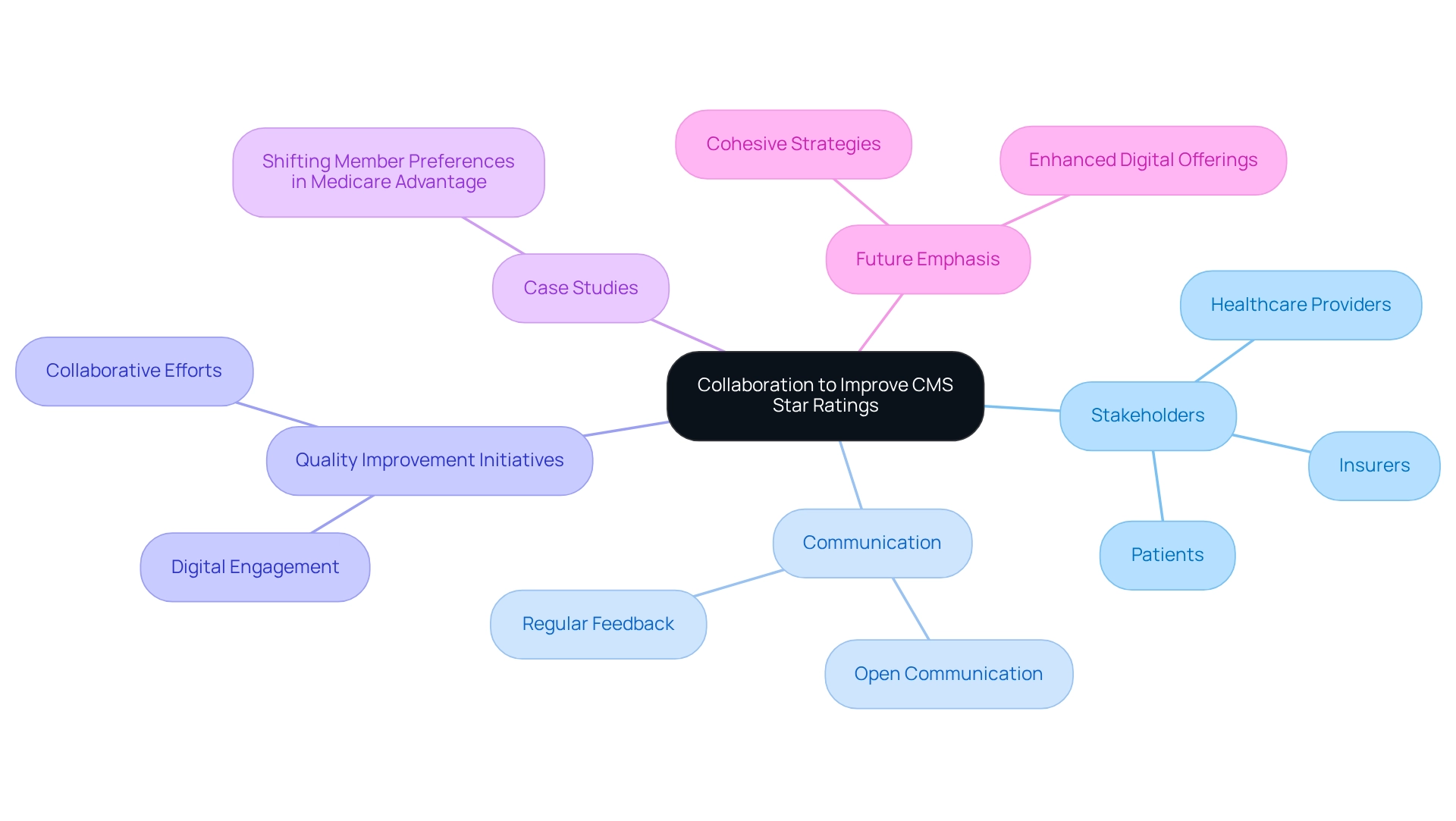
Collaboration Among Stakeholders: Key to Improving CMS Star Ratings
Cooperation among stakeholders—healthcare providers, insurers, and patients—is crucial for improving CMS performance scores. By fostering open communication and establishing shared objectives, organizations can implement effective quality improvement initiatives that cater to the diverse needs of all parties involved. Engaging stakeholders in the decision-making process not only aligns strategies with patient care goals but also drives better health outcomes and higher ratings.
Successful quality improvement initiatives often stem from collaborative efforts. The case study titled ‘Shifting Member Preferences in Medicare Advantage’ illustrates how stakeholders can significantly improve CMS performance scores by enhancing digital engagement and omnichannel experiences. In 2025, the emphasis on collaboration will be more pronounced, as organizations recognize that collective engagement leads to more effective solutions and improved member experiences.
Healthcare leaders emphasize the importance of stakeholder collaboration in achieving these goals. Insights from industry experts highlight that a unified approach can streamline processes and enhance the overall quality of care. Organizations utilizing CareSet’s comprehensive Medicare information insights can rationalize their supplemental benefit portfolios and reinvest in core medical benefits, which can lead to marked improvements in their 5 star rating cms. This reinforces the notion that teamwork is vital for success in the healthcare landscape.
As member preferences evolve, particularly towards digital engagement, the need for a cohesive strategy that incorporates stakeholder input becomes even more critical. Organizations should consider implementing frameworks that facilitate regular communication and feedback among stakeholders. By investing in collaborative strategies and utilizing CareSet’s data insights, organizations can not only enhance their performance scores but also cultivate long-term relationships that improve care and satisfaction. Gabe Isaacson notes that a fundamental query is whether new compensation caps will encourage payers to enhance their marketing and sales capabilities, further underscoring the importance of stakeholder engagement.
Future Trends in CMS Star Ratings: Innovations and Evolving Standards
The CMS Star Ratings system is undergoing a significant transformation, driven by innovations and evolving standards that will redefine healthcare quality assessment. A key trend is the increased emphasis on reported outcomes, which are becoming crucial for evaluating care quality from the individual’s perspective. Furthermore, the integration of social determinants of health is gaining traction, as these factors are increasingly recognized for their impact on health outcomes and overall patient experience.
Recent developments, such as Humana’s appeal of its star ratings results, underscore the real-world implications of these changes, with potential revenue threats looming for 2026. This situation highlights the urgency for healthcare organizations to adapt to the evolving environment of CMS performance evaluations.
Advancements in information analytics are also reshaping the landscape of CMS Star Ratings. By leveraging sophisticated analytical tools, healthcare organizations can gain deeper insights into treatment patterns and patient demographics, enabling them to tailor their services more effectively. CareSet’s pioneering role as the first Medicare data vendor, along with its integration of over 100 external data sources, exemplifies how data-driven solutions can enhance strategic initiatives for clients in the healthcare sector. This capability offers a more refined understanding of healthcare delivery that is essential for improving performance scores.
Expert forecasts indicate that the future of CMS quality evaluations will adopt a more comprehensive approach for assessing quality, integrating various metrics that reflect the complexities of care. As highlighted in recent case studies, such as the identification of consistently low-performing plans by the CMS, organizations must proactively address quality gaps to avoid increased scrutiny and potential corrective actions. The identification of low performers may lead to significant consequences, emphasizing the stakes involved in maintaining high-quality standards.
Moreover, the evolving landscape necessitates that healthcare organizations remain agile, adapting their strategies to align with the latest CMS expectations. Innovations in data analytics and quality assessment will not only enhance the 5 star rating cms but also contribute to better patient outcomes, ultimately driving success in the competitive healthcare market. As Emily Olsen noted, “CMS expands audits to crack down on Medicare Advantage overpayments,” highlighting the regulatory environment that organizations must navigate to ensure compliance and quality in their services.

Conclusion
Achieving high CMS Star Ratings is essential for healthcare organizations committed to enhancing patient care and ensuring financial sustainability. This article underscores the pivotal role of data analysis in navigating the intricacies of the CMS Five-Star Quality Rating System. By harnessing advanced analytics, organizations can pinpoint performance gaps and refine care delivery, which directly influences patient choice and reimbursement rates.
High Star Ratings confer numerous advantages, including improved patient experiences and increased revenue, thereby providing facilities with a competitive edge. Organizations that prioritize quality enhancements not only attract a higher volume of patients but also secure more favorable contracts with insurers. A comprehensive understanding of the rating system’s nuances is crucial for success in today’s competitive healthcare landscape.
Nevertheless, challenges such as data inaccuracies and staffing shortages can impede performance. Investing in robust data management systems and promoting stakeholder collaboration are vital strategies to surmount these hurdles. A cohesive approach to quality improvement initiatives is essential for driving superior health outcomes.
Looking ahead, the CMS Star Ratings system is set to evolve alongside advancements in data analytics and an increased focus on patient-reported outcomes and social determinants of health. By adopting a data-driven strategy and prioritizing quality improvements, healthcare organizations can enhance their Star Ratings, achieve better patient outcomes, and flourish in an increasingly competitive environment.


