Overview
The article titled “7 Insights on Fee for Service vs Value Based Care for Stakeholders” delves into the pivotal distinctions and ramifications of the transition from fee-for-service (FFS) to value-based care (VBC) models within the healthcare sector. This shift towards VBC underscores a profound emphasis on patient outcomes and the quality of care. It is propelled by comprehensive data analytics and active stakeholder engagement, ultimately culminating in enhanced healthcare delivery and optimized resource utilization.
Introduction
As the healthcare landscape undergoes a significant transformation, the shift from traditional fee-for-service (FFS) models to value-based care (VBC) is taking center stage. This evolution is not merely a change in payment structures; it represents a fundamental rethinking of how care is delivered and valued, placing a growing emphasis on patient outcomes and quality over quantity.
With the increasing adoption of innovative technologies and comprehensive data analytics, stakeholders are now better equipped to navigate these changes, unlocking insights that drive improved healthcare decisions.
As organizations strive to enhance patient satisfaction and optimize resource allocation, understanding the implications of this transition becomes crucial for achieving success in an ever-evolving industry.
CareSet: Comprehensive Medicare Data Insights for Fee for Service and Value Based Care
CareSet excels in extracting and interpreting complex Medicare claims data, providing stakeholders with comprehensive insights into the differences between fee for service vs value based care. By examining over $1.1 trillion in yearly claims data, CareSet enables clients to identify treatment patterns, provider networks, and demographics—elements crucial for informed decision-making in the rapidly evolving healthcare landscape. This data-driven approach not only highlights the implications of the fee for service vs value based care transition but also provides stakeholders with insights necessary to enhance individual well-being and optimize resource allocation.
The shift toward quality-focused treatment is underscored by recent trends emphasizing the growing importance of preventive services, chronic illness management, and coordinated support. For instance, the implementation of value-focused approaches in the Netherlands has yielded a 10% improvement in satisfaction ratings, showcasing the potential benefits of such models. Healthcare analysts, including Joshua Raskin, anticipate a significant transition in care delivery from insurers to providers, asserting that “the next era of healthcare will be defined by the trend of physician enablement.” In this context, the role of comprehensive Medicare data analysis becomes increasingly vital.
As we look ahead to 2025, the landscape of Medicare claims data analysis is expected to advance further, with stakeholders relying on precise data to navigate the complexities of market access and consumer engagement. CareSet’s commitment to delivering high-quality insights without flawed projections positions its clients to make strategic decisions that improve patient outcomes and optimize the lifecycle management of pharmaceutical products. The insights derived from Medicare claims data are not mere statistics; they reflect real-world implications on medical decisions, ultimately driving enhancements in treatment analytics and market reach.
Moreover, CareSet’s innovative data science offerings, which include features like predictive analytics and real-time reporting, aim to support drug launches and refine medical strategies, empowering stakeholders with actionable insights from over 62 million beneficiaries and 6 million providers. Case studies, such as those demonstrating the impact of CareSet’s data on oncology treatment options, further illustrate the effectiveness of these insights in practical applications.
Transitioning from Fee for Service to Value Based Care: Key Implications
Transitioning from fee for service vs value based care presents several pivotal implications for stakeholders. This shift underscores a movement from fee for service vs value based care, compelling healthcare providers to prioritize individual outcomes over the sheer number of services delivered. Such a transformation necessitates significant alterations in service delivery models, including enhanced coordination of services and improved patient involvement strategies. Furthermore, stakeholders must navigate new reimbursement structures that focus on the debate of fee for service vs value based care, incentivizing quality and efficiency rather than quantity.
Statistics reveal that 63% of studies indicate mixed motivations behind the adoption of value-based care models, highlighting the complexity of this transition. Case studies, such as “PUTTING PATIENTS FIRST: Unlocking Medicare Data to Empower HCP” involving oncology treatment options like Qinlock for Gastrointestinal Stromal Tumor (GIST), illustrate how leveraging comprehensive Medicare data can enhance engagement with healthcare providers. CareSet’s data-driven solutions empower stakeholders by offering insights from more than 62 million beneficiaries and 6 million providers, facilitating informed decision-making that aligns with individual needs and pharmaceutical utilization.
Specialist viewpoints underscore the significance of this shift; for instance, Dr. Brady Steineck emphasizes how collaborations in quality-driven healthcare can revive a commitment to high-standard service for individuals. He notes that working with entities like agilon has rekindled his enthusiasm for delivering the assistance elderly individuals merit. As medical leaders advocate for these changes, it becomes increasingly clear that aligning strategies with the evolving medical landscape is crucial for achieving better patient outcomes and ensuring sustainable growth in the industry.
Understanding the Core Differences Between Fee for Service and Value Based Care
The essential distinctions between fee for service vs value based care are rooted in their philosophies and payment frameworks. The discussion of fee for service vs value based care highlights how fee-for-service models reward providers based on the volume of services delivered, potentially leading to unnecessary procedures and inflated medical expenses. In contrast, outcome-focused models emphasize patient results and the quality of services provided, rewarding providers for achieving specific health goals and enhancing patient satisfaction. This transition fosters a more comprehensive approach to medical care, emphasizing preventive measures and effective chronic disease management. Consequently, outcome-focused treatment not only enhances health results but also contributes to cost savings throughout the medical system. CareSet’s extensive Medicare data solutions, incorporating insights from over 62 million beneficiaries and 6 million providers, empower medical stakeholders to navigate this transition effectively. With over $900 billion in claims processed annually, these insights enable organizations to gain a deeper understanding of individual needs, provider networks, and pharmaceutical utilization, ultimately guiding strategic medical decision-making.
For instance, a recent collaboration between Aetna and Landmark Health exemplifies this shift. Launched in March 2024, their partnership focuses on delivering home-based medical assistance to individuals with chronic illnesses participating in outcome-oriented health programs. This collaboration strengthens reimbursement practices centered on quality across the medical sector by demonstrating how customized support can yield better outcomes and satisfaction for individuals, thereby underscoring the practical application of data insights in real-world contexts.
Statistics from 2023 reveal that strategic acquisitions by health insurers and medical providers constituted 55% of total investment activity in the quality-focused sector, underscoring the growing commitment to this model. These acquisitions reflect a broader trend among stakeholders to transition from a focus on fee for service vs value based care to outcome-oriented approaches, as they seek to align incentives with patient health results. Moreover, addressing social determinants of health could potentially reduce U.S. medical expenses by 11%, highlighting the financial benefits of a value-oriented approach and the importance of considering factors beyond clinical services. Experts assert that the transition from fee for service vs value based care models represents not just a trend, but a crucial evolution in medical delivery. This shift is essential for enhancing service quality and ensuring the sustainability of medical systems in the long run. To effectively navigate this transition, stakeholders, particularly pharmaceutical market access managers, should prioritize developing strategies that emphasize health outcomes and invest in data analytics—like those offered by CareSet—to evaluate the impact of their initiatives.
Pros and Cons of Fee for Service vs Value Based Care: A Comparative Analysis
When comparing fee-for-service (FFS) and value-based care (VBC), distinct advantages and disadvantages emerge, significantly shaping the landscape of healthcare delivery.
Pros of Fee-for-Service:
- Immediate Revenue: Providers benefit from a steady cash flow, receiving payment for each service rendered, thus enhancing financial stability.
- Flexibility: Clinicians enjoy the freedom to offer a diverse array of services without restrictions, allowing for tailored patient care.
Cons of Fee-for-Service:
- The debate between fee for service vs value based care highlights how this model often incentivizes unnecessary procedures, resulting in inflated costs without corresponding improvements in patient outcomes.
- Fragmented Care: The lack of coordination among providers can lead to disjointed patient experiences and suboptimal health results.
Pros of Value-Based Care:
- Focus on Outcomes: Providers are incentivized to enhance patient health, fostering a commitment to high-quality care and improved health outcomes. For instance, a case study involving an oncology treatment producer illustrated how utilizing Medicare data through CareSet’s data leadership can facilitate prompt interaction with medical providers regarding treatment options such as Qinlock for Gastrointestinal Stromal Tumor (GIST), ultimately enhancing outcomes for individuals. This engagement resulted in a measurable increase in treatment adherence and patient satisfaction.
- Cost Efficiency: By prioritizing preventive care, VBC can significantly lower overall healthcare expenditures, benefiting both patients and providers.
Cons of Value-Based Care:
- The complex implementation of fee for service vs value based care necessitates substantial changes in practice management and care delivery, which can be challenging for many providers.
- Financial Risk: Providers might face financial penalties if they do not meet established quality metrics, creating a degree of uncertainty in their revenue streams.
A case study from the Netherlands demonstrates the effectiveness of VBC, where hospitals reported a 10% enhancement in satisfaction scores post-implementation of quality-driven approaches. This shift not only improved client experiences but also optimized resource utilization, showcasing the potential benefits of VBC in real-world settings. As healthcare professionals increasingly recognize the significance of social determinants of health, they understand that a quality-focused approach is a proactive strategy that can assist at-risk populations by decreasing illness, enhancing wellness, and reducing expenses. This proactive nature of VBC emerges as a promising strategy to address the needs of vulnerable populations, ultimately reducing illness and promoting wellness.
Impact of Fee for Service and Value Based Care on Patient Outcomes
The impact of fee for service vs value based care on individual outcomes is profound. In the discussion of fee for service vs value based care, individuals frequently encounter fragmented assistance, leading to inconsistent treatment and suboptimal health outcomes. Conversely, outcome-focused treatment promotes a coordinated, patient-centered approach that prioritizes health results, highlighting the differences between fee for service vs value based care. Recent studies indicate that individuals engaged in outcome-focused arrangements report significantly higher satisfaction levels and enjoy improved health outcomes, including a marked reduction in hospital readmissions and enhanced management of chronic conditions.
For instance, the emergence of the Home Health Value-Driven Purchasing Model in 2022 established a benchmark for quality-focused medical services, reinforcing the commitment to value-oriented reimbursement practices across the industry. This transition towards value-driven services is essential for elevating the overall quality of medical delivery, as evidenced by the 2.3 million additional individuals benefiting from such arrangements over the past decade. CareSet’s comprehensive Medicare data insights are pivotal in this evolution, equipping stakeholders with the knowledge necessary to make informed decisions that enhance patient support and drive business success.
Notably, case studies from oncology treatment providers illustrate how CareSet’s data-driven methodologies have improved interactions with medical providers regarding late-stage treatment options. However, it is important to note that fewer than half of primary healthcare providers in the United States have reported receiving payments through outcome-oriented reimbursement models, highlighting ongoing challenges in the adoption of these strategies. Furthermore, the share of private capital investment in outcome-focused asset classes within the medical sector has surged from 6% in hospitals to nearly 30% in just two years, reflecting a growing interest and financial backing for outcome-oriented approaches.
As the healthcare landscape evolves, the emphasis on quality-driven services will continue to play a crucial role in enhancing patient experiences and outcomes, particularly in the context of pharmaceutical market access strategies. Additionally, CareSet’s latest data science offerings are designed to facilitate drug introductions, providing insights that can further augment the effectiveness of initiative-based healthcare efforts.
Financial Incentives in Fee for Service vs Value Based Care: What You Need to Know
Financial incentives play a pivotal role in shaping the dynamics of treatment models, particularly in the context of fee for service vs value based care. In the fee-for-service model, providers are incentivized to increase the volume of services rendered, as their revenue directly correlates with the quantity of assistance provided. This framework often results in overutilization, escalating medical costs without necessarily improving patient outcomes.
Conversely, quality-oriented models prioritize excellence and patient results, rewarding providers for achieving specific performance metrics. Notably, in 2023, strategic investments by health insurers and healthcare providers accounted for 55% of total activity in the performance-oriented healthcare sector, signaling a significant shift in treatment provision and compensation.
Furthermore, the integration of personalized medicine into value-oriented health systems has the potential to reduce adverse drug events by up to 30%, as highlighted by specialist Samruddhi Yardi. Understanding these financial dynamics is crucial for stakeholders aiming to formulate effective reimbursement strategies that align with both organizational objectives and individual welfare goals.
CareSet’s comprehensive Medicare data insights, derived from over 62 million beneficiaries and 6 million providers, empower stakeholders to adeptly navigate these changes by providing vital information on individual needs, provider networks, and pharmaceutical utilization.
Real-world examples, such as the implementation of quality-focused treatment in nephrology, demonstrate its effectiveness in reducing hospital admissions and complications, thereby improving health outcomes while controlling costs. Significantly, a 5% reduction in hospital admissions for chronic obstructive pulmonary disease (COPD) patients in the Netherlands further underscores the benefits of patient-centered approaches.
As the healthcare landscape evolves, the transition from fee for service vs value based care continues to reshape reimbursement strategies, emphasizing the urgent need for stakeholders to adapt and innovate their methodologies.
Leveraging Technology for the Transition to Value Based Care
The successful transition from fee for service vs value based care depends on the effective use of technology. As David B. Snow, Jr. stated, ‘Ultimately, the discussion of fee for service vs value based care reveals a broken system, and those who align business toward value and prevention will succeed because it’s the right thing to do.’ Advanced data analytics, electronic health records (EHRs), and telehealth solutions play crucial roles in improving coordination of services and engagement of individuals.
Key insights include:
- Data Analytics: CareSet’s innovative data science products empower providers to identify at-risk patients and implement preventive measures, significantly improving patient outcomes. CareSet’s monthly Medicare updates provide critical insights into drug utilization and treatment pathways, answering essential business questions that enhance provider engagement.
- EHRs: These systems enable smooth information exchange among treatment teams, ensuring that all parties have access to crucial individual data, which is vital for informed decision-making in a quality-focused service model.
- Telehealth: This approach has proven crucial in broadening access to services, especially for individuals in distant regions, with its usage surging by 154% in 2020.
- Financial Benefits: Physicians can earn as much as 241% more than Medicare’s rates under the fee for service vs value based care model, emphasizing the financial incentives for providers to adopt it.
- Ethical AI Use: It is essential to guarantee responsible and ethical utilization of AI tools to safeguard individuals and improve service delivery.
By adopting these technologies, healthcare organizations can optimize operations, improve patient experiences, and ultimately promote better health results in a framework focused on value. Significantly, models centered on outcomes have been associated with a 4.6% decrease in 30-day hospital readmission rates, highlighting the effectiveness of these strategies in managing chronic conditions.
Engaging Stakeholders in the Shift to Value Based Care
Involving stakeholders in the transition to quality-focused services is essential for fostering teamwork and ensuring effective execution. Key stakeholders—including healthcare providers, payers, and patients—must be actively engaged in both the planning and implementation of initiatives centered on quality. Effective communication and transparency are crucial for building trust and aligning objectives. Engagement approaches can include:
- Frequent meetings
- Feedback sessions
- Joint decision-making processes
All of which have been shown to enhance stakeholder involvement, particularly in the debate of fee for service vs value based care. As we look ahead to 2025, with value-driven practices continuing to gain traction, it is imperative to embrace innovative collaboration strategies. For instance, leveraging CareSet’s extensive Medicare data insights can significantly improve the collection and sharing of individual information, thereby enhancing service coordination. CareSet’s analytics solutions evaluate over $1.1 trillion in annual claims and integrate data from more than 100 external sources, empowering medical stakeholders with actionable insights that can lead to improved care outcomes.
A notable case study illustrates how the integration of electronic health records and data analytics has resulted in better-informed decision-making, ultimately enhancing care outcomes by enabling stakeholders to access real-time data and insights. According to Samruddhi Yardi, over 36% of medical payments in the U.S. are now linked to alternative payment models, highlighting the ongoing shift from fee for service vs value based care and underscoring a steady rise in the adoption of quality-oriented payment methods. This shift highlights the critical importance of stakeholder involvement, as it directly correlates with improved outcomes for those receiving care. Furthermore, patient-centered approaches have led to a 9% decrease in emergency visits and a 7% reduction in healthcare inequalities, showcasing the success of collaborative efforts in achieving these results.
To ensure successful stakeholder involvement, healthcare organizations must prioritize effective communication strategies. This includes:
- Establishing clear goals
- Utilizing technology for seamless information exchange
- Fostering an inclusive environment for feedback
By cultivating a shared vision for quality-driven healthcare that enhances patient outcomes and promotes organizational success, entities can actively engage stakeholders in the process. As a call to action, stakeholders are encouraged to implement these strategies within their organizations to facilitate the transition to patient-centered approaches.
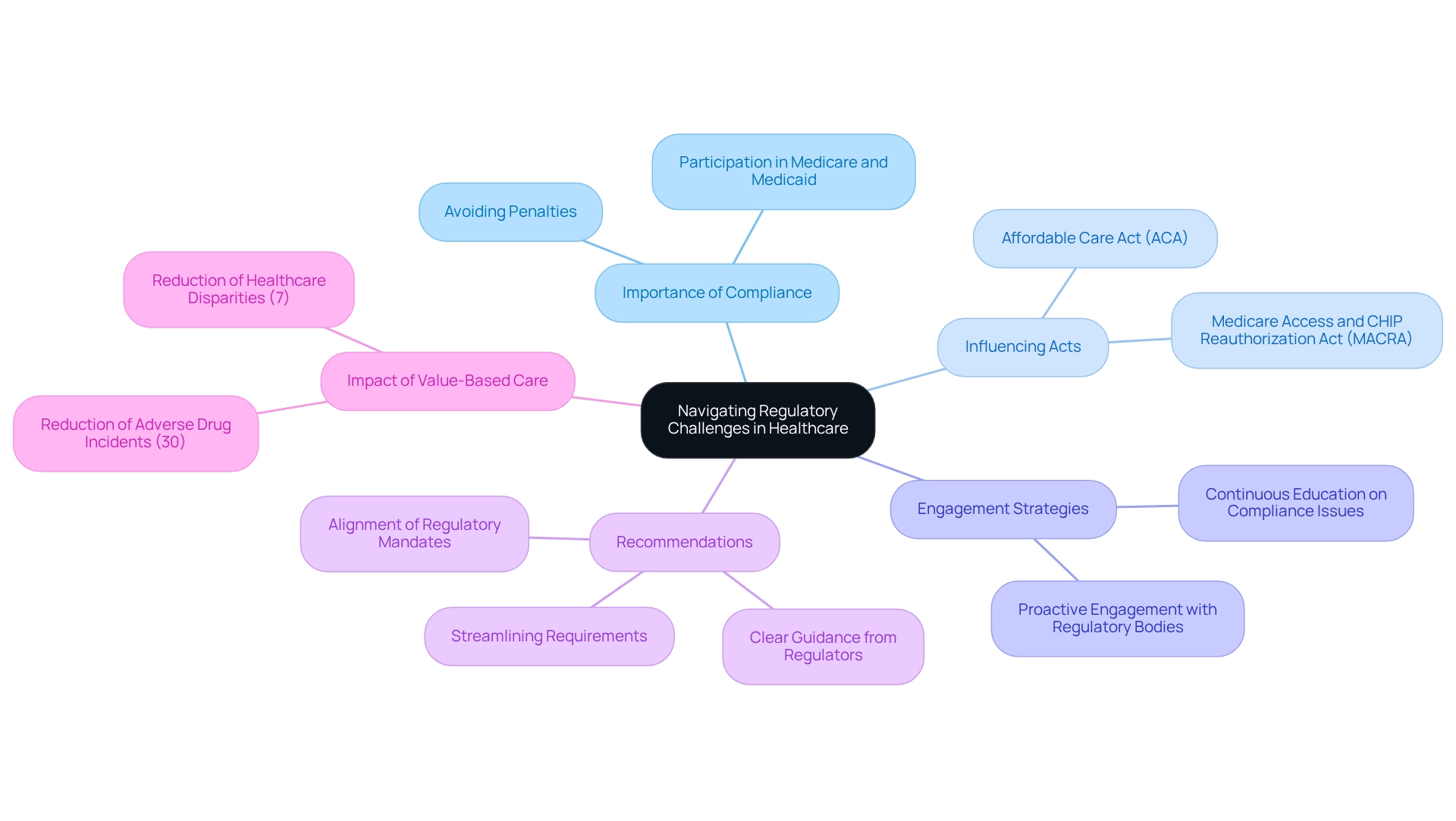
Navigating Regulatory Challenges in Fee for Service and Value Based Care
Navigating regulatory challenges is essential for stakeholders engaged in the discussion of fee for service vs value based care models. As regulations governing reimbursement, quality metrics, and individual privacy continue to evolve, staying informed is imperative. Compliance with these regulations not only helps avoid penalties but also ensures ongoing participation in Medicare and Medicaid programs. The Affordable Care Act (ACA) has significantly influenced medical reimbursement, advocating for a transition from fee for service vs value based care, while the Medicare Access and CHIP Reauthorization Act (MACRA) further underscores the necessity for alignment with federal requirements.
Proactive engagement with regulatory bodies and continuous education on compliance issues are vital strategies for organizations aiming to effectively navigate these complexities. As compliance specialists indicate, “Staying ahead of regulatory changes is not merely about compliance; it’s about utilizing those changes to enhance health outcomes and operational efficiency.” Value-focused initiatives have demonstrated a 7% decrease in disparities in medical services, showcasing their potential to enhance equity in access and results. Furthermore, the integration of personalized medicine into quality-focused health systems has shown the ability to reduce adverse drug incidents by up to 30%, emphasizing the importance of regulatory adherence in improving safety for individuals.
Real-world examples of compliance strategies in Medicare and Medicaid illustrate how organizations can successfully adapt to regulatory challenges. By leveraging comprehensive insights from CareSet’s extensive Medicare data analytics, which encompass over 62 million beneficiaries and 6 million providers, stakeholders can better understand the implications of current regulations and develop informed strategies to align with them. CareSet addresses critical questions such as “Who drives adherence?” and “What is the diagnosis to treatment path?” to provide actionable insights. Additionally, recommendations to reduce administrative requirements include:
- Better alignment of regulatory mandates
- Clear guidance from regulators
- Streamlining meaningful use requirements
This approach not only mitigates risks but also fosters long-term growth and improved patient outcomes in the evolving medical landscape, all while upholding CareSet’s unwavering commitment to quality and patient privacy.
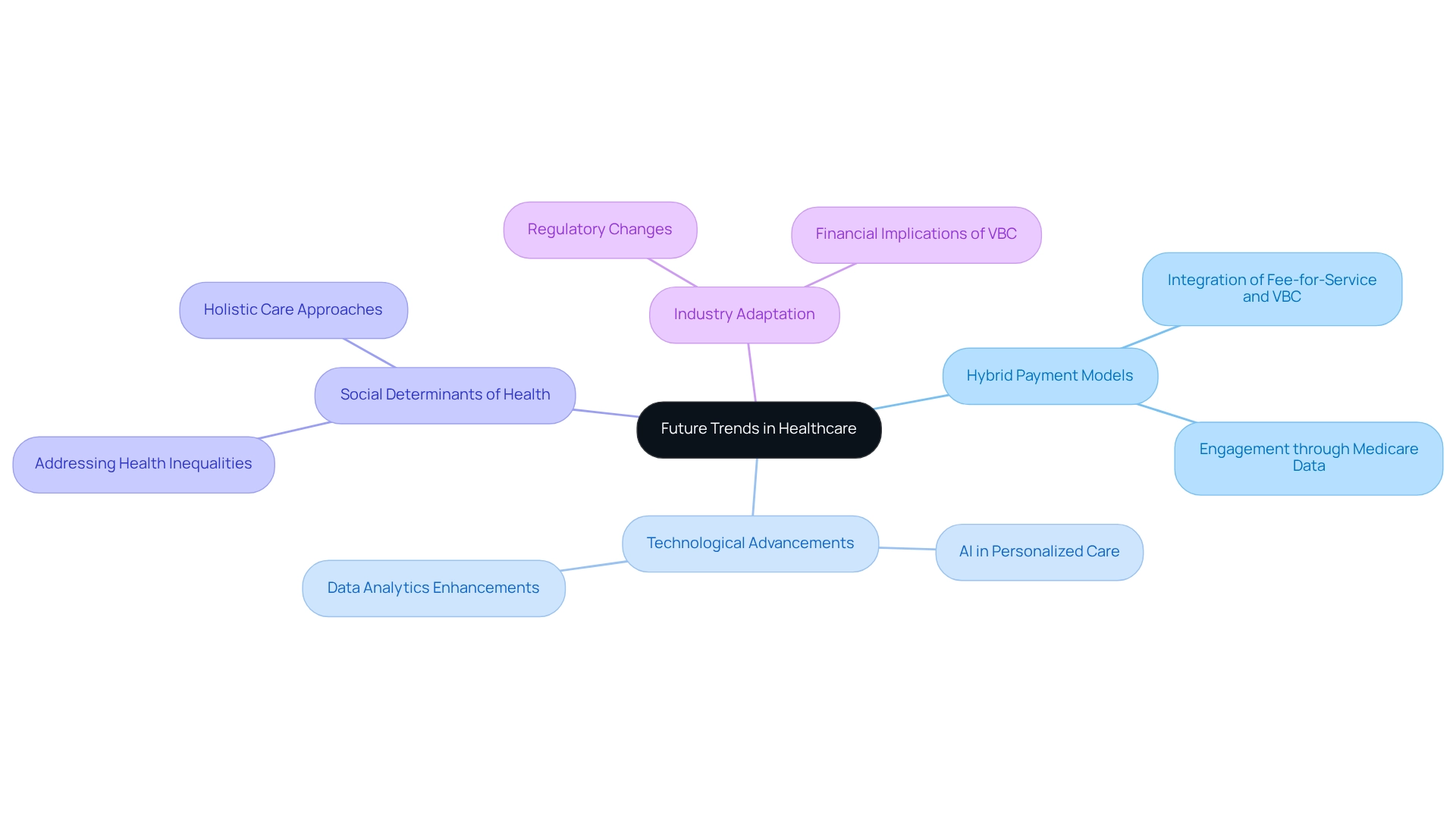
Future Trends in Healthcare: The Evolution of Fee for Service and Value Based Care
The medical landscape is on the brink of a significant transformation as it shifts from conventional fee for service vs value based care models to value-based care solutions. A notable trend is the increasing adoption of hybrid payment models that integrate elements of both fee for service vs value based care, which provides providers with enhanced flexibility in their reimbursement structures. This evolution represents not merely a change in payment but a fundamental rethinking of how assistance is delivered and valued.
Technological advancements, particularly in artificial intelligence (AI) and machine learning, are poised to revolutionize data analytics capabilities. These technologies empower medical providers to offer more individualized care by analyzing extensive volumes of individual data, including insights derived from CareSet’s comprehensive Medicare data solutions, to tailor treatment plans effectively. As AI continues to evolve, its integration into medical processes is expected to enhance personalization and efficiency, ultimately leading to improved outcomes for individuals. For instance, the case study titled “Putting Patients First: Unlocking Medicare Data to Empower HCP” illustrates how leveraging Medicare data can enhance engagement with medical providers regarding treatment options, highlighting the potential benefits of VBC.
Moreover, the growing emphasis on social determinants of health is fostering a more holistic approach to individual care. By addressing the root causes of health inequalities, stakeholders can contribute to a more equitable medical system. This comprehensive perspective is crucial for developing effective strategies that not only enhance individual patient outcomes but also improve overall community health.
As the industry evolves, stakeholders must remain agile and responsive to these emerging trends. The transition to fee for service vs value based care is not solely about modifying payment structures; it represents a broader commitment to enhancing the quality and accessibility of medical services. Notably, the Act aims to sustain the 2024 qualifying APM participant eligibility threshold levels through 2025, reflecting ongoing regulatory changes in payment models. Additionally, recent data reveals that year-over-year growth in inpatient revenue has outpaced outpatient revenue in March for the first time in over two years, underscoring the financial ramifications of the shift toward VBC. By embracing these changes and leveraging innovative data science products from CareSet, healthcare organizations can position themselves for success in an increasingly complex environment.
Conclusion
The transition from fee-for-service to value-based care represents a critical turning point in the healthcare landscape, placing significant emphasis on patient outcomes rather than the volume of services rendered. Key insights indicate that organizations utilizing comprehensive Medicare data, such as those provided by CareSet, are better positioned to navigate this paradigm shift. By delving into extensive datasets, stakeholders can identify treatment patterns, optimize resource allocation, and craft strategies that enhance patient satisfaction and overall care quality.
As the industry progresses, the commitment to value-based care is reinforced by compelling case studies and statistics that showcase improved patient outcomes, including decreased hospital readmissions and enhanced chronic disease management. This evidence substantiates the idea that value-based models not only yield better health results but also promote financial sustainability within healthcare systems. Furthermore, the integration of technology—particularly advanced data analytics and EHR systems—plays a crucial role in facilitating this transition, empowering healthcare providers to make informed decisions that prioritize patient needs.
In conclusion, the evolution towards value-based care is not merely a trend; it is a necessary paradigm shift that promises to elevate the quality of healthcare delivery. Stakeholders must remain engaged and proactive in adapting to these changes, leveraging data-driven insights and innovative technologies to ensure that patient care remains at the forefront of their strategic initiatives. By embracing this model, the healthcare industry can strive towards a future that prioritizes quality, efficiency, and ultimately, improved patient outcomes.


