Overview
Clinically integrated networks present significant advantages for healthcare providers, including:
- Enhanced collaboration
- Improved patient engagement
- Superior health outcomes achieved through data integration and resource sharing
These networks facilitate vital communication among providers, optimizing treatment pathways with comprehensive data insights. As a result, they lead to more effective patient care and operational efficiencies. Engaging with CareSet’s insights can further illuminate the transformative potential of these networks in healthcare.
Introduction
In the evolving landscape of healthcare, the integration of data and collaboration among providers is fundamentally transforming patient care. Clinically Integrated Networks (CINs) stand at the forefront of this revolution, harnessing comprehensive Medicare data to enhance treatment pathways, improve care coordination, and ultimately drive better health outcomes.
By leveraging insights from over $1.1 trillion in annual Medicare claims, organizations like CareSet empower healthcare providers to make informed decisions that bridge gaps in care and optimize patient engagement.
As the industry shifts towards value-based care, the significance of these networks in fostering collaboration and innovation becomes increasingly evident, promising a future where quality care is not merely an aspiration but a standard.
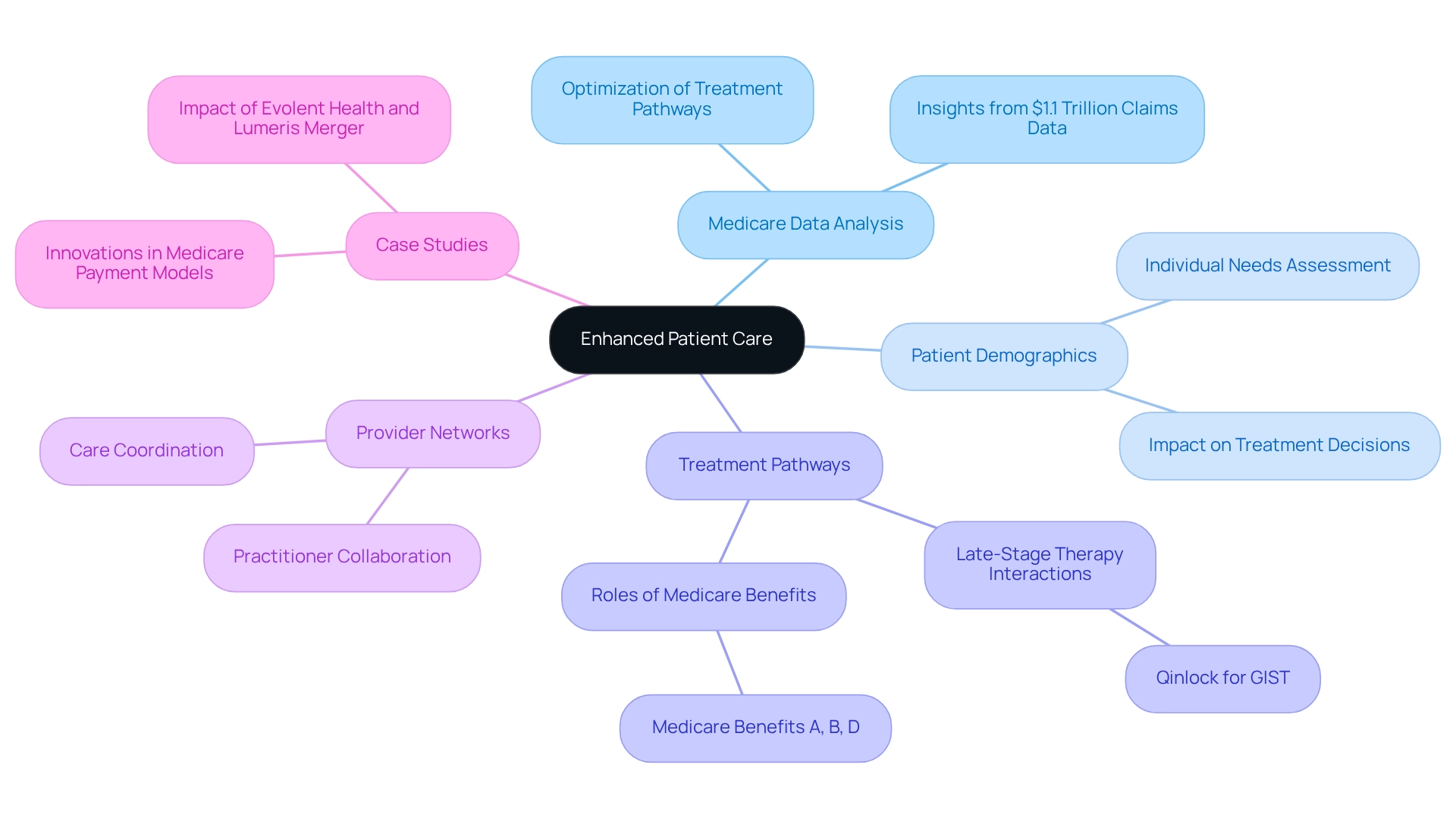
CareSet: Enhanced Patient Care Through Comprehensive Medicare Data Insights
CareSet harnesses its extensive analysis of over $1.1 trillion in annual Medicare claims data to provide medical professionals with critical insights into individual demographics, treatment trends, and practitioner networks. This innovative approach not only identifies gaps in support but also optimizes treatment pathways, significantly enhancing outcomes for patients.
For instance, the case study on oncology treatment options illustrates how timely interactions with healthcare providers regarding late-stage therapies, such as Qinlock for Gastrointestinal Stromal Tumor (GIST), can improve patient well-being. By equipping practitioners with actionable intelligence derived from insights into Medicare claims data, CareSet empowers informed decision-making that leads to better treatment and increased satisfaction.
As Jessica Walradt remarked, “It will be important for all stakeholders to work together to sustain and continually improve this important societal program.” The impact of such comprehensive data analysis is evident in its ability to reduce hospital admissions and enhance care coordination, ultimately fostering a more effective medical service delivery system.
Furthermore, understanding how providers navigate the patient’s journey from diagnosis to treatment—including the specific roles of Medicare benefits A, B, and D—enables healthcare professionals to better address individual needs. Additionally, analyzing the relationships among HCPCS, ICD, DRGs, and NCDs within a therapeutic area provides deeper insights into treatment pathways and enriches the overall understanding of individual health dynamics.
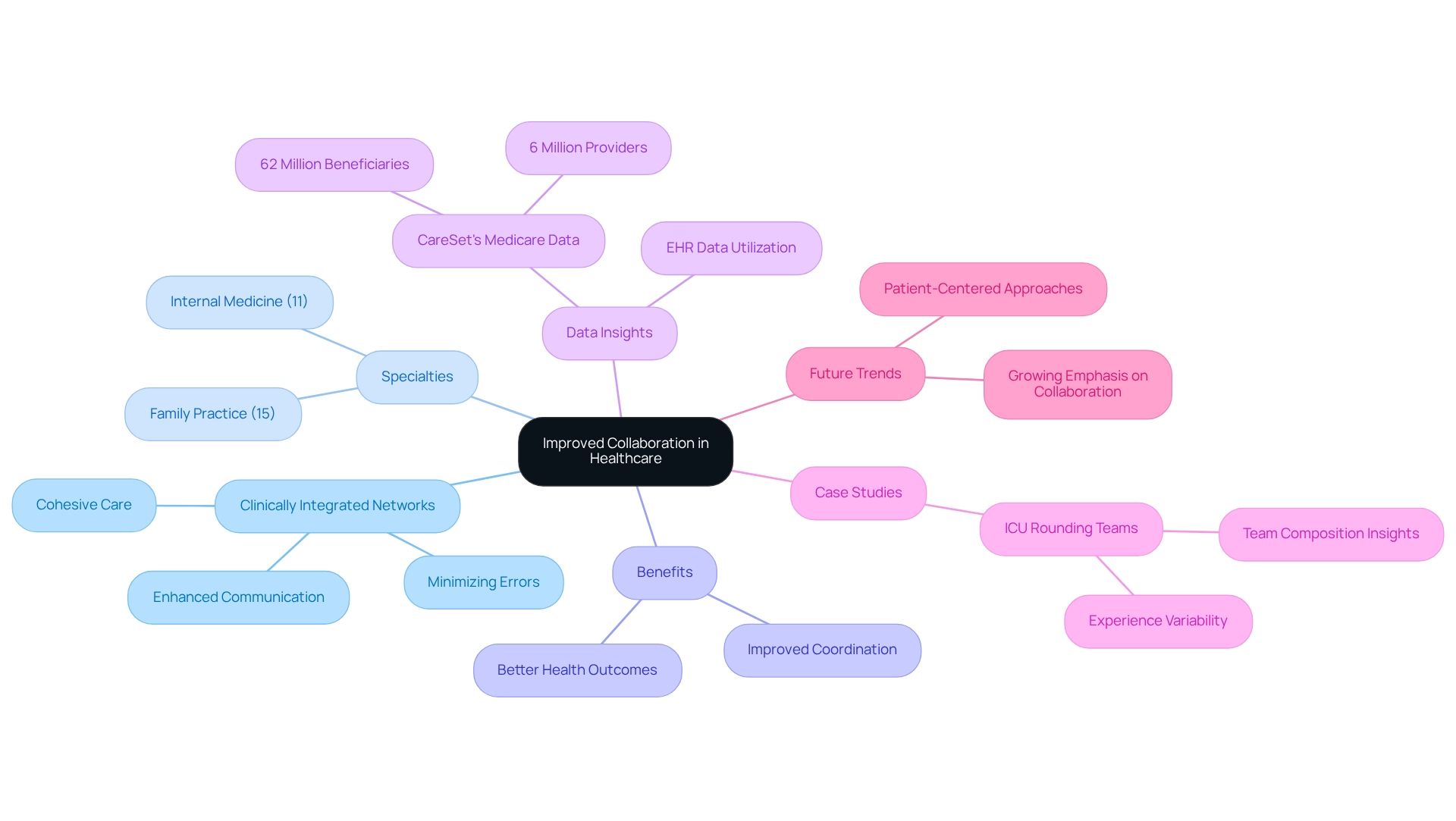
Improved Collaboration: Enhanced Coordination Among Healthcare Providers
Clinically integrated networks are crucial for enhancing cooperation among healthcare professionals by providing a robust platform for shared information and resources. This improved coordination fosters seamless communication, which is crucial for minimizing errors and ensuring that all parties involved in a patient’s treatment are aligned. As a result, individuals benefit from more cohesive and comprehensive care, ultimately leading to better health outcomes.
Statistics reveal that the most common specialties within these networks include family practice (15%) and internal medicine (11%). This diversity not only highlights the extensive expertise available in clinically integrated networks but also bolsters the ability to effectively address various healthcare needs, thereby enhancing collaborative efforts among practitioners.
Healthcare professionals have expressed strong support for the benefits of improved coordination in patient treatment. Dr. Mazhar Jaffry, for instance, emphasizes that “data privacy and security are significant concerns for CINs,” underscoring the necessity of building trust in collaborative initiatives to facilitate effective communication and coordination.
Moreover, leveraging CareSet’s comprehensive Medicare data insights can empower healthcare stakeholders to refine strategies for patients receiving medical services. By utilizing data from over 62 million beneficiaries and 6 million providers, clinically integrated networks can make informed decisions that improve outcomes for individuals.
Case studies, such as those examining Intensive Care Unit (ICU) rounding teams, demonstrate that electronic health record (EHR) data can yield valuable insights into team composition and experience. These findings suggest that enhanced coordination can improve team performance in critical care settings, ultimately contributing to better integration of individuals within CINs.
The substantial impact of clinically integrated networks on individual treatment coordination is noteworthy. By improving communication among caregivers, these networks not only streamline processes but also enhance outcomes for patients. Separate sensitivity analyses have confirmed the robustness of these results, further validating the effectiveness of CINs. As we move into 2025, the emphasis on collaboration within clinically integrated networks (CINs) continues to grow, reflecting a broader trend towards integrated support models that prioritize patient-centered approaches. To fully harness the advantages of clinically integrated networks, healthcare professionals should consider how CareSet’s data solutions can bolster their strategies for improved client care and business success.
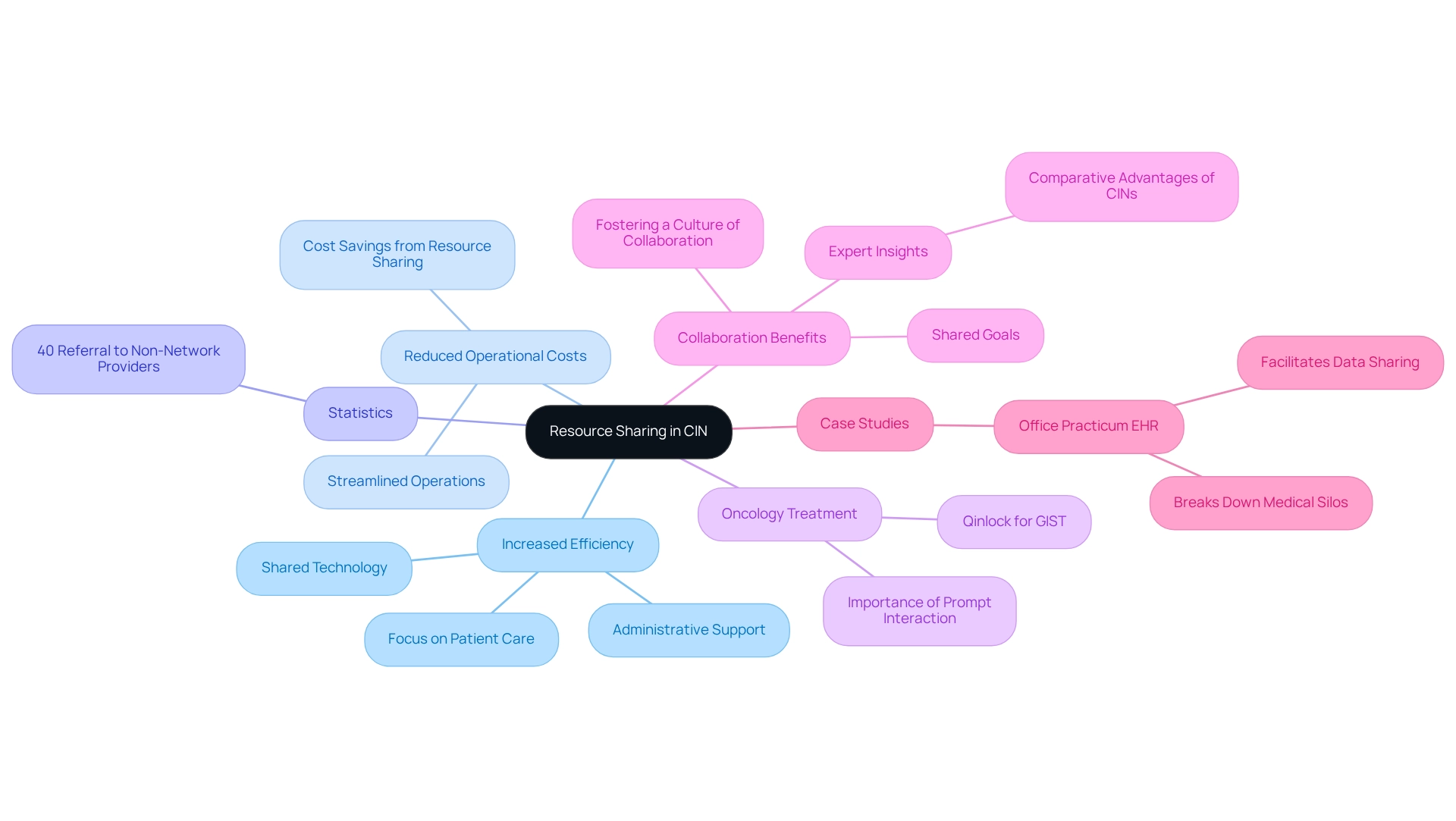
Resource Sharing: Increased Efficiency and Reduced Operational Costs
A key benefit of joining clinically integrated networks is the ability to share resources among practitioners. This includes shared technology, administrative support, and clinical best practices, which collectively contribute to significant operational cost reductions. For instance, a recent study revealed that over 40% of employed doctors within a particular 13-hospital CIN were directing individuals to non-network practitioners. This statistic underscores the potential for enhanced collaboration and resource utilization, as increasing network participation can lead to improved management of individuals and decreased referral leakage.
In the realm of oncology treatment, particularly concerning late-stage therapies like Qinlock for Gastrointestinal Stromal Tumor (GIST), prompt and significant interaction with medical providers is crucial. CareSet’s leadership in unlocking Medicare data empowers medical organizations to enhance their outreach and support for physicians, ensuring they are well-informed about treatment options. By pooling resources, medical organizations can optimize operations, enabling them to focus more on individual treatment rather than administrative duties. The Office Practicum EHR exemplifies this by facilitating data sharing among pediatric practices, dismantling medical silos, and enhancing data flow. This technology not only improves operational efficiency but also allows providers to devote more time to caring for individuals, ultimately resulting in cost savings through reduced administrative burdens.
The advantages of resource sharing extend beyond immediate cost reductions; they foster a culture of collaboration and shared goals, ultimately enhancing service delivery. As medical administrators increasingly recognize the value of collaboration, the potential for operational cost reduction through shared resources becomes a compelling incentive for practices to join clinically integrated networks. Expert insights suggest that such collaborative frameworks not only improve outcomes for individuals but also optimize the overall healthcare delivery system. To capitalize on these insights, practices should actively pursue opportunities to engage with clinically integrated networks, ensuring they maximize the benefits of resource sharing for enhanced operational efficiency.
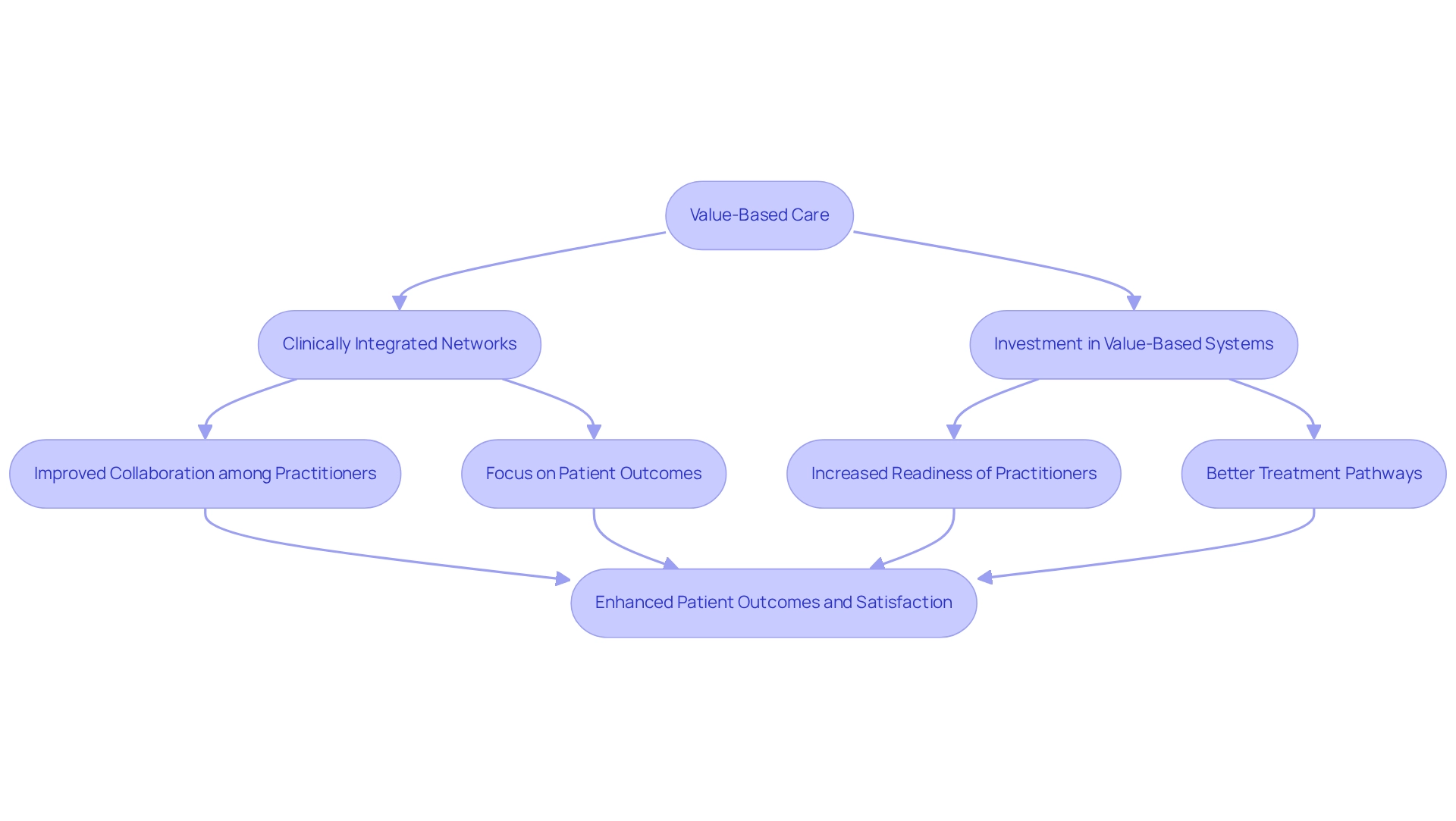
Value-Based Care: Alignment of Incentives for Better Patient Outcomes
Clinically integrated networks are essential for advancing value-based healthcare by aligning the incentives of all practitioners involved. This strategic alignment shifts the focus from merely increasing service volume to delivering high-quality support, which is essential for enhancing patient outcomes. Notably, in 2023, strategic purchases by health insurers and medical practitioners constituted 55% of total investment activity in the value-based system. This substantial investment underscores the growing emphasis on clinically integrated networks, which are designed to foster collaboration among practitioners and improve service delivery. Data indicates that fewer than half of primary health physicians in the U.S. currently receive payments through value-based payment models, highlighting a significant opportunity for improvement. As these networks prioritize individual outcomes, they ensure that patients receive the most effective treatments, leading to better health results and reduced healthcare costs over time. CareSet’s comprehensive Medicare data solutions provide insights into the treatment pathways of over 62 million beneficiaries, enabling stakeholders to understand which interventions are most effective and how practitioners can optimize their strategies.
For example, a Clinicient survey from April 2017 revealed that only 38% of therapists were preparing for value-based payment models, while 65% expressed a lack of understanding of value-based support. This gap in readiness is particularly concerning, given that nearly half of the U.S. population experiences musculoskeletal pain annually, representing a substantial market growth area. By adapting to these evolving payment models, physical therapists can better meet the needs of these individuals, showcasing the potential for improved outcomes through aligned incentives. Expert opinions emphasize that aligning incentives is crucial for achieving enhanced results. Healthcare economists advocate for this approach, noting that it fosters cooperation among practitioners, ultimately elevating the quality of service delivered. As we advance further into 2025, the benefits of value-oriented health services within clinically integrated networks will continue to emerge, enhancing health outcomes and patient satisfaction. With CareSet’s insights into network systems and pharmaceutical usage, healthcare stakeholders can make informed decisions that enhance patient treatment and business success.
Negotiating Power: Improved Reimbursement Rates Through Network Participation
Participating in clinically integrated networks significantly enhances a practitioner’s negotiating power with insurance companies and payers. By presenting a unified front, network members can leverage collective bargaining to secure improved reimbursement rates and terms, which are crucial for their financial sustainability. This collaborative approach not only permits practitioners to negotiate more advantageous contracts but also guarantees they receive equitable compensation for the quality care they deliver.
Statistics indicate that the majority of physicians now operate within multispecialty practices, a trend that is on the rise. This shift underscores the increasing significance of clinically integrated networks in enhancing overall medical efficiency through coordinated efforts. For instance, a recent analysis of UnitedHealth Group’s physician payment practices revealed that the company pays its own practices significantly more than other physician groups for similar services. This disparity highlights the potential for clinically integrated networks to negotiate better rates by consolidating their influence and addressing conflicts of interest that can inflate costs for consumers. Such insights are essential, particularly considering the Medicare Advantage Value-Based Insurance Design Model, which emphasizes the necessity for effective reimbursement strategies in the changing medical landscape.
Moreover, network participation has demonstrated an improvement in reimbursement rates for professionals. As clinically integrated networks evolve in 2025, their influence on negotiating power with payers is anticipated to increase, allowing healthcare professionals to achieve improved financial outcomes. CareSet’s comprehensive Medicare data insights can empower healthcare stakeholders by providing actionable information that enhances negotiation strategies within CINs. Expert insights indicate that as clinically integrated networks improve, they will play a crucial role in influencing reimbursement strategies, ultimately benefiting both healthcare professionals and individuals. As Carmouche aptly noted, from a consumer’s standpoint, the current system lacks transparency, which makes the role of clinically integrated networks even more critical in advocating for fair practices.
Enhanced Patient Engagement: Strategies for Improved Adherence and Outcomes
Clinically integrated networks utilize diverse strategies to enhance individual engagement, such as:
- Personalized communication
- Educational resources
- Proactive follow-up care
Actively involving individuals in their medical journey allows caregivers to significantly improve compliance with treatment plans, fostering a sense of ownership over their well-being. This heightened engagement correlates with improved health outcomes, as demonstrated by a case study where a hospital achieved $12 million in savings by reducing emergency room visits through medication adherence initiatives.
Furthermore, with 80% of individuals preferring digital communication with medical providers, integrating technology into these strategies is essential for modern medical delivery. For instance, the use of QR code-activated surveys simplifies feedback collection, thereby enhancing individual involvement. Additionally, proactive communication strategies, such as requesting extended refills, have yielded a 54% response rate, with 47% of requests approved, showcasing their effectiveness in improving adherence.
The result is not only enhanced health outcomes but also increased satisfaction and loyalty among individuals, highlighting the critical role of engagement in boosting treatment adherence and overall effectiveness within clinically integrated networks.
Advanced Analytics: Identifying Care Gaps and Improving Treatment Pathways
Advanced analytics are essential for the effectiveness of clinically integrated networks, enabling medical professionals to identify service gaps and improve treatment pathways. By utilizing extensive Medicare data solutions from CareSet, which include insights from over 62 million beneficiaries and 6 million providers, medical professionals can pinpoint areas where support may be lacking or where individuals are at risk of non-adherence. This proactive strategy facilitates timely interventions, ensuring that individuals receive the appropriate care at the right moment—essential for enhancing health outcomes.
Looking ahead to 2025, the integration of advanced analytics is anticipated to become even more sophisticated, with medical institutions increasingly adopting AI and big data technologies. Studies indicate that organizations with robust infrastructure, thorough staff training, and strong management support are more likely to successfully implement these technologies. This underscores the critical role that foundational elements play in the adoption of advanced analytics.
The execution of healthcare engagement analytics has shown substantial operational cost advantages, with an average return on investment (ROI) of 3.2:1 over three years, and some organizations reporting ROIs reaching as high as 5.7:1. These figures, derived from case studies on operational cost benefits, highlight the financial advantages of utilizing data analytics in healthcare.
Recognizing treatment gaps through data analysis not only boosts adherence but also enhances overall effectiveness. Insights into patient treatment pathways, including the examination of Medicare claims data, provider interventions, and treatment approvals, are essential for developing targeted health strategies. Specialists in the area stress the significance of employing advanced analytics to reveal these gaps, which can result in more efficient treatment strategies. As Hani Al-Dmour observed, “We want to thank every respondent for assisting us in gathering the data for this research,” emphasizing the importance of data collection in advancing improvements in health services. As medical services continue to evolve, the capacity to utilize data analytics will be crucial in enhancing treatment and operational efficiency within clinically integrated networks.
Innovation in Care Delivery: Implementing New Practices and Technologies
Clinically integrated networks act as catalysts for innovation in service delivery, fostering a collaborative environment where providers can share best practices and adopt new technologies. This culture of innovation not only encourages the adoption of advanced treatments and support models but also significantly enhances the overall quality of service for individuals.
CareSet’s comprehensive Medicare data insights empower medical stakeholders by delivering critical information on drug utilization and treatment pathways, thereby enhancing patient care and driving business success. Notably, the incorporation of artificial intelligence in medical services has been transformative, with the global market for AI in drug discovery projected to grow from USD 1.2 billion in 2022 to USD 12.8 billion by 2032, reflecting a compound annual growth rate (CAGR) of 27.5%. Furthermore, the vertical integration model segment is expected to record USD 15.5 billion by 2023, underscoring the financial impact and significance of clinically integrated networks within the medical landscape.
Additionally, case studies illustrate the effectiveness of clinically integrated networks in enhancing medical efficiency. A prime example is the role of Integrated Delivery Networks (IDNs), designed to streamline medical services by coordinating various components of the system. This integration has led to improved coordination of services, decreased duplicate testing, and enhanced overall efficiency for individuals, which are all advantages of clinically integrated networks. CareSet’s monthly Medicare updates enhance provider involvement by offering insights into essential business inquiries, such as which conditions providers identify and manage, and how individuals navigate their treatment journeys.
As healthcare providers embrace innovative practices, they can profoundly influence the quality of service. Statistics reveal that organizations utilizing predictive analytics have reported favorable outcomes, with 42% observing enhanced satisfaction and 39% realizing cost savings. The Society of Actuaries highlights that the use of predictive analytics yields positive results, reinforcing the necessity of adopting new technologies within clinically integrated networks to ensure that patients receive the most effective and efficient care possible. Furthermore, CareSet addresses urgent data requirements while promoting long-term strategic development for partners, emphasizing the strategic significance of clinically integrated networks within the broader framework of analytics and decision-making in the medical field.
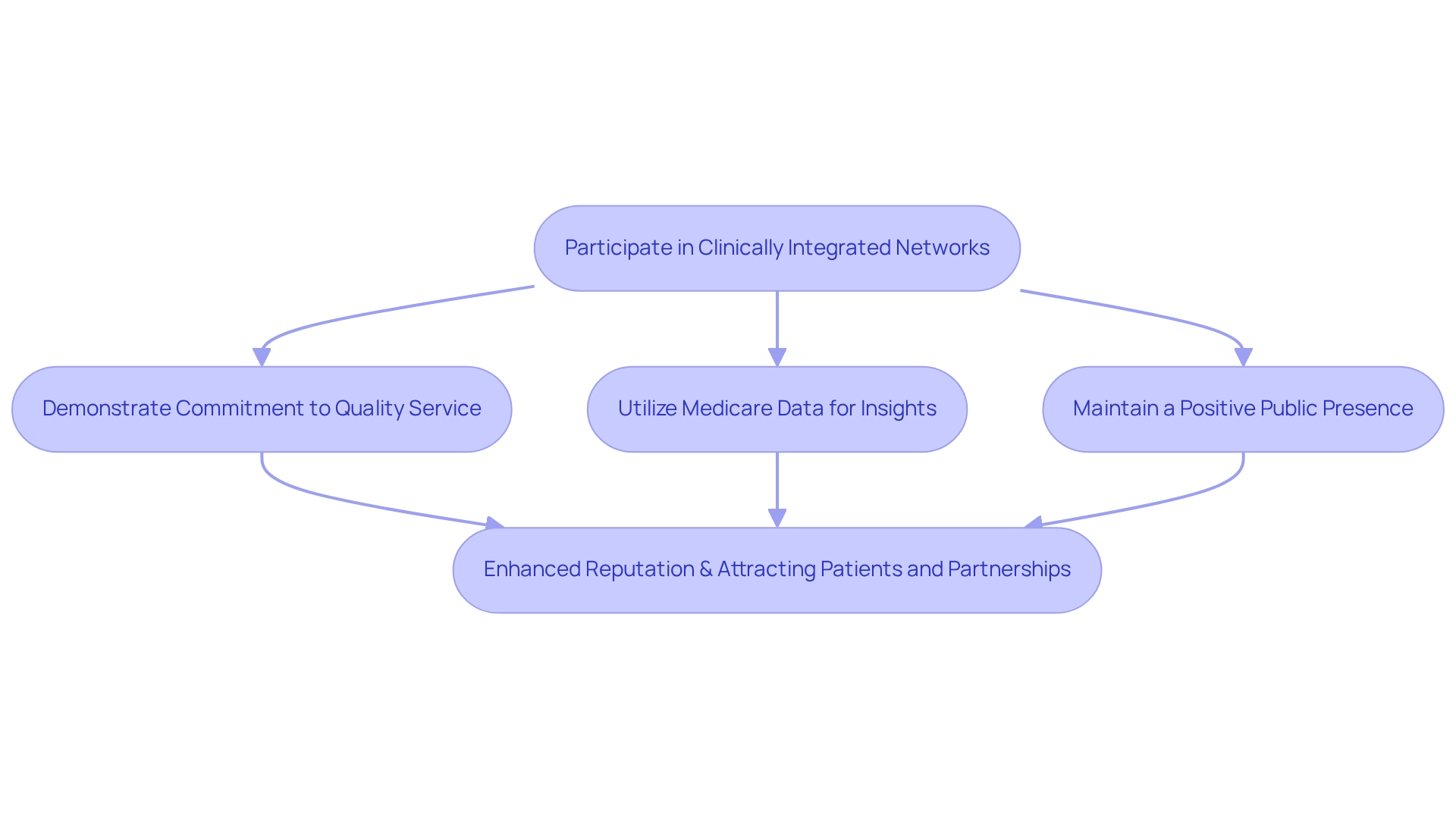
Reputation Enhancement: Attracting Patients and Partnerships Through Network Participation
Joining clinically integrated networks significantly enhances a medical professional’s reputation within the community. By demonstrating a commitment to quality service and collaborative methods, practitioners attract a broader clientele and forge valuable partnerships with other healthcare organizations. This improved reputation leads to an increased influx of clients and opens doors for collaborative initiatives that elevate care delivery standards.
Statistics reveal that participants engaged in network involvement experience notable improvements in their reputation. Negative news is reported to have three times the impact of positive news, underscoring the necessity of maintaining a robust, positive presence through network participation. This is crucial for medical professionals aiming to bolster their reputation and attract clients.
Expert insights suggest that collaboration within these networks nurtures trust and transparency, essential for drawing in individuals. Paul Gileno, President of the U.S. Pain Foundation, underscores the complexities of cost and value in healthcare, stating, “Cost and value are complicated topics—as individuals and advocates who have received fair reimbursement for services from pharma, we’re in a precarious position in regards to defending drug prices publicly. We really need your support in this conversation.” This perspective reinforces the idea that a commitment to quality care significantly influences patient choices, as patients increasingly seek out practitioners dedicated to excellence.
Case studies, such as CareSet’s initiative focusing on oncology treatment options like Qinlock for Gastrointestinal Stromal Tumor (GIST), exemplify how leveraging Medicare data can enhance engagement with healthcare professionals. By utilizing real-time data insights, healthcare professionals can improve interactions with physicians, ensuring timely and meaningful discussions regarding treatment options. This data-driven approach not only enhances user experience but also promotes quality outcomes, thereby strengthening the organization’s reputation.
Ultimately, the impact of a commitment to quality services on client attraction is profound. By actively participating in clinically integrated networks and utilizing Medicare data to inform their practices, professionals can effectively enhance their reputation, attract more individuals, and cultivate partnerships that improve service delivery. To embark on this journey, healthcare professionals should engage with existing networks, seek partnerships that align with their commitment to quality service, and utilize client feedback to continually refine their offerings.
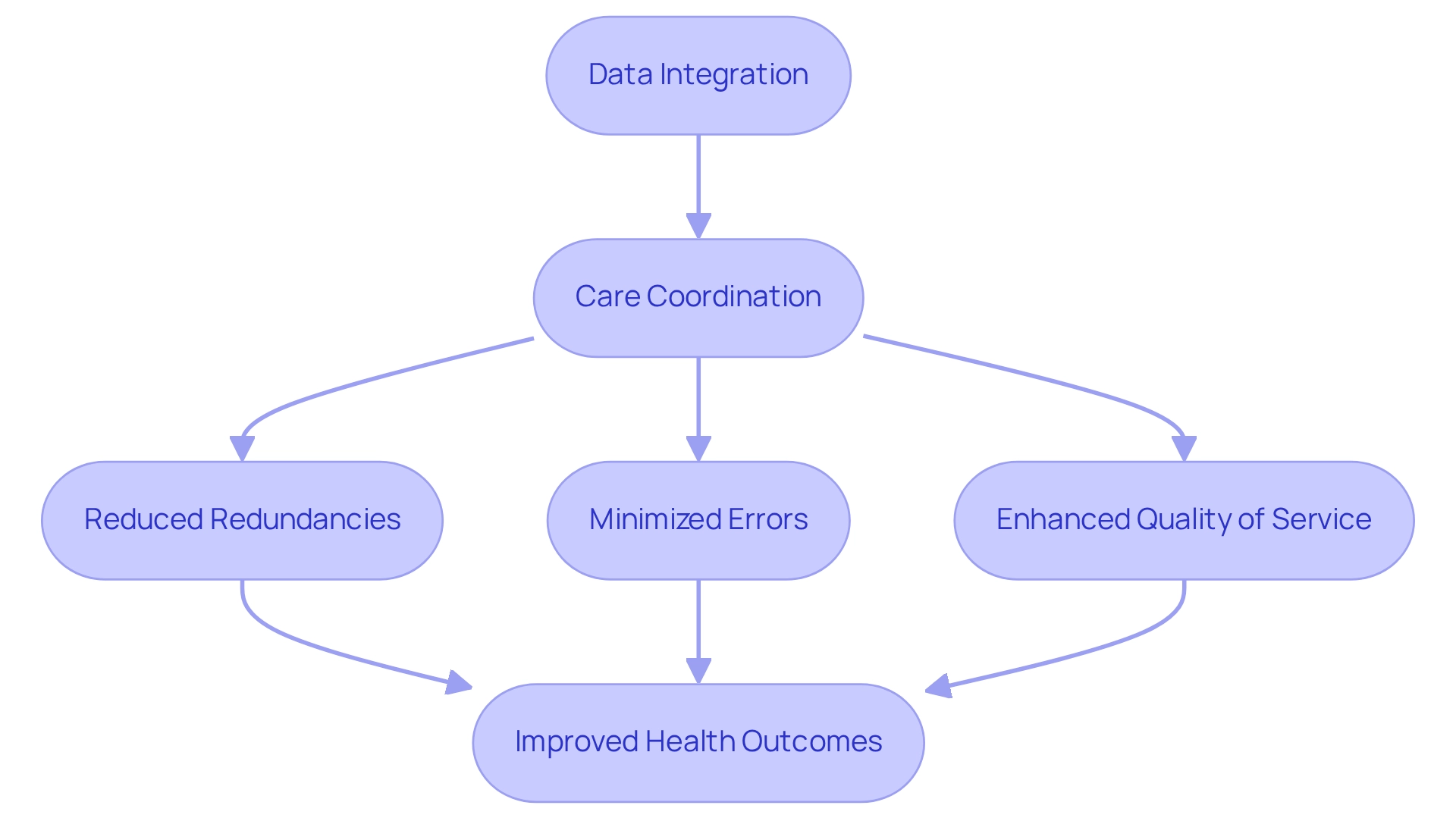
Improved Health Outcomes: Benefits of Data Integration and Care Coordination
The combination of information and coordination within clinically integrated networks is essential for achieving significantly improved health outcomes for individuals. By ensuring that all providers involved in an individual’s treatment have access to the same information, these networks effectively reduce redundancies, minimize errors, and enhance the overall quality of service. This comprehensive approach not only aids individual clients but also boosts the overall efficiency and effectiveness of the medical system. Notably, inefficiencies in the US healthcare system waste up to 25% of expenditures, underscoring the critical need for improved data integration and coordination of services.
In 2025, organizations utilizing population health analytics reported a remarkable 76% improvement in key chronic disease management metrics, including blood pressure control, diabetes management, and medication adherence rates. Such statistics underscore the transformative impact of coordinated support on individual health outcomes, particularly as data integration plays a vital role in facilitating these advancements.
A significant case study exemplifies the effectiveness of the Transitional Management (TCM) program, which emphasizes robust communication during transitions between support settings. Participation in this program has been shown to reduce patient readmission rates by nearly 87%, demonstrating how strong coordination and follow-up support in the critical first 30 days post-hospital discharge can lead to improved patient outcomes. This aligns with CareSet’s comprehensive strategy, which leverages insights from over 62 million Medicare beneficiaries and 6 million providers to foster long-term strategic growth for partners in the healthcare sector.
Moreover, analysts highlight that health plans with outstanding beneficiary-reported service coordination achieve higher performance scores, as noted in the Journal of General Internal Medicine. This reinforces the notion that efficient coordination of services is essential for enhancing health outcomes. As the healthcare landscape continues to evolve, the advantages of data integration and care coordination will remain vital for improving patient care and promoting long-term strategic growth within clinically integrated networks in the healthcare industry.
Conclusion
The integration of data and collaboration through Clinically Integrated Networks (CINs) is reshaping the landscape of healthcare, demonstrating a powerful model for improving patient care and outcomes. By harnessing the vast insights from Medicare claims data, organizations like CareSet are not only identifying gaps in care but also enhancing treatment pathways and care coordination. This data-driven approach empowers healthcare providers to make informed decisions that ultimately lead to better health outcomes and increased patient satisfaction.
The emphasis on collaboration within CINs facilitates improved communication among providers, reducing errors and ensuring a more cohesive care experience for patients. As these networks continue to evolve, the collective bargaining power they offer enhances negotiating capabilities with insurers, leading to better reimbursement rates for providers. This financial sustainability is crucial as the industry shifts towards value-based care, where the focus is on delivering high-quality care rather than merely increasing service volume.
Moreover, the commitment to patient engagement through personalized communication and proactive follow-up care fosters adherence to treatment plans, further reinforcing the positive impact of CINs on health outcomes. With advanced analytics identifying care gaps and informing treatment strategies, healthcare organizations are poised to deliver more effective and efficient care.
As the healthcare system continues to face challenges, embracing the collaborative and innovative framework that CINs provide is essential. By actively participating in these networks and leveraging comprehensive data insights, healthcare providers can not only enhance their reputation but also contribute to a more effective healthcare delivery system that prioritizes patient-centered care. The future of healthcare lies in collaboration, data integration, and a steadfast commitment to quality outcomes for all patients.


