Overview
The article delineates seven pivotal benefits of claims clearinghouses that significantly enhance healthcare efficiency. These benefits encompass:
- Improved accuracy
- Expedited payments
- Cost savings
- Enhanced compliance with regulations
Evidence substantiates these advantages, demonstrating that claims clearinghouses not only streamline processes but also reduce errors and facilitate timely reimbursements. Ultimately, this leads to heightened patient satisfaction and operational effectiveness within healthcare organizations.
Introduction
In the rapidly evolving landscape of healthcare, claims clearinghouses have emerged as pivotal intermediaries that streamline the claims submission process between providers and payers. By automating and standardizing claims data, these entities enhance operational efficiency and significantly reduce errors. This ensures that healthcare organizations can concentrate more on patient care rather than administrative burdens. As the demand for accurate and timely reimbursements escalates, it becomes essential for stakeholders to comprehend the transformative impact of clearinghouses on financial performance and patient satisfaction.
This article explores the multifaceted benefits of claims clearinghouses, examining how they foster improved communication, accelerate reimbursement cycles, and ultimately enhance the overall healthcare experience.
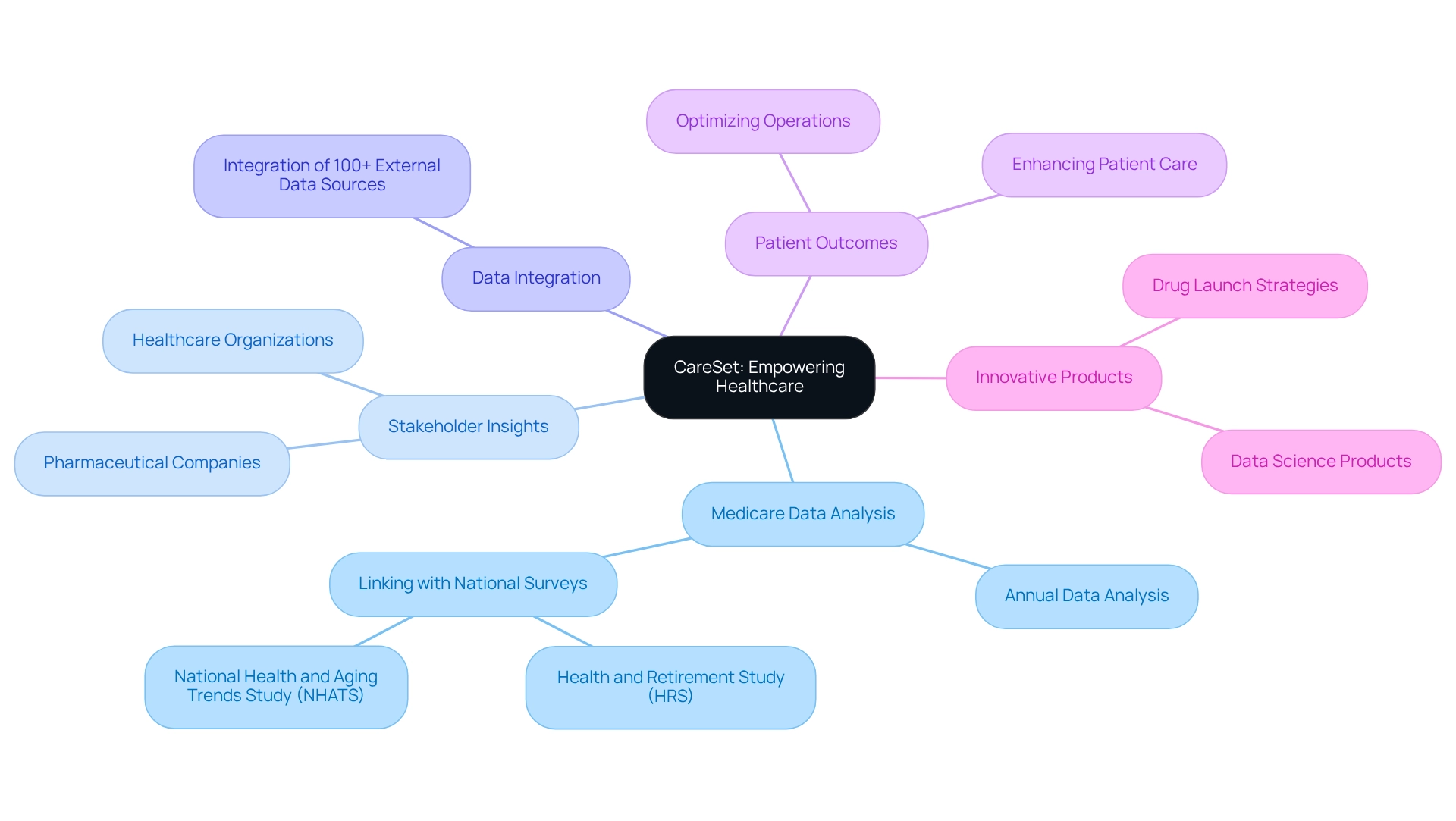
CareSet: Empowering Healthcare with Comprehensive Medicare Data Insights
CareSet stands at the forefront of medical analytics, specializing in the extraction and interpretation of complex Medicare data. By analyzing over $1.1 trillion in annual data, CareSet equips stakeholders with actionable insights that foster informed decision-making. This expertise is crucial for pharmaceutical companies and healthcare organizations that rely on precise data to optimize operations and enhance patient care, while CareSet’s innovative approach empowers medical organizations to identify data gaps and map patient journeys, thus complementing the efficiency improvements provided by claims clearinghouses. This collaboration enables healthcare providers to refine their operations and significantly enhance patient outcomes, ultimately supporting the strategic initiatives of pharmaceutical market access managers.
Current trends in medical analytics underscore the increasing reliance on comprehensive data sources. CareSet integrates over 100 external data sources, enriching its analyses and offering a more holistic perspective on treatment patterns and patient demographics. A noteworthy case study, ‘PUTTING PATIENTS FIRST,’ illustrates how the integration of Medicare data with national surveys, such as the Health and Retirement Study (HRS) and the National Health and Aging Trends Study (NHATS), amplifies the depth of data available for research. This linkage allows for thorough investigations into health trends and outcomes among older adults, showcasing the transformative potential of insights derived from Medicare data.
Moreover, CareSet’s commitment to developing innovative data science products, such as [specific features of the products], further enhances drug launch strategies and medical insights, solidifying its role as a vital partner for pharmaceutical companies. By fostering long-term strategic growth and boosting medical efficiency, CareSet not only addresses pressing data needs but also facilitates the optimization of the lifecycle management of pharmaceutical products.
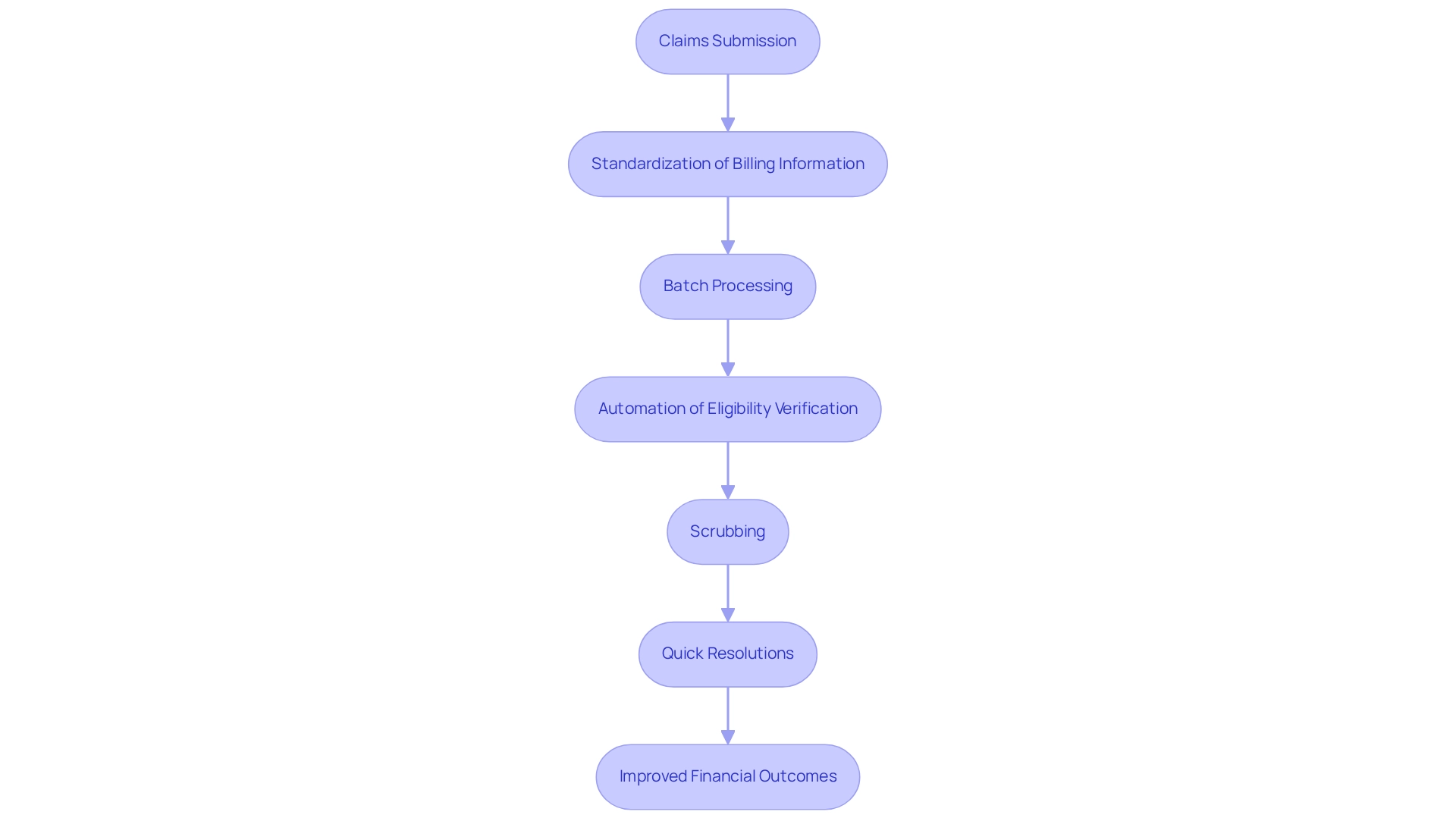
Operational Efficiency: Streamlining Claims Processing with Clearinghouses
Claims clearinghouses act as vital intermediaries that enhance the submission process between medical practitioners and payers. By converting medical billing information into standardized formats, claims clearinghouses simplify the complexities of submissions, enabling providers to file multiple requests simultaneously. This batch processing capability not only conserves time but also alleviates the administrative burden on medical personnel, allowing them to focus on patient care rather than paperwork.
Moreover, claims clearinghouses automate numerous aspects of request processing, including eligibility verification and scrubbing, which further boosts operational efficiency. This streamlined approach leads to quicker resolutions of requests and reduces the likelihood of errors that can delay payments. For instance, medical service providers utilizing intermediary services have reported notable improvements in their submission acceptance rates, thereby decreasing payment delays and enhancing overall revenue cycle management.
The adoption of advanced medical submission software by intermediaries has further elevated the accuracy and efficiency of processing, reflecting a clear trend toward operational excellence in the healthcare sector. As a result, healthcare organizations can expect not only streamlined processes but also improved financial outcomes, which underscores the crucial role of claims clearinghouses as intermediaries in modern healthcare operations.
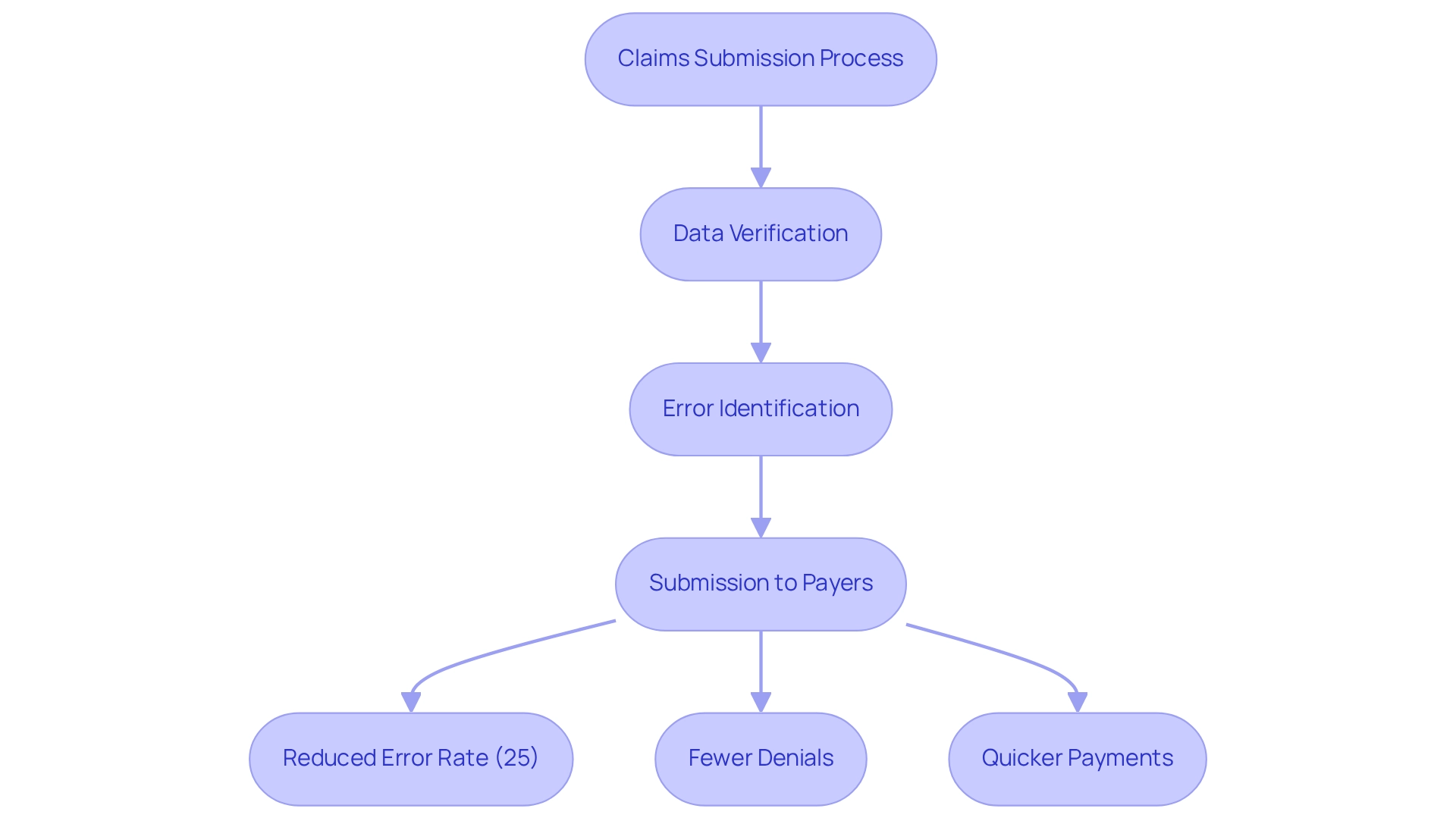
Enhanced Accuracy: Reducing Errors in Claims Submissions through Clearinghouses
One of the notable benefits of utilizing clearinghouses is their capacity to improve the precision of submissions. Claims clearinghouses conduct automated verifications on data to identify mistakes or missing information before the submissions are sent to payers. This procedure, commonly known as ‘scrubbing submissions,’ significantly lowers the error rate related to claims clearinghouses.
Studies show that submissions made electronically through intermediaries have a 25% reduced error rate compared to those sent via conventional paper methods. By identifying mistakes early, intermediaries assist medical practitioners in evading expensive denials and resubmissions, ultimately resulting in quicker payments and enhanced cash flow. As Jessica Glenn, Senior Product Owner, observes, “Prompt resubmission of rejected requests guarantees that suppliers receive compensation for services delivered in a timely manner.”
Moreover, the utilization of standardized medical request formats can greatly minimize the likelihood of rejections due to format mistakes, further highlighting the significance of claims clearinghouses in the medical landscape.
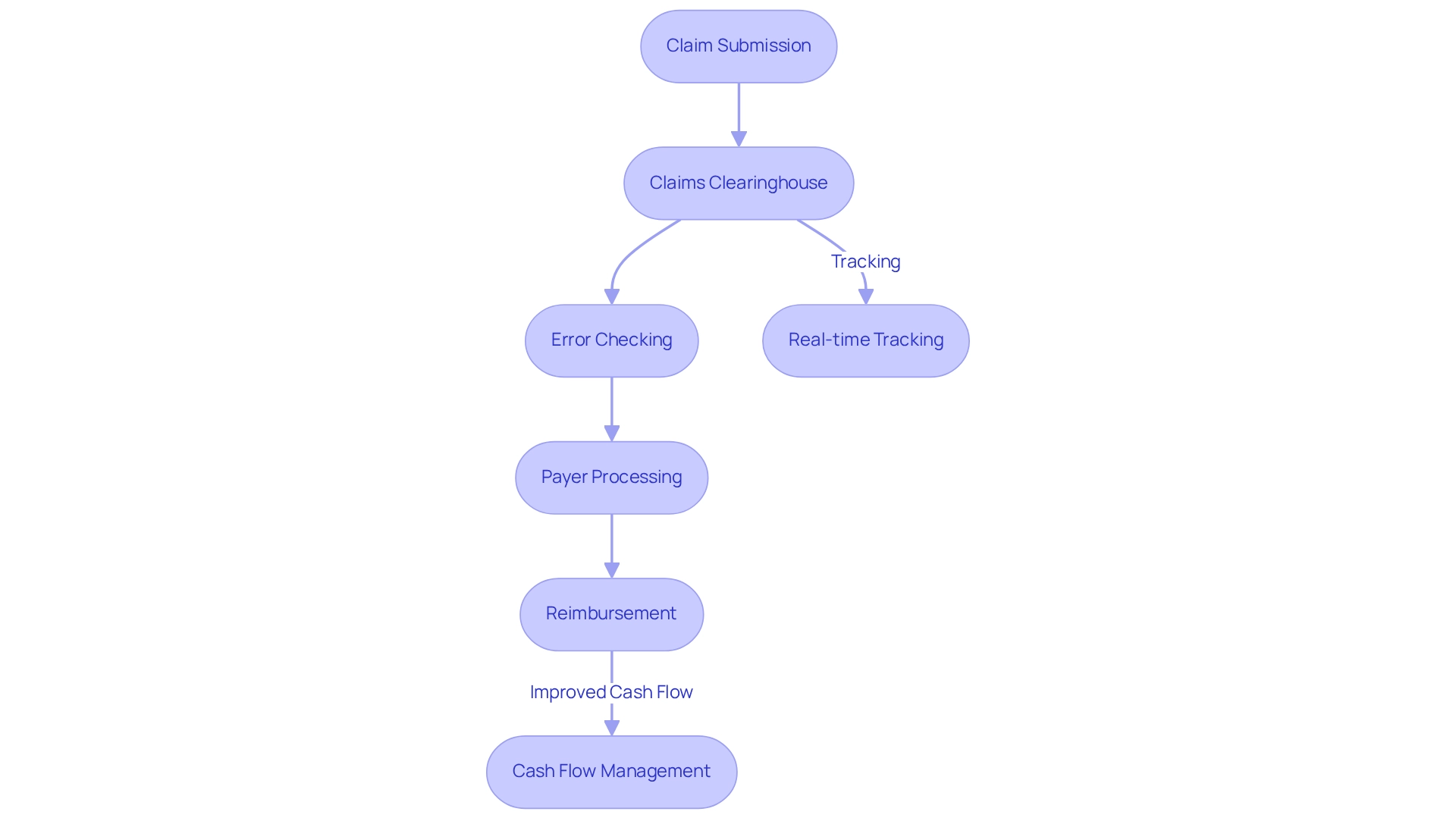
Faster Payments: Accelerating Reimbursement Cycles with Clearinghouses
Claims clearinghouses play a crucial role in expediting the reimbursement processes for medical practitioners, especially regarding Medicare submissions. By ensuring that claims are accurately formatted and devoid of errors, claims clearinghouses facilitate quicker processing by payers, which is vital for maintaining effective cash flow management. Moreover, claim processing centers offer real-time tracking of submissions, empowering professionals to monitor the status of their filings and swiftly address any issues that arise. This transparency not only boosts operational efficiency but also strengthens relationships between suppliers and payers, ultimately leading to enhanced financial outcomes.
Statistics reveal that medical suppliers utilizing intermediaries see a notable reduction in average reimbursement cycle durations, with many reporting improvements in payment speed by as much as 30%. Financial officers within the medical sector have recognized that the impact of intermediaries on cash flow is substantial, often resulting in a more stable financial environment.
For instance, organizations that have embraced intermediaries have achieved quicker payments, allowing them to reinvest in patient care and operational improvements. By leveraging these systems, medical practitioners can navigate the complexities of processing more effectively, ensuring they receive timely reimbursements and maintain a healthy revenue cycle. To fully capitalize on the benefits of these platforms, it is imperative for suppliers to understand how these systems interact with Medicare data and coding procedures, thereby refining their overall reimbursement strategies.
Cost Savings: Achieving Financial Efficiency with Claims Clearinghouses
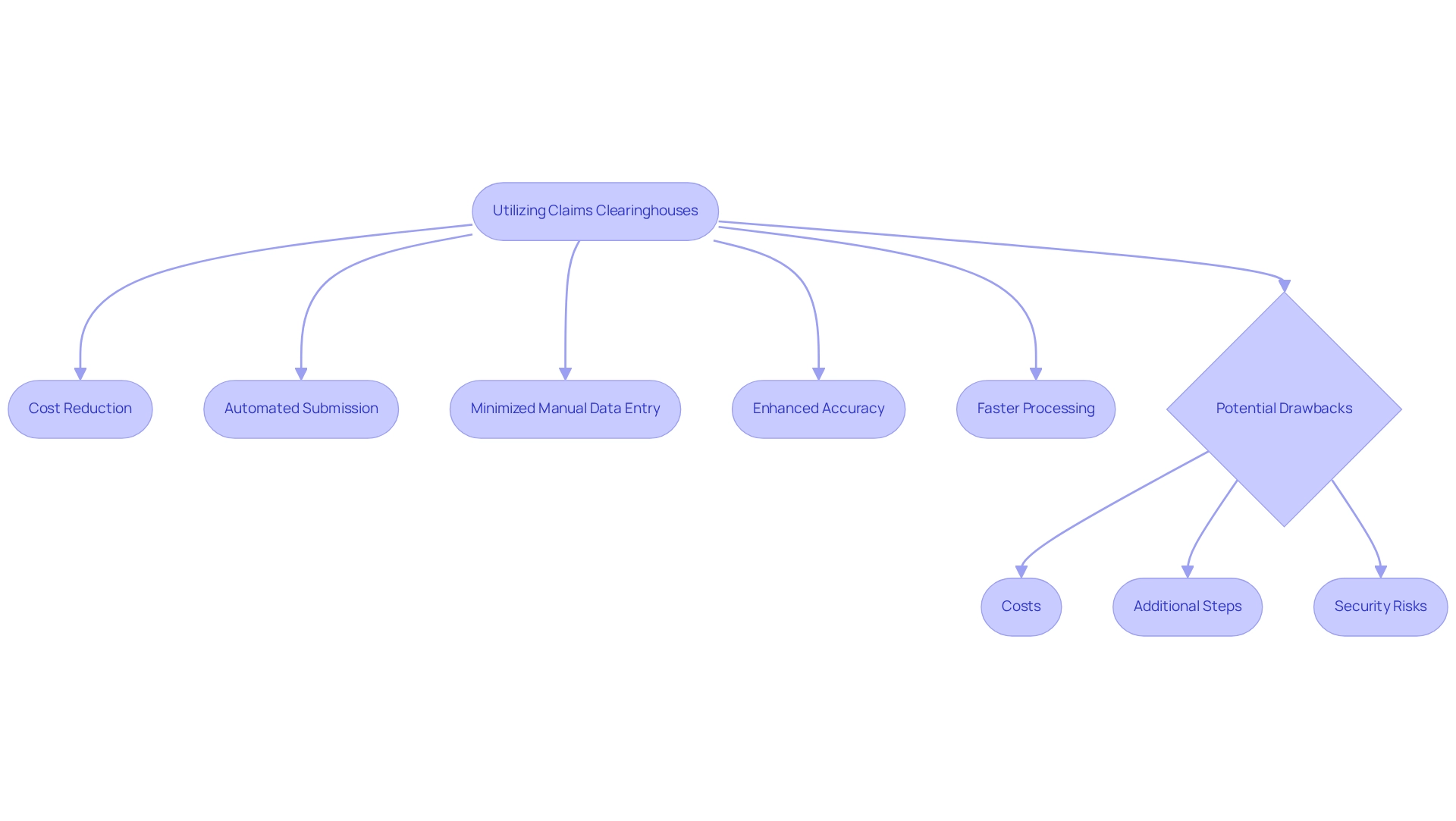
Utilizing billing intermediaries can lead to substantial cost reductions for healthcare providers. By automating the submission process and minimizing manual data entry, these organizations significantly lower administrative expenses associated with management. This advantage is particularly beneficial for smaller practices that often operate with limited resources.
The automation not only streamlines operations but also enhances the accuracy and speed of processing requests, thereby reducing the likelihood of costly denials and the need for rework. A study indicates that healthcare professionals leveraging claims processing centers can achieve an average administrative cost reduction of up to 30%. This financial efficiency empowers providers to reallocate resources toward patient care and other critical operational areas, ultimately enhancing overall service delivery.
Furthermore, it is crucial to distinguish between intermediaries and outsourced medical billing companies. While centralized organizations focus on the technical precision of claims, outsourced companies manage the entire billing process. Understanding this distinction enables healthcare providers to optimize their billing processes by selecting the right solution tailored to their specific needs.
However, potential drawbacks of using claims clearinghouses must also be acknowledged. These may encompass costs, additional steps in the billing process, and risks of security breaches involving sensitive patient information. As Stephen Beer notes, “There is also the risk of security breaches, as intermediaries store and transmit sensitive patient information.”
Moreover, expert opinions underscore the importance of processing centers in achieving financial efficiency. Healthcare managers have reported that transitioning to automated processing has led to significant improvements in their financial performance, with many citing enhanced cash flow and shorter billing cycle durations. By leveraging the capabilities of billing processing centers, medical practitioners can not only refine their invoicing procedures but also foster a more sustainable financial structure.
Regulatory Compliance: Ensuring Adherence to Healthcare Standards with Clearinghouses
Claims processing centers are pivotal in ensuring healthcare providers adhere to regulatory standards. Designed to comply with HIPAA regulations, these centers govern the privacy and security of patient information. Claims clearinghouses act as intermediaries to help safeguard sensitive information during the submission process. Moreover, claims clearinghouses remain vigilant to changing regulations and industry standards, ensuring claims are submitted in line with the latest requirements. This proactive compliance strategy assists medical providers in evading potential penalties while preserving the integrity of their billing practices.
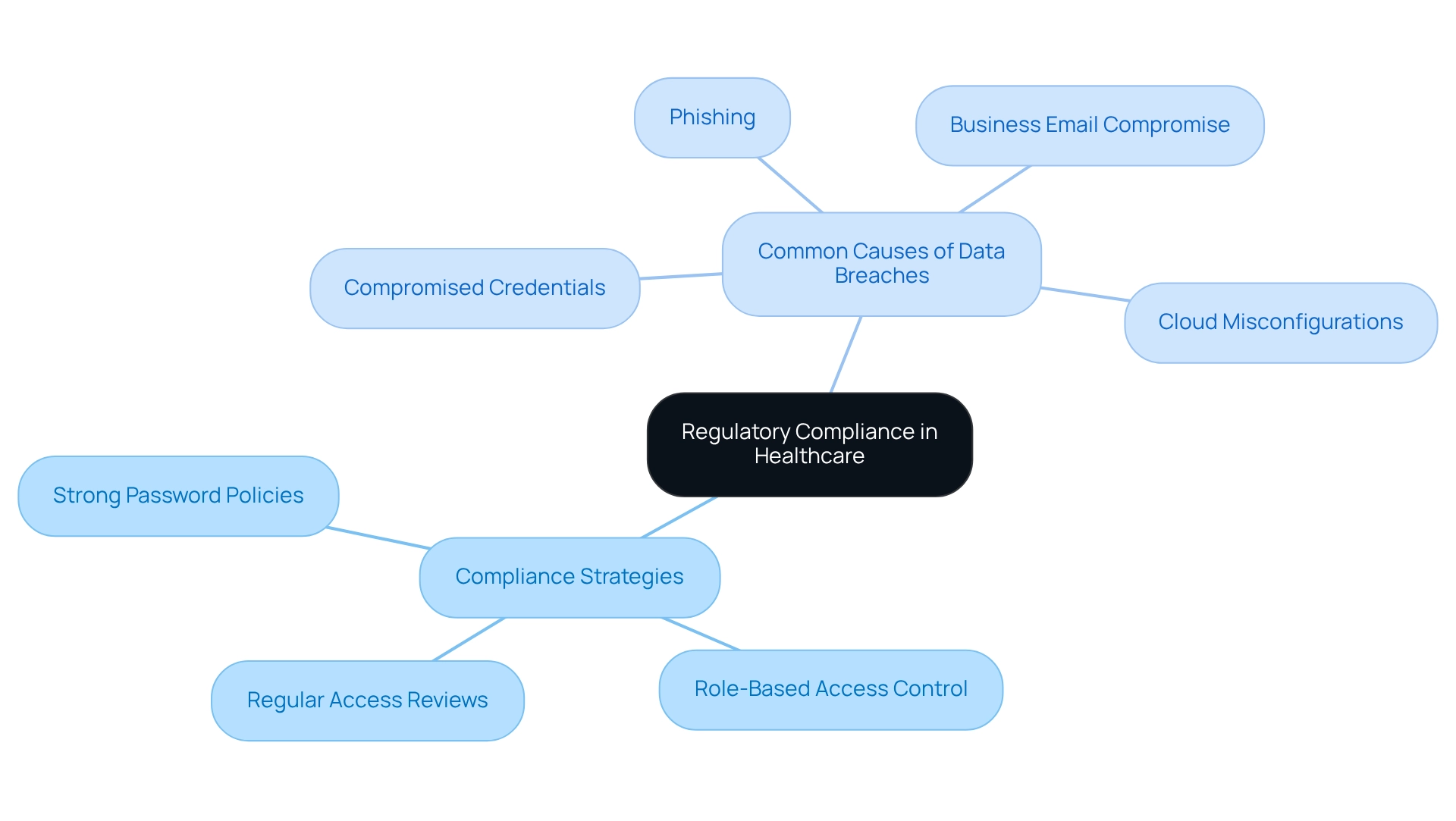
To further mitigate compliance risks, medical organizations should implement strategies such as:
- Strong password policies
- Role-based access control
- Regular access reviews
These measures are essential in addressing the four most common causes of medical data breaches:
- Compromised credentials
- Phishing
- Cloud misconfigurations
- Business email compromise
The HIPAA Journal reported that in 2022, the average rate of reported data breaches involving 500 or more records was approximately two reports per day, nearly double the amount in 2018. This statistic underscores the critical importance of stringent compliance measures, and expert insights reveal that claims clearinghouses not only facilitate compliance but also enhance operational efficiency. For instance, medical service providers utilizing intermediaries have reported improved compliance with HIPAA standards, demonstrating the effectiveness of these entities in navigating the complexities of medical regulations. As the landscape of healthcare data management continues to evolve, the role of intermediary organizations in ensuring compliance remains vital for safeguarding patient information and maintaining trust in the healthcare system.
Improved Patient Satisfaction: Enhancing Care Experience through Efficient Claims Processing
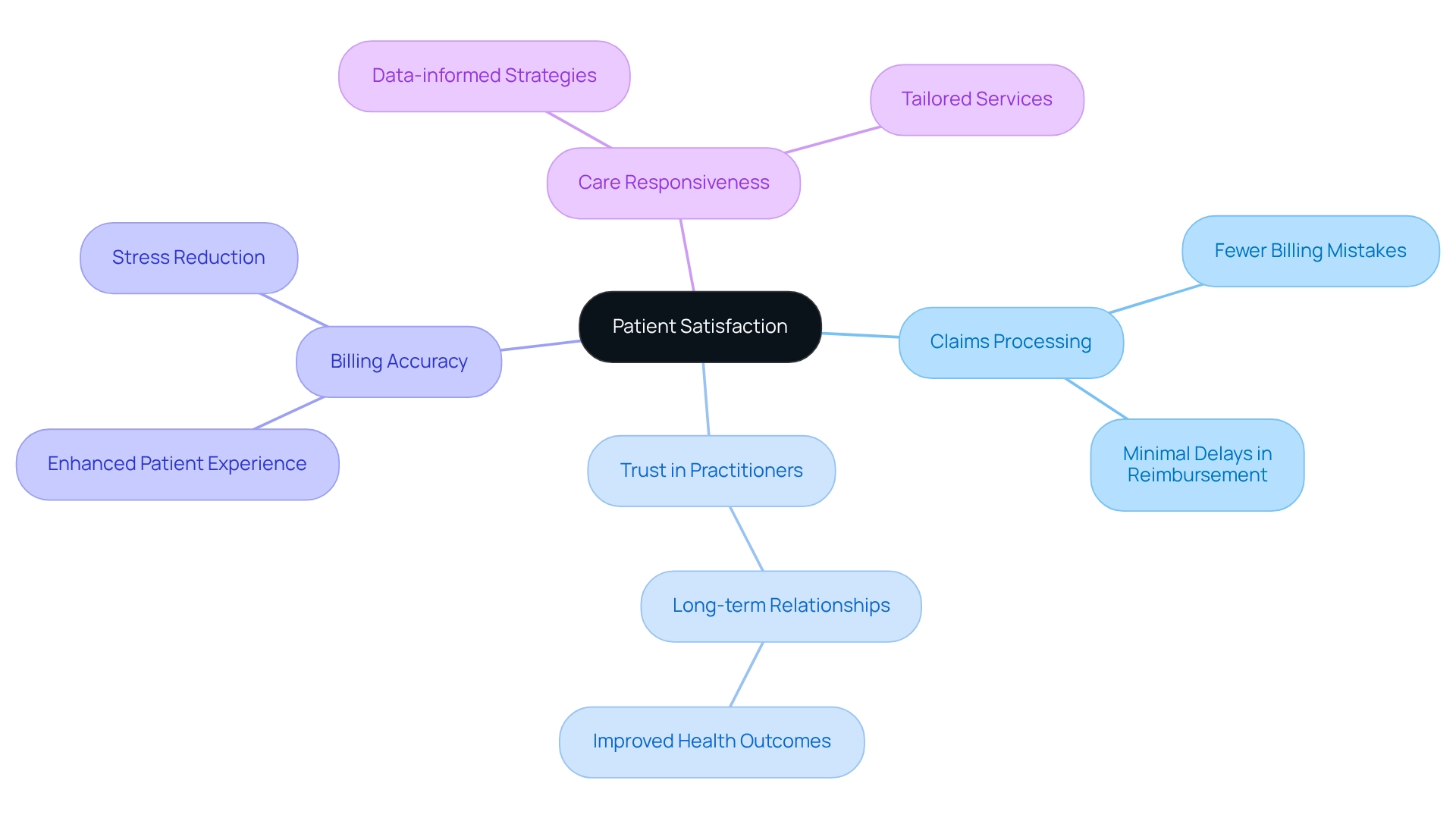
Effective processing of requests via claims clearinghouses is crucial for enhancing the patient experience. When requests are managed promptly and precisely, patients encounter fewer billing mistakes and experience minimal delays in reimbursement. This efficient process alleviates stress and confusion, fostering a more favorable interaction with healthcare professionals.
Timely and accurate billing details not only boost patient satisfaction but also cultivate trust in healthcare practitioners. This trust is essential for establishing long-term relationships, which are vital for achieving improved health outcomes. Indeed, research indicates that a 3.7-point reduction in the responsiveness of hospital personnel during the pandemic significantly impacted patient experiences, underscoring the necessity for effective claims clearinghouses to maintain high satisfaction levels.
Healthcare providers utilizing claims clearinghouses have reported notable enhancements in patient satisfaction. For instance, practices employing data-informed strategies have proactively addressed issues, tailoring services to meet patient needs and enhancing care responsiveness. Such instances underscore the importance of precise billing in fostering a positive medical environment, as affirmed by patient advocates who emphasize that billing accuracy is fundamental to patient trust and satisfaction.
Access to Valuable Data: Leveraging Insights from Claims Clearinghouses
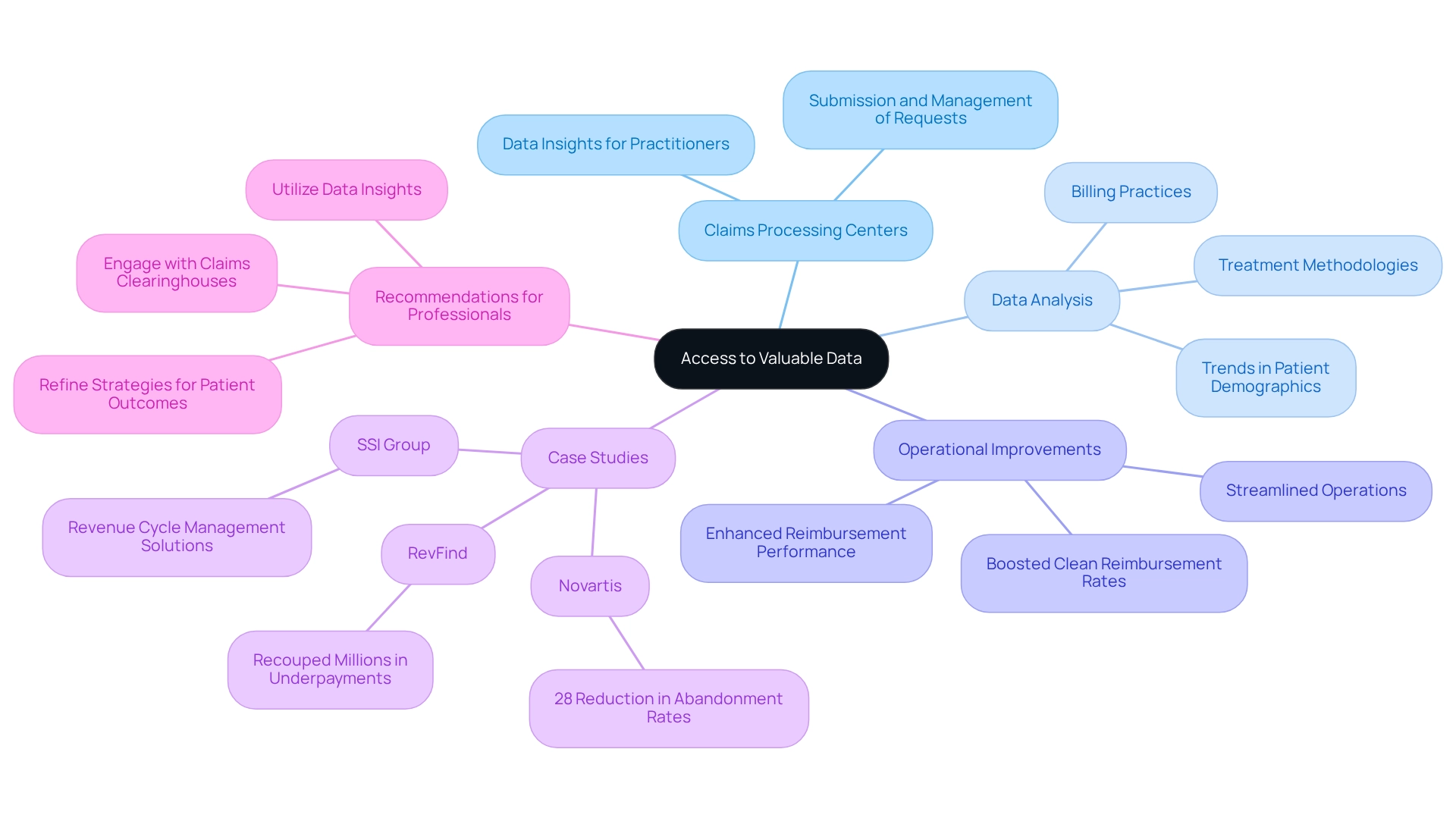
Claims processing centers serve a pivotal function within the medical ecosystem, facilitating not only the submission and management of requests but also delivering essential data insights to practitioners. By meticulously analyzing data related to services, medical organizations can uncover significant trends regarding patient demographics, treatment methodologies, and billing practices. This information is crucial for informed decision-making regarding resource allocation and the enhancement of patient engagement strategies.
Moreover, various claims clearinghouses, particularly those utilizing CareSet’s advanced data science products, provide sophisticated reporting tools that enable healthcare professionals to monitor their reimbursement performance over time. CareSet’s extensive Medicare data insights empower medical stakeholders to improve patient care and business outcomes by scrutinizing treatment pathways and provider interventions. This data-driven strategy allows healthcare organizations to streamline operations, boost clean reimbursement rates, and ultimately strengthen their revenue streams.
For instance, organizations leveraging insights from claims clearinghouses have reported substantial operational improvements; Novartis, for example, achieved a 28% reduction in abandonment rates for high-cost treatments. Additionally, clients using RevFind have recouped millions in underpayments through enhanced contract management and data analytics. Such statistics underscore the transformative impact of data analysis on medical decision-making and operational efficiency, reinforcing the critical notion that enhancing clean submission rates fortifies revenue streams for medical organizations.
To fully capitalize on these advantages, medical professionals are encouraged to actively engage with claims clearinghouses and harness the insights provided to refine their strategies and elevate patient outcomes.
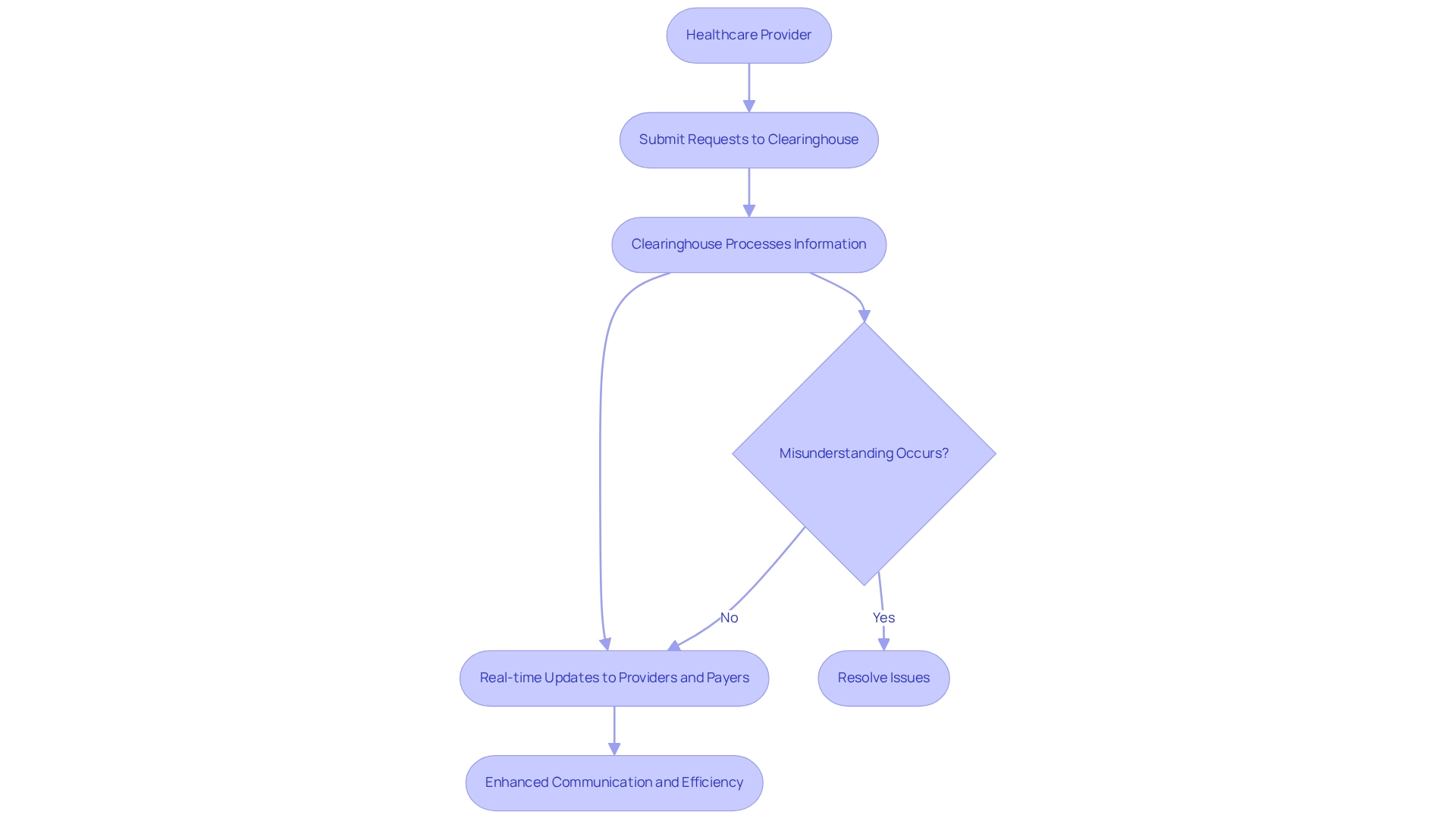
Seamless Communication: Enhancing Provider-Payer Interactions through Clearinghouses
Clearinghouses serve as a vital communication link between healthcare providers and payers, acting as a centralized hub for the submission of requests. By streamlining the exchange of information, they guarantee that both parties have immediate access to crucial data necessary for efficient processing. This seamless communication significantly reduces misunderstandings and errors, which are common culprits behind payment delays, and claims clearinghouses enhance operational efficiency by providing real-time updates on claims status. This capability empowers providers to quickly resolve any issues that may arise, thereby fostering transparency and trust in provider-payer relationships. As a result, organizations utilizing these systems often experience improved collaboration and expedited resolutions to claims-related inquiries.
Research indicates that medical organizations engaged in systematic benchmarking, including the use of intermediary services, achieve notably higher operating margins—up to 18% greater than their non-benchmarking counterparts. This highlights the critical role of effective communication strategies in optimizing revenue cycle performance.
Additionally, data sourced from intermediaries can help identify denial trends and their underlying causes, enabling proactive measures to mitigate denials and enhance overall efficiency in processing requests.
Future Trends: Evolving Role of Claims Clearinghouses in Healthcare
As the medical landscape continues to evolve, claims processing centers are anticipated to play an increasingly crucial role in streamlining operations and improving efficiency. With the growth of telehealth and digital health solutions, clearinghouses must adapt to new technologies and workflows to meet the demands of contemporary medical services. CareSet’s extensive Medicare data solutions, which include insights from over 62 million beneficiaries and 6 million practitioners, empower stakeholders in the medical field to navigate these changes effectively. Notably, the telehealth market size in China reached $1.8 billion in 2020, with an anticipated compound annual growth rate (CAGR) of 30% from 2021 to 2026, underscoring the substantial growth potential in this field.
Future trends may involve the incorporation of artificial intelligence and machine learning to further streamline processing and enhance precision. As noted by Helen Zhuravel, Director of Product Solutions, her extensive experience in product management across various industries underscores the importance of adapting to these technological advancements. Furthermore, as medical practitioners aim to improve patient involvement, data repositories will likely concentrate on offering more thorough information insights that enable providers to make knowledgeable choices regarding patient care. For instance, the expansion of telepsychiatry services presents a significant opportunity for claims clearinghouses to support improved access to mental health care, while CareSet’s data solutions can guide strategies for the entire lifecycle of pharmaceuticals. This evolution will ensure that claims clearinghouses remain essential partners in the healthcare ecosystem, particularly as the insurance industry increasingly adopts automation and data-driven efficiency through AI.

Conclusion
The integration of claims clearinghouses into the healthcare ecosystem has proven transformative, enhancing operational efficiency, accuracy, and patient satisfaction. By automating the claims submission process, these intermediaries allow healthcare providers to prioritize patient care over administrative tasks, streamlining workflows and significantly reducing errors. The enhanced accuracy achieved through automated claim scrubbing minimizes costly denials and accelerates reimbursement cycles, leading to improved cash flow for healthcare organizations.
Moreover, clearinghouses facilitate seamless communication between providers and payers, fostering transparency and building trust—an essential foundation for effective collaboration. As stakeholders increasingly leverage the valuable data insights offered by claims clearinghouses, they can make informed decisions that enhance patient engagement and optimize resource allocation. The presented case studies highlight substantial operational improvements and financial efficiencies, reinforcing the critical role these entities play in the modern healthcare landscape.
Looking ahead, the evolving role of claims clearinghouses will be instrumental as the healthcare industry adapts to new technologies and trends, such as telehealth and artificial intelligence. By continuing to innovate and provide comprehensive data solutions, clearinghouses will support healthcare providers in navigating the complexities of claims processing while contributing to better patient outcomes and sustainable financial models. Embracing these advancements is essential for healthcare organizations aiming to thrive in a rapidly changing environment, ensuring they remain equipped to meet the demands of both patients and the broader healthcare system.


