Overview
The article presents four proven strategies designed to enhance health care outcomes:
- Patient-centered care
- Evidence-based practices
- Continuous monitoring
- Technology integration
These strategies are underpinned by substantial data and research, illustrating that prioritizing patient needs and leveraging robust analytics can lead to significant improvements in treatment adherence and overall health care quality. By focusing on these approaches, health care providers can not only meet but exceed patient expectations, ultimately fostering better health outcomes.
Introduction
In the rapidly evolving landscape of healthcare, the integration of data analytics is fundamentally transforming how organizations approach patient care and outcomes. With a wealth of information at their fingertips, healthcare providers can uncover critical insights into patient demographics, treatment trends, and operational efficiencies.
As organizations strive to enhance care quality and patient satisfaction, implementing proven strategies—such as:
- Patient-centered care
- Evidence-based practices
- Robust collaboration among stakeholders
becomes paramount. Furthermore, navigating the complexities of regulatory and reimbursement challenges necessitates agility and a proactive mindset. This article delves into the essential components of leveraging data and implementing effective strategies to foster improved health outcomes in today’s healthcare environment.
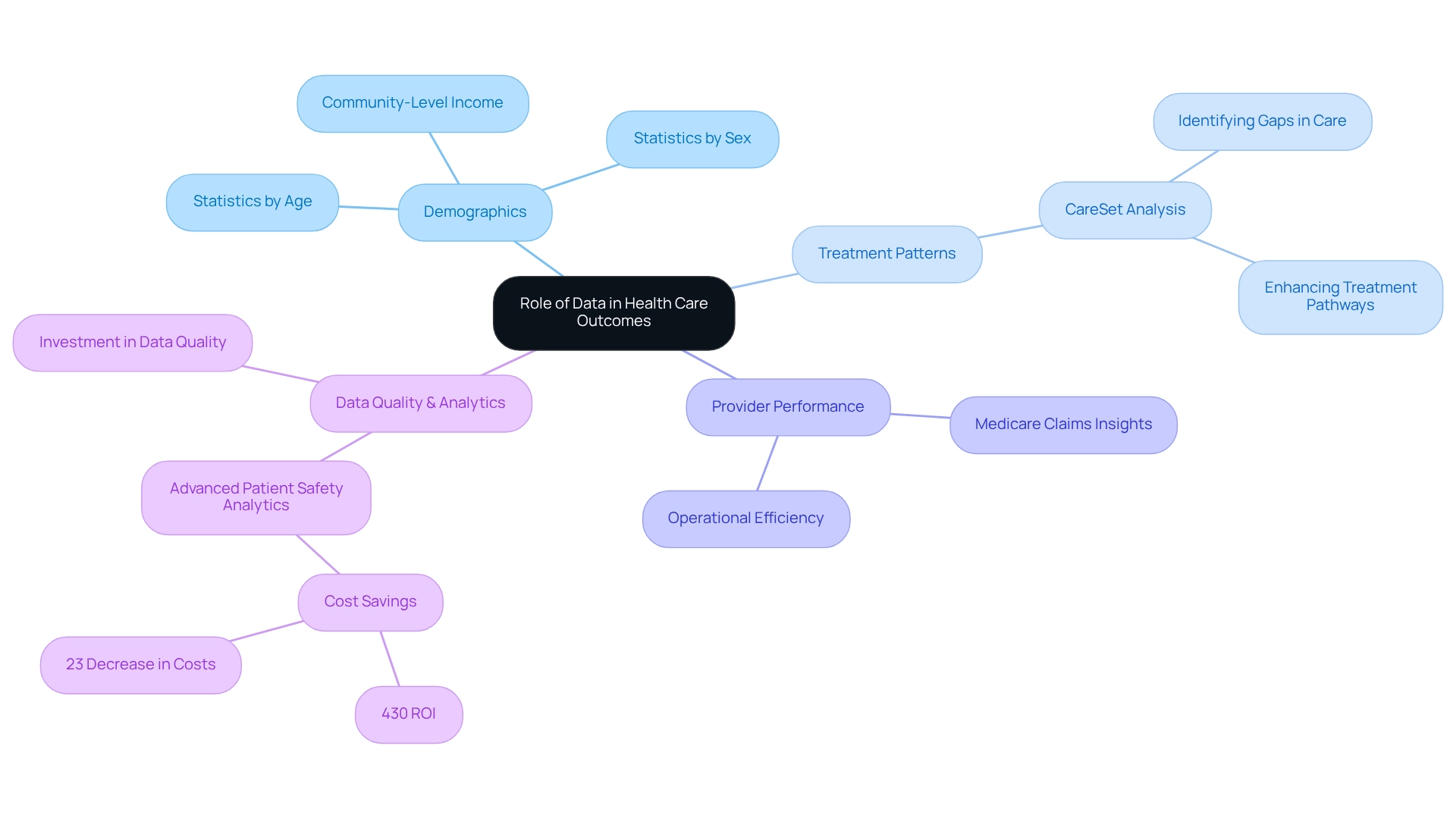
Understand the Role of Data in Health Care Outcomes
Data plays a pivotal role in shaping health care outcomes by offering critical insights into individual demographics, treatment patterns, and provider performance. By leveraging Medicare claims information, healthcare organizations can uncover trends in prescribing habits and patient experiences.
For example, CareSet’s analysis of over $1.1 trillion in annual claims data empowers stakeholders to identify gaps in care and effectively enhance treatment pathways. This robust analytical approach not only improves operational efficiency but also cultivates a culture of evidence-based practice, resulting in superior health care outcomes for patients.
Organizations committed to investing in data quality and analytics capabilities are better positioned to extract actionable insights from their data, ultimately driving improved health care outcomes.
Implement Proven Strategies for Improving Patient Care
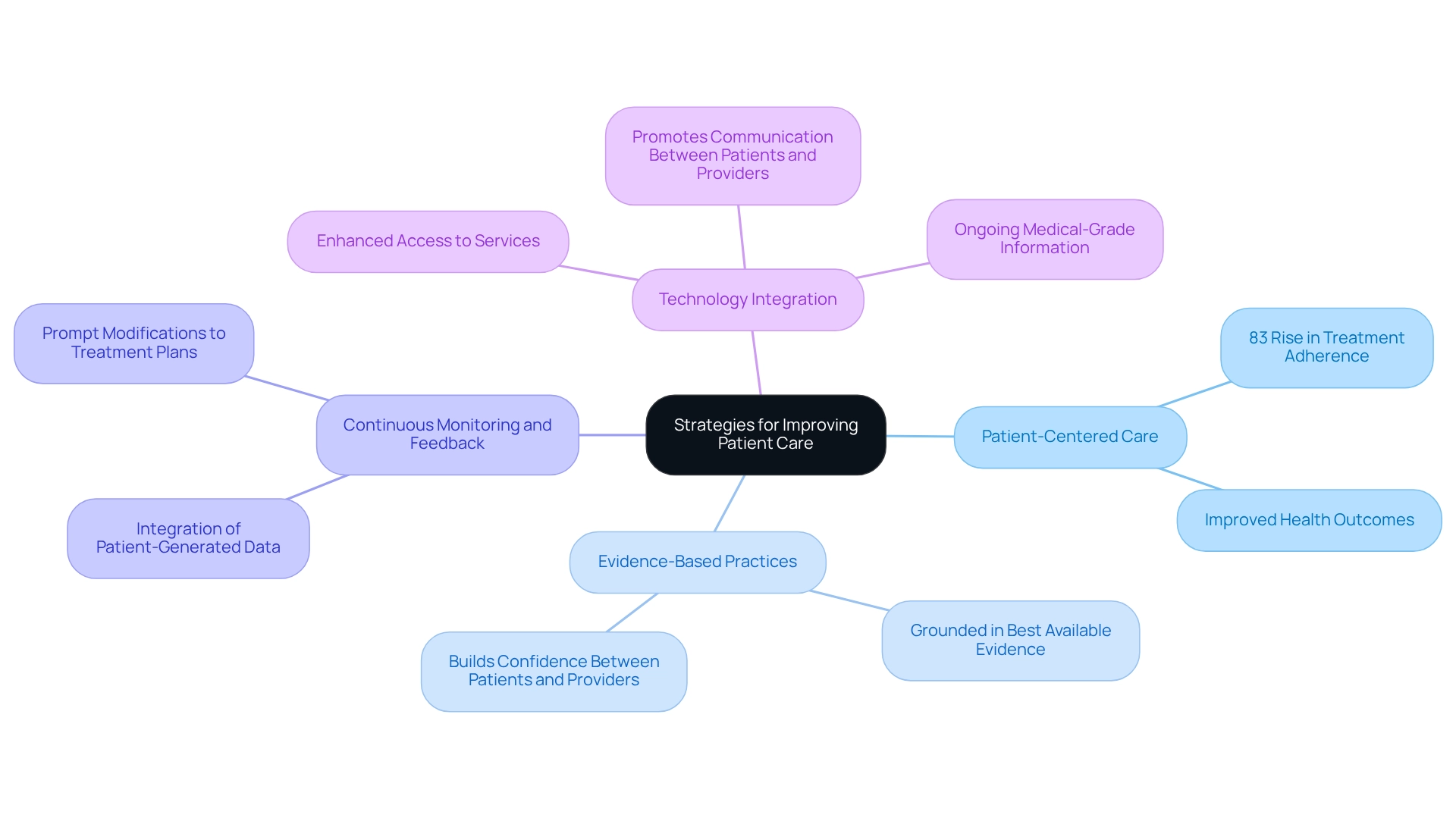
To enhance the quality of treatment, healthcare organizations must implement several established strategies:
-
Patient-Centered Care: Prioritizing the individual needs and preferences of patients is crucial for improving satisfaction and adherence to treatment plans. A report in the Annals of Behavioral Medicine emphasized that patient-focused treatment systems can lead to an impressive 83% rise in treatment adherence, ultimately resulting in improved health outcomes.
-
Evidence-Based Practices: Utilizing clinical guidelines and research findings to inform treatment decisions ensures that services are grounded in the best available evidence. This method not only improves the standard of service but also builds confidence between individuals receiving treatment and their providers.
-
Continuous Monitoring and Feedback: Establishing systems for constant evaluation of individual outcomes and satisfaction enables prompt modifications to treatment plans. Ceci Connolly observed an increasing willingness among doctors to integrate patient-generated data, which can greatly enhance the feedback loop and improve service delivery.
-
Technology Integration: Utilizing digital health resources, such as telemedicine and health portals, enhances access to services and promotes communication between individuals and providers. As new technologies arise, there is optimism for ongoing medical-grade information that can further boost patient involvement and results, as mentioned by industry leaders.
By methodically implementing these strategies, organizations can significantly enhance health care outcomes and patient experiences, ensuring that treatment is not only efficient but also aligned with the evolving needs of patients in 2025 and beyond.
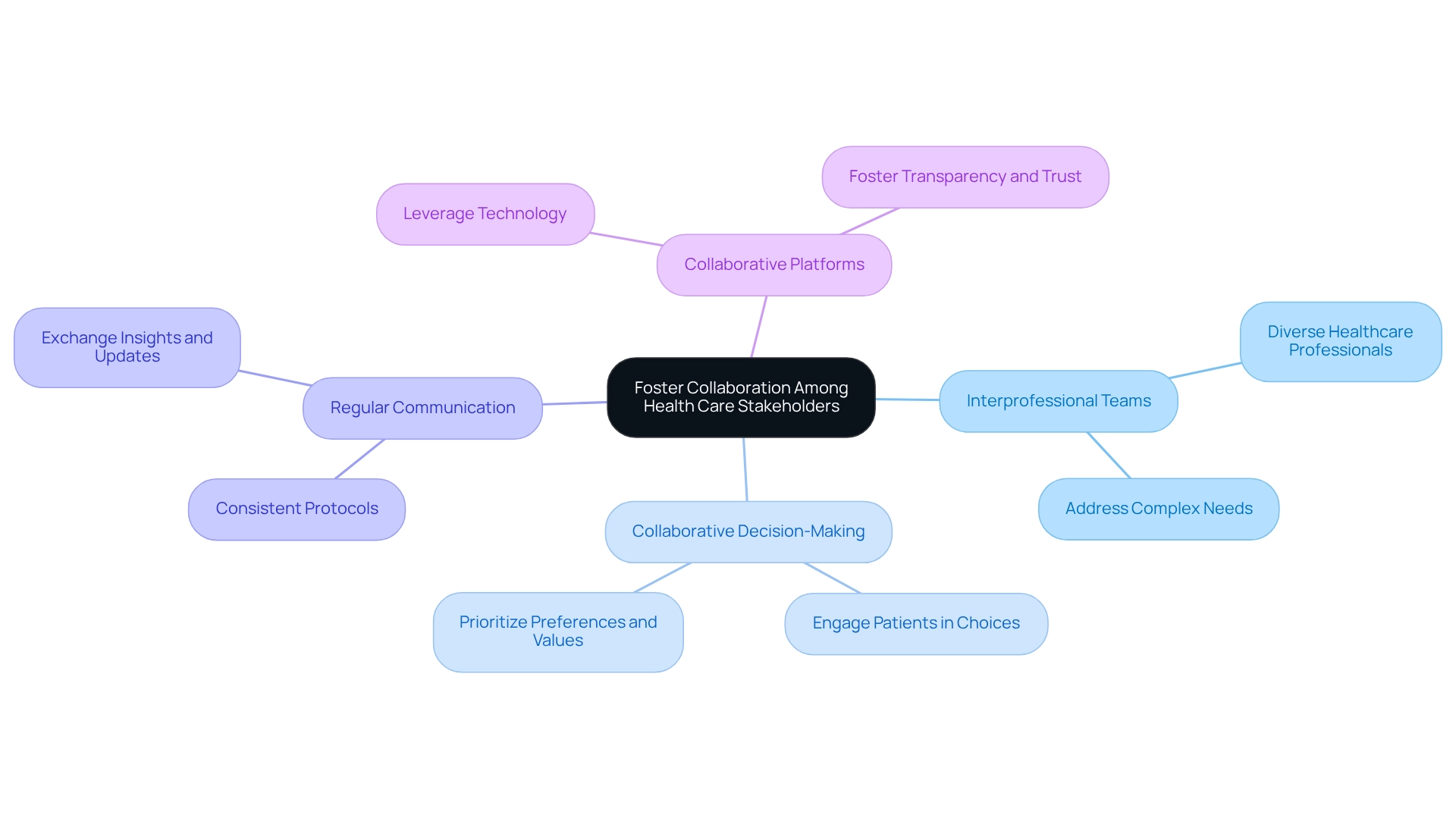
Foster Collaboration Among Health Care Stakeholders
Encouraging cooperation among medical stakeholders—providers, payers, and patients—is essential for improving health outcomes. Effective communication and common goals greatly enhance the coordination of services and reduce fragmentation. Key strategies to bolster collaboration include:
- Interprofessional Teams: Form diverse groups of healthcare professionals to comprehensively address complex individual needs.
- Collaborative Decision-Making: Actively engage individuals in their treatment choices, ensuring their preferences and values are prioritized.
- Regular Communication: Implement protocols for consistent communication among stakeholders to exchange insights and updates on patient care.
- Collaborative Platforms: Leverage technology to establish platforms for information sharing and collaboration, fostering transparency and trust among stakeholders.
CareSet combines over 100 external information sources for its analysis, underscoring the significance of evidence-based collaboration in the medical field. This integration is exemplified in a case study titled “Putting Patients First: Unlocking Medicare Data to Empower HCP,” which showcases how CareSet enhances provider engagement through timely and meaningful interactions regarding treatment options like Qinlock for rare conditions. Furthermore, CareSet’s role in sharing COVID-19 hospital capacity information, as emphasized in the FAQs, has improved community awareness and involvement, further promoting the necessity for cooperation among medical stakeholders. By prioritizing these collaborative efforts, medical organizations can cultivate a more integrated approach to patient care, ultimately leading to improved health outcomes.
Adapt to Evolving Regulatory and Reimbursement Challenges
Healthcare organizations must remain agile in response to evolving regulatory and reimbursement challenges. Key strategies include:
- Stay Informed: Regularly monitor changes in medical regulations and reimbursement policies to ensure compliance and adapt practices accordingly. This proactive approach is essential as the landscape continues to shift in 2025.
- Training and Education: Ongoing training for staff on regulatory requirements and best practices for documentation and coding is crucial. This not only minimizes errors but also optimizes reimbursement, significantly impacting overall health care outcomes.
- Leverage Technology: Implementing advanced analytics and reporting tools can streamline compliance processes and enhance visibility into reimbursement trends. Such technology is vital for organizations aiming to improve operational efficiency and reduce costs.
- Engage with Payers: Building strong relationships with payers is essential to understanding their requirements and negotiating favorable reimbursement terms. By proactively addressing these challenges, organizations can enhance their operational resilience and thereby improve health care outcomes while continuing to deliver high-quality patient care.

Conclusion
The integration of data analytics is revolutionizing healthcare by delivering critical insights into patient demographics and treatment patterns. By harnessing resources such as Medicare claims data, organizations can pinpoint care gaps and refine treatment pathways, ultimately enhancing patient outcomes.
To elevate patient care, healthcare providers must implement strategies that prioritize patient-centered care, embrace evidence-based practices, and ensure continuous monitoring. Focusing on the unique needs of each patient while utilizing clinical guidelines fosters trust and engagement, ensuring that care is grounded in the most reliable evidence available. Additionally, technology significantly enhances communication and access to care, further supporting these efforts.
Collaboration among healthcare stakeholders—including providers, payers, and patients—is paramount for effective care coordination. Establishing interprofessional teams, encouraging shared decision-making, and maintaining consistent communication can mitigate fragmentation and yield improved health outcomes. The integration of diverse data sources further strengthens this collaborative framework.
Lastly, adaptability to evolving regulatory and reimbursement landscapes is essential for sustaining operational resilience. Staying abreast of regulations, investing in staff training, and leveraging technology can streamline compliance and enhance reimbursement processes.
In summary, leveraging data analytics, implementing established care strategies, fostering collaboration, and adapting to regulatory challenges are critical for optimizing health outcomes. By embracing these elements, healthcare organizations are empowered to deliver high-quality care and significantly enhance patient satisfaction.


