Overview
The article focuses on various quality improvement examples in healthcare that aim to enhance patient outcomes and operational efficiencies. It highlights initiatives from organizations like CareSet and the Institute for Healthcare Improvement, demonstrating how data analysis, structured frameworks, and patient-centered approaches lead to measurable improvements in healthcare delivery and patient satisfaction.
By showcasing these initiatives, the article underscores the critical role of data-driven insights in transforming healthcare practices and improving patient experiences. This compelling narrative invites readers to explore further insights from CareSet, fostering a deeper understanding of the impact of quality improvements in the healthcare sector.
Introduction
In the dynamic landscape of healthcare, the pursuit of quality improvement has never been more critical. Leveraging comprehensive Medicare data and implementing structured improvement models, various organizations are making significant strides to enhance patient care and operational efficiency. This article explores the innovative strategies employed by leading institutions, including:
- CareSet
- The Institute for Healthcare Improvement
- The American Public Health Association
By examining their methodologies, successes, and challenges, readers will gain insight into how these efforts collectively contribute to better health outcomes and a more effective healthcare delivery system. As the industry evolves, understanding these quality improvement initiatives becomes essential for stakeholders aiming to navigate the complexities of modern healthcare.
CareSet: Transforming Healthcare Quality with Comprehensive Medicare Data Insights
CareSet leverages its extensive Medicare claims data to deliver actionable insights that significantly enhance the standard of care. By analyzing over $1.1 trillion in annual claims, the company uncovers critical treatment patterns, identifies gaps in care, and evaluates provider networks. This data-driven methodology empowers healthcare organizations to make informed decisions that lead to improved outcomes for individuals and operational efficiencies.
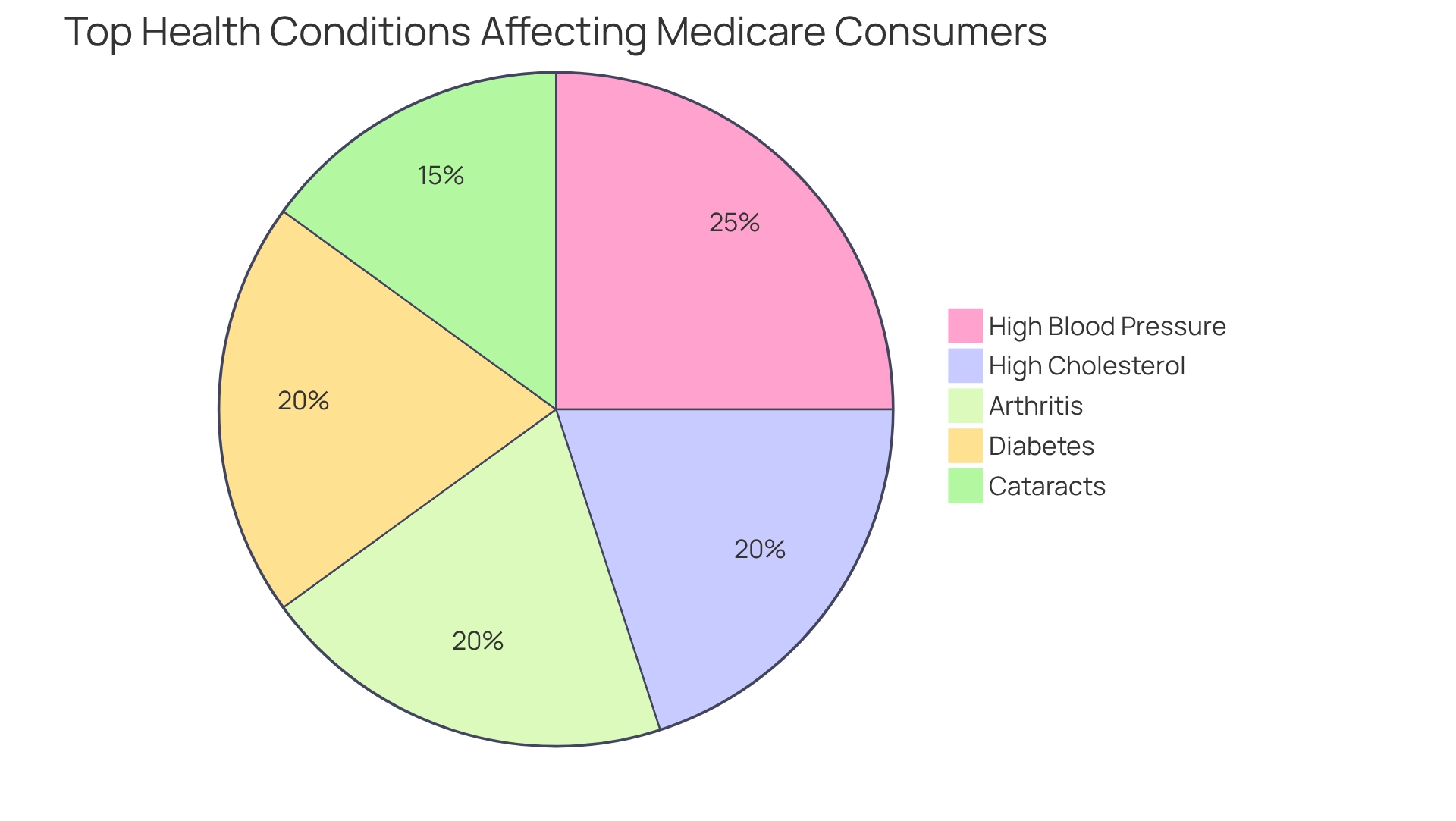
For instance, through meticulous mapping of individual journeys, CareSet enables stakeholders to grasp the complexities of care, thereby fostering quality improvement examples in healthcare initiatives. As we approach 2025, the influence of Medicare claims data on patient outcomes becomes increasingly apparent. Statistics reveal that the top five health conditions affecting Medicare consumers are:
- High blood pressure
- High cholesterol
- Arthritis
- Cataracts
- Diabetes
By addressing these prevalent conditions through comprehensive data analysis, CareSet enhances medical providers’ ability to tailor interventions effectively. Moreover, CareSet’s commitment to clarity and high-quality insights not only satisfies immediate data needs but also supports long-term strategic development for its partners in the medical sector. This focus on strategic growth is essential for optimizing the lifecycle management of pharmaceutical products, ultimately resulting in improved patient outcomes.
Case studies illustrate how CareSet’s data analysis has elevated medical care, highlighting quality improvement examples in healthcare through successful enhancement initiatives in real-world settings. Expert insights further underscore the importance of precise Medicare claims information in shaping policy decisions and refining health services. As the landscape of Medicare Advantage enrollment grows increasingly complex, the demand for accurate data to inform these initiatives is more critical than ever.
Institute for Healthcare Improvement: Implementing the Model for Improvement in Healthcare
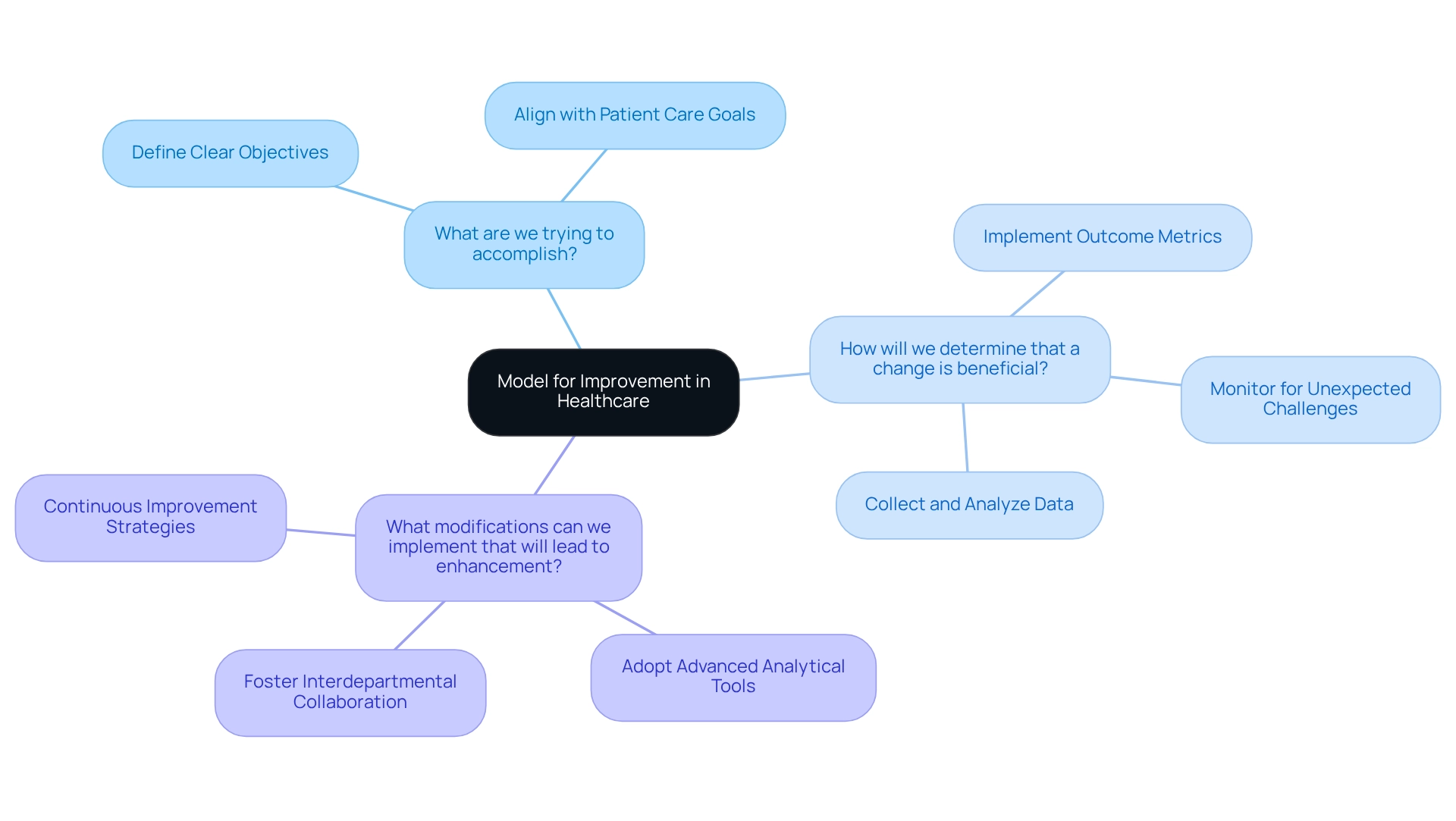
The Institute for Healthcare Improvement (IHI) champions the Model for Improvement, a strategic framework engineered to elevate healthcare quality through structured inquiry. This model is anchored by three essential questions:
- What are we trying to accomplish?
- How will we determine that a change is beneficial?
- What modifications can we implement that will lead to enhancement?
By addressing these inquiries, medical teams can delineate clear objectives, effectively measure outcomes, and systematically implement changes.
Embracing the Model for Improvement fosters a culture of continuous enhancement within healthcare organizations, ultimately driving improved care and operational efficiency. Current adoption rates indicate a growing recognition of this model’s value, with numerous organizations incorporating it into their quality improvement examples in healthcare initiatives. For instance, medical teams utilizing this model have reported significant advancements in patient outcomes, showcasing quality improvement examples in healthcare that demonstrate its efficacy in real-world applications.
Looking ahead to 2025, ongoing enhancement strategies are expected to evolve further, emphasizing the use of advanced analytical tools to drive innovation in medical service delivery. Case studies illustrate that organizations committed to the Model for Improvement have not only bolstered their analytical capabilities but also nurtured collaboration across departments, which serve as quality improvement examples in healthcare, resulting in more effective healthcare solutions.
As Amar Shah, a distinguished expert in standard enhancement, emphasizes, any advancement endeavor should incorporate outcome metrics that are directly linked to the initiative’s goals. This alignment ensures that changes are impactful and contribute to the overarching objective of enhancing patient care.
BMC Health Services Research: Leveraging Benchmarking for Quality Improvement in Healthcare
BMC Health Services Research underscores the critical importance of benchmarking as a key among the quality improvement examples in healthcare that drive enhancements within the medical field. By systematically comparing performance metrics against established industry standards, healthcare organizations can identify service delivery gaps and implement targeted interventions. For instance, hospitals can benchmark their readmission rates and satisfaction scores, gaining valuable insights into their performance relative to peers. This data-driven approach, supported by CareSet’s integration of over 100 external data sources, not only fosters accountability but also encourages organizations to adopt best practices that significantly enhance care quality.
Moreover, effective benchmarking has been linked to improved outcomes for patients, as evidenced by case studies that highlight the significance of medication reconciliation. Implementing robust medication reconciliation practices prior to discharge has been proven to reduce medication-related readmissions, which are among the quality improvement examples in healthcare that showcase tangible benefits. A notable example is CareSet’s case study titled “PUTTING PATIENTS FIRST: Unlocking Medicare Data to Empower HCP,” which illustrates how leveraging Medicare data can empower medical providers to engage more effectively with physicians on treatment options such as Qinlock for Gastrointestinal Stromal Tumor (GIST).
As the medical field continues to evolve, the utilization of benchmarking and comprehensive Medicare data insights will remain essential for organizations aiming to enhance care delivery and achieve outstanding results for patients, ultimately fostering long-term strategic growth.

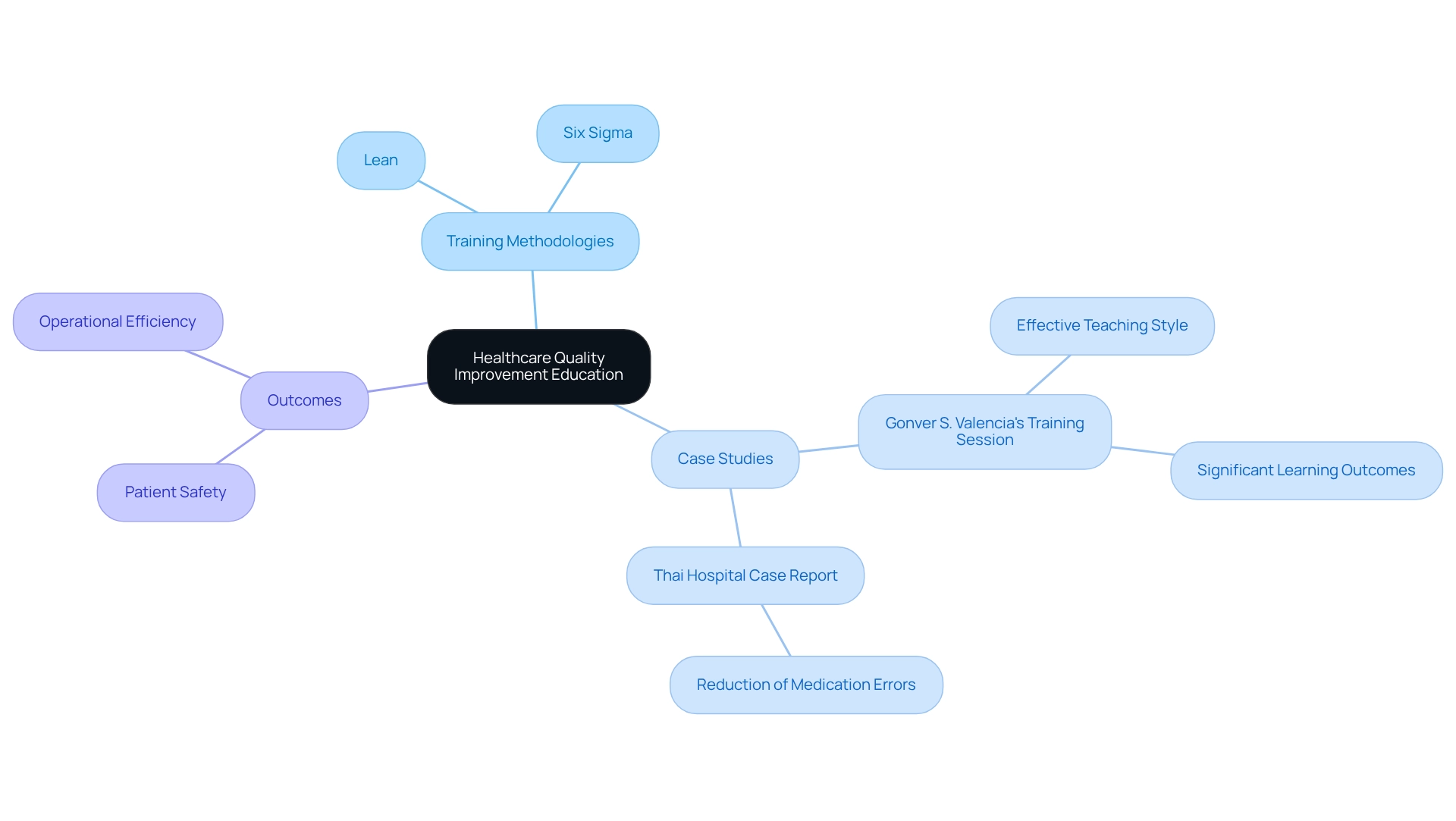
Harvard School of Public Health: Educating Leaders in Healthcare Quality Improvement
The Harvard School of Public Health stands at the forefront of training future leaders dedicated to enhancing health services. This institution emphasizes the integration of evidence-based methods and strategic decision-making to improve health delivery. Their programs showcase quality improvement examples in healthcare, including methodologies such as Lean and Six Sigma, which have been pivotal in the medical field since their introduction in 1986. These approaches equip professionals with the essential skills needed to spearhead initiatives that significantly improve patient outcomes and operational efficiency.
A case study by Gonver S. Valencia exemplifies this, detailing an effective training session that yielded substantial learning in a condensed timeframe, facilitated by an engaging teaching style. Graduates emerge prepared to confront complex challenges within the medical sector, fostering a culture of excellence and safety that is vital for advancing health standards.
As highlighted by Mohd. Shadab, ‘An exhaustive systematic literature review was conducted for the present study,’ emphasizing the robust research underpinning these educational programs. Furthermore, quality improvement examples in healthcare, including Lean Six Sigma methodologies, have proven instrumental in reducing medication errors, as evidenced by a case report from a Thai hospital, which further demonstrates the profound impact of these training programs on patient safety and operational efficiency.
Catalyst by NEJM: Enhancing Quality Through Effective Risk Management Strategies
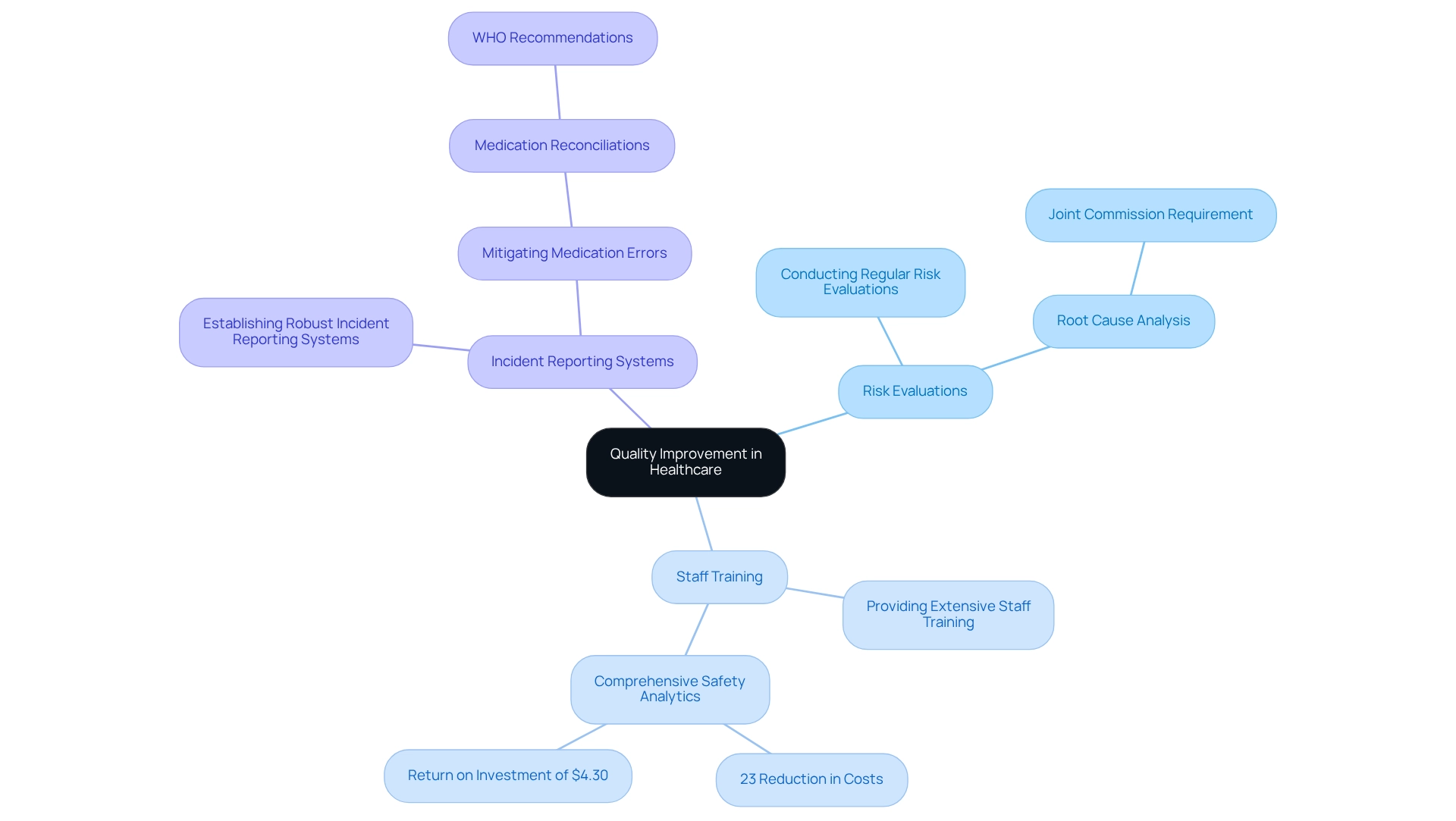
Catalyst by NEJM underscores the crucial role of effective risk management strategies as quality improvement examples in healthcare to elevate the quality of medical care. By proactively identifying potential risks and implementing preventive measures, medical organizations can significantly diminish the occurrence of adverse events, serving as quality improvement examples in healthcare. Key strategies for quality improvement examples in healthcare include:
- Conducting regular risk evaluations
- Providing extensive staff training
- Establishing robust incident reporting systems
All of which are essential for nurturing a culture of safety. For instance, quality improvement examples in healthcare have shown that medical systems integrating comprehensive safety analytics programs reported an impressive 23% reduction in costs associated with avoidable adverse events. This translates to a return of $4.30 for every dollar invested in advanced safety analytics for patients, emphasizing the financial and clinical advantages of such initiatives.
Furthermore, the Joint Commission mandates that medical institutions conduct a root cause analysis following all sentinel events, reinforcing the imperative of thorough risk management practices. As highlighted in the ‘Top 10 Safety Concerns 2025’ report, a strategic approach to addressing safety issues is vital for implementing quality improvement examples in healthcare, particularly given the increasing complexity of medical service delivery. Additionally, the WHO publication suggests that medication reconciliations in primary care settings, supported by effective communication between healthcare providers and patients, can significantly mitigate the risk of medication-related adverse events. Hospitals that have successfully implemented effective risk management frameworks often experience a marked decrease in medication errors, thereby enhancing safety for patients. By prioritizing these strategies, medical organizations can not only improve their operational efficiency but also foster an environment where patient safety is paramount.
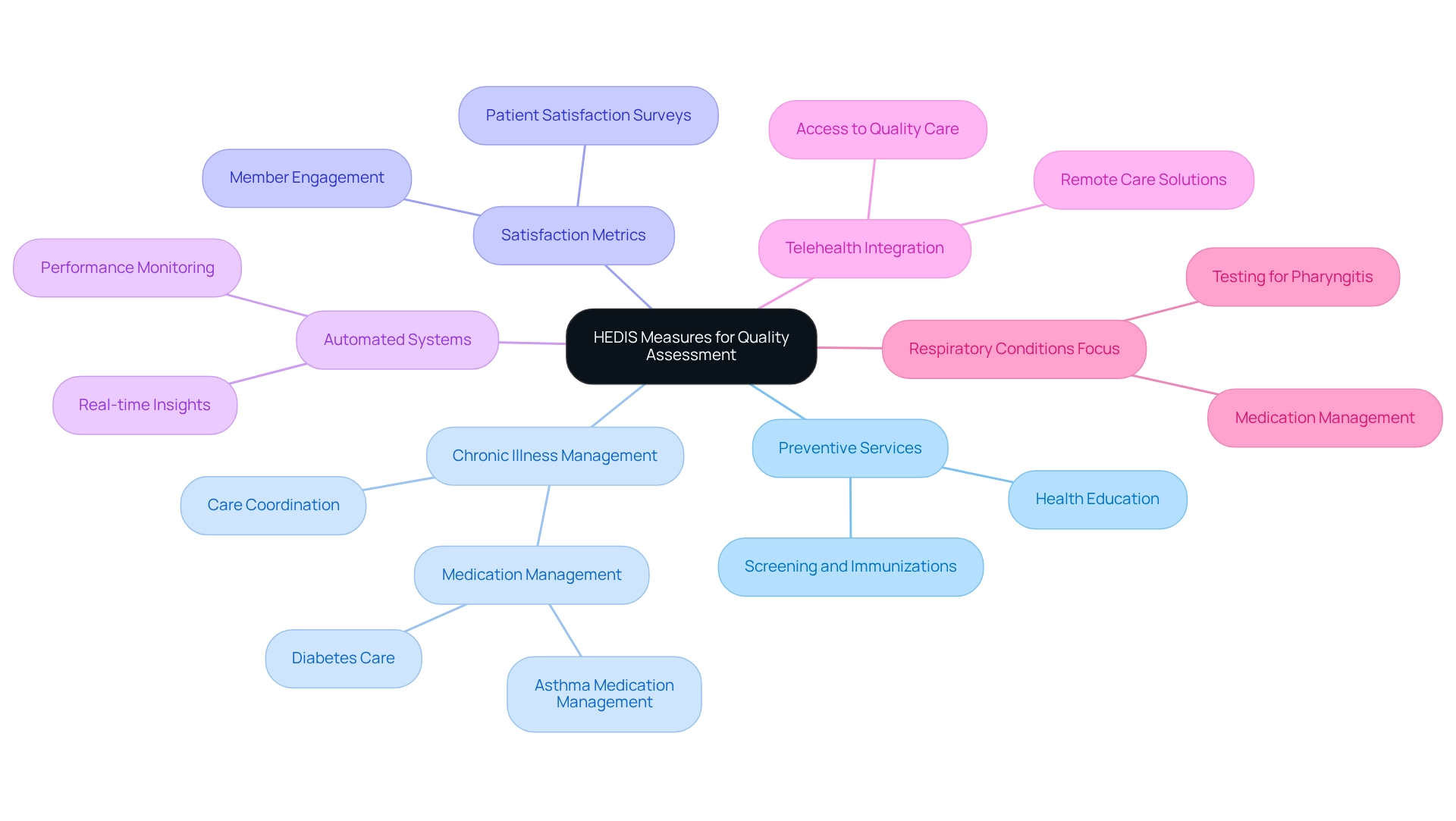
National Committee for Quality Assurance: Utilizing HEDIS Measures for Quality Assessment
The National Committee for Quality Assurance (NCQA) utilizes the Healthcare Effectiveness Data and Information Set (HEDIS) as an essential instrument for assessing the quality of care provided by health plans. HEDIS encompasses a wide range of medical dimensions, including preventive services, chronic illness management, and satisfaction metrics. By thoroughly analyzing HEDIS data, medical organizations can identify specific areas in need of quality improvement examples in healthcare and develop targeted interventions to bridge these gaps. The incorporation of automated systems has transformed this process, facilitating real-time insights that enable organizations to effectively monitor performance against key metrics. This capability not only improves operational efficiency but also enhances member engagement and satisfaction.
Furthermore, the COVID-19 pandemic has highlighted the significance of telehealth in advancing HEDIS performance. Health plans that successfully integrated remote care solutions have expanded access to high-quality care, demonstrating the potential of digital health initiatives in managing chronic diseases. As of 2025, current HEDIS measures statistics reveal an increasing focus on respiratory conditions, which highlights the necessity for appropriate testing and medication management, serving as quality improvement examples in healthcare. By strategically leveraging HEDIS data, healthcare organizations can implement improvement initiatives that yield better health outcomes, ultimately contributing to a more effective healthcare delivery system.
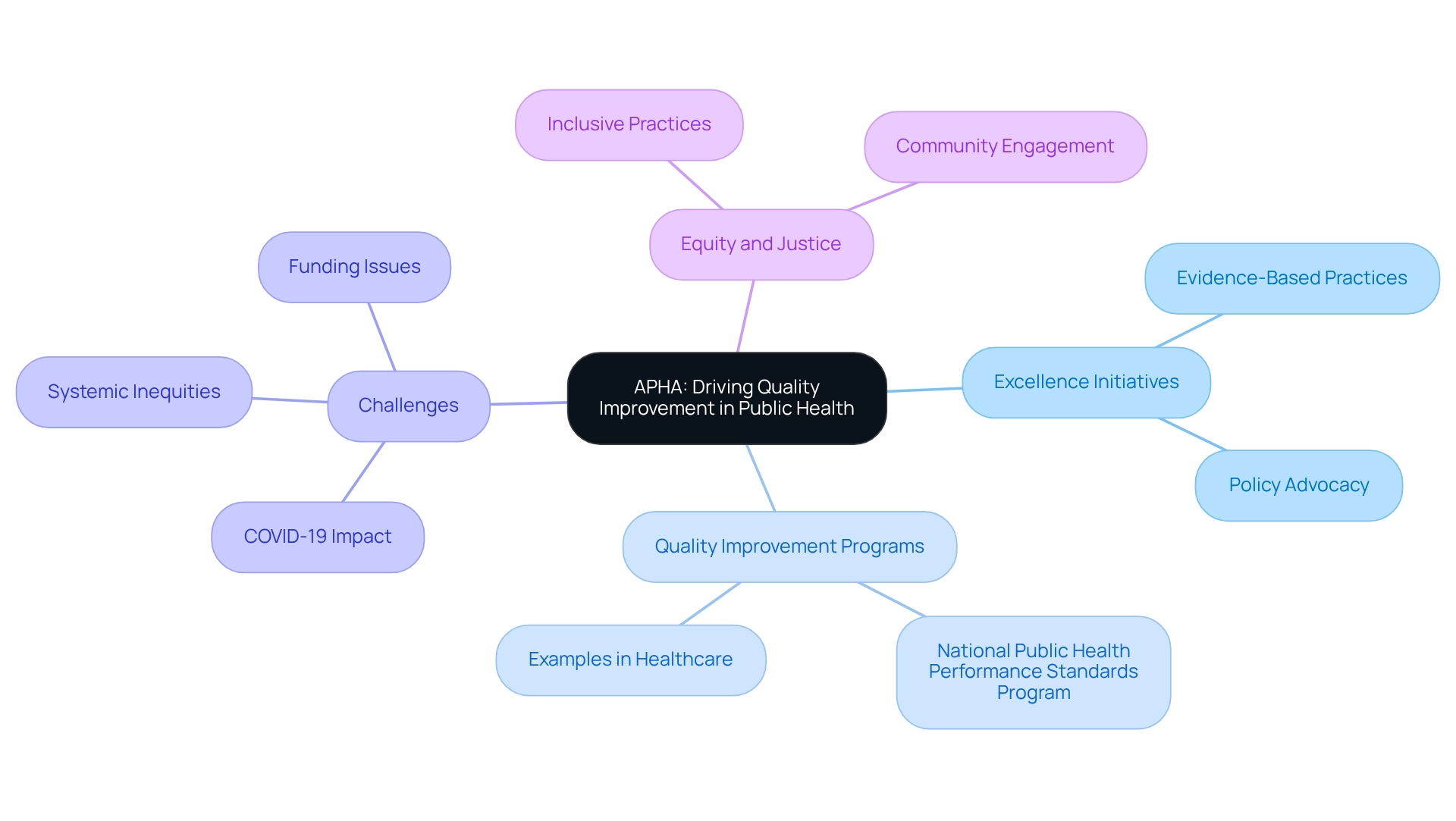
American Public Health Association: Driving Quality Improvement in Public Health
The American Public Health Association (APHA) plays a pivotal role in advancing excellence initiatives within public health. By championing evidence-based practices and advocating for essential policy changes, APHA significantly enhances the standard of public health services. Programs such as the National Public Health Performance Standards Program are designed to evaluate and improve the effectiveness of public health systems.
Through strategic collaboration with local health departments, APHA fosters a culture of continuous improvement by implementing quality improvement examples in healthcare that ultimately benefits community health outcomes. Recent challenges, notably the COVID-19 pandemic, have underscored the urgent need to address systemic inequities, inadequate funding, and leadership deficiencies in public health.
As highlighted in the case study ‘Pandemics Exposing Systemic Inequities,’ these challenges expose critical weaknesses in public health systems, reinforcing the importance of APHA’s initiatives. Furthermore, as Jannat Saini aptly stated, ‘This whole conversation starts and ends with equity and justice,’ emphasizing the necessity of inclusive practices that serve all community members.
Through these comprehensive efforts, APHA not only tackles immediate public health challenges but also establishes a foundation that includes quality improvement examples in healthcare for sustainable improvements in community health.
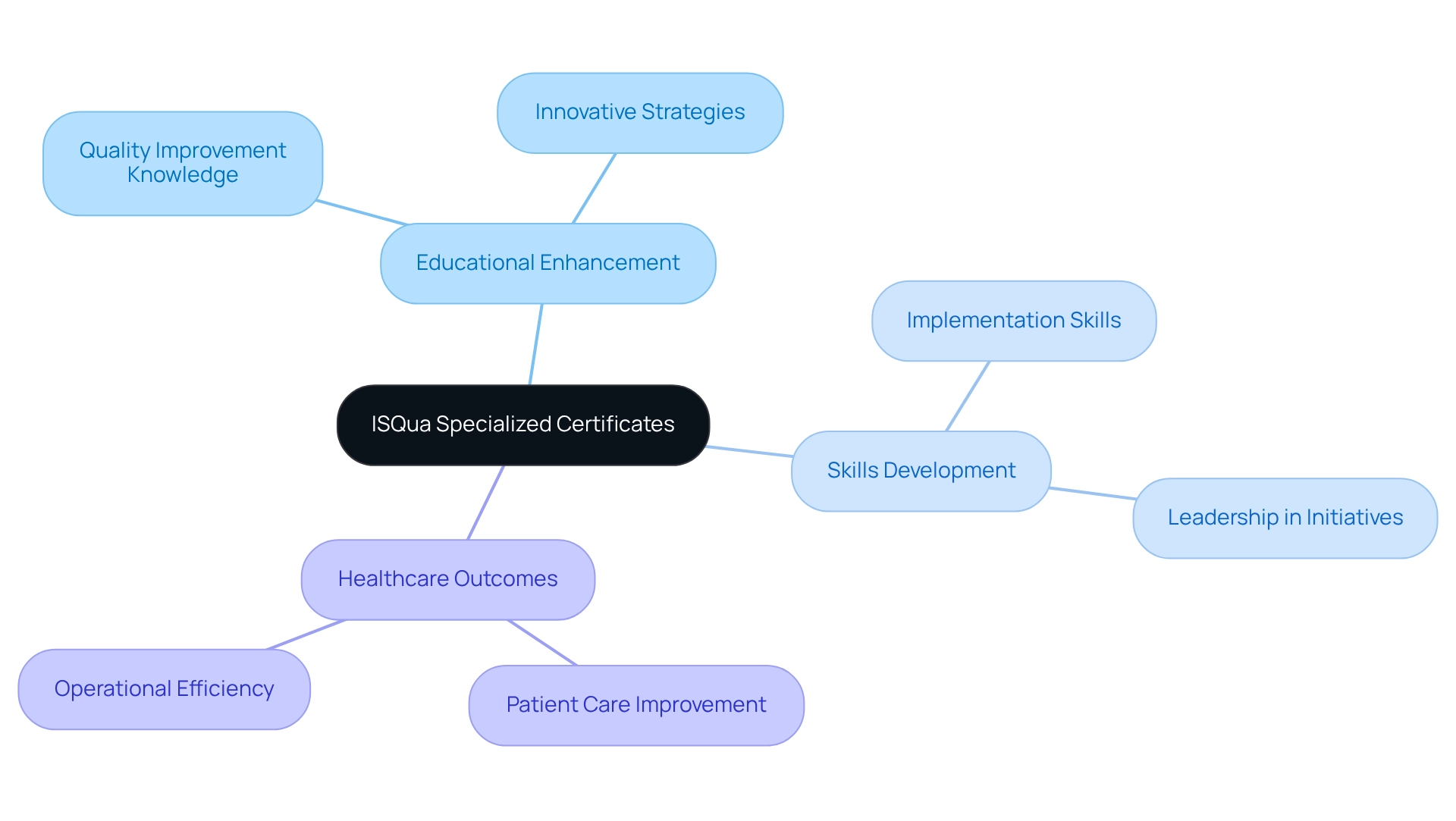
ISQua: Advancing Quality Improvement Education Through Specialist Certificates
The International Society for Excellence in Health Care (ISQua) offers specialized certificates designed to enhance education in standards advancement. These programs equip medical professionals with the essential knowledge and skills needed to implement effective quality improvement examples in healthcare initiatives. By focusing on optimal methods and innovative strategies, ISQua prepares participants to lead initiatives that serve as quality improvement examples in healthcare, ultimately enhancing patient care and safety.
Graduates of these programs are significantly better equipped to confront the challenges associated with delivering high-quality medical care. Evidence indicates that quality improvement examples in healthcare, particularly ongoing enhancement initiatives, can lead to reduced hospital infection rates and shorter hospital stays, underscoring their enduring impact on medical processes.
With approximately 1.8 million job vacancies projected annually in the medical field from 2022 to 2032, the demand for skilled enhancement experts is more critical than ever. By pursuing ISQua’s specialized certificates, healthcare professionals position themselves to navigate the complexities of providing high-quality care, which ultimately leads to quality improvement examples in healthcare and enhances operational efficiencies within healthcare systems.
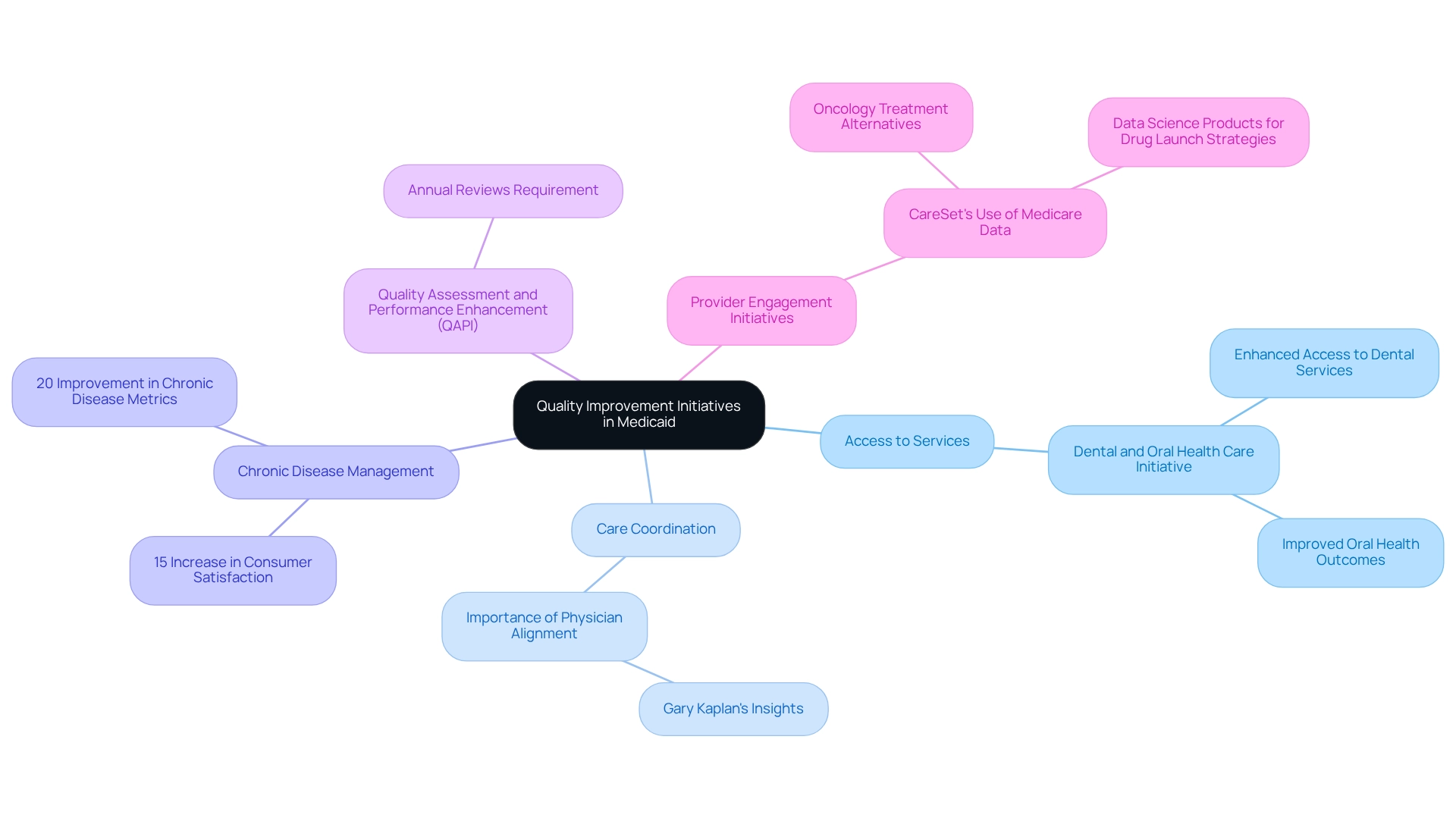
Medicaid.gov: Implementing Quality Improvement Initiatives in Medicaid Programs
Medicaid.gov outlines a range of quality enhancement initiatives aimed at improving care for Medicaid beneficiaries, with a focus on access to services, care coordination, and preventive measures. Notably, many Medicaid programs are implementing projects specifically targeting chronic disease management, ensuring beneficiaries receive timely and effective interventions. For instance, programs such as the Dental and Oral Health Care Initiative have successfully enhanced access to dental services and preventive care, resulting in improved oral health outcomes.
In 2025, states are required to conduct annual evaluations of the effectiveness of each managed care entity’s Quality Assessment and Performance Enhancement (QAPI) program, underscoring the commitment to continuous improvement. Experts emphasize that effective care coordination is essential; as Gary Kaplan, M.D., chairman and CEO of Virginia Mason Health System, noted, alignment among physicians is critical for driving meaningful change.
The impact of Medicaid programs on healthcare access and coordination is significant, particularly for vulnerable populations. Quality improvement examples in healthcare not only enhance health outcomes but also play a crucial role in managing chronic conditions among beneficiaries. Statistics indicate that states implementing these initiatives have reported a 15% increase in consumer satisfaction and a 20% improvement in chronic disease management metrics, which serve as quality improvement examples in healthcare, reinforcing the importance of quality enhancement in Medicaid programs. Simultaneously, CareSet is leading initiatives to enhance provider engagement through the strategic use of Medicare data, particularly in oncology treatment alternatives such as Qinlock for Gastrointestinal Stromal Tumor (GIST). By unlocking valuable insights from Medicare data, CareSet empowers healthcare providers to make informed decisions, ultimately improving health outcomes. Additionally, CareSet Systems has introduced innovative data science products designed to enhance drug launch strategies, equipping pharmaceutical companies with the necessary tools to navigate the complexities of market access effectively.
Overall, the ongoing efforts to refine and enhance Medicaid initiatives, including the mandated annual reviews of QAPI programs, are crucial in fostering better health outcomes and ensuring that beneficiaries receive the comprehensive care they require. These enhancements also provide guidance for pharmaceutical market access strategies, as improved health results can lead to more effective engagement and product positioning.
Permanente Medicine: Achieving Quality Care Through a Patient-Centered Approach
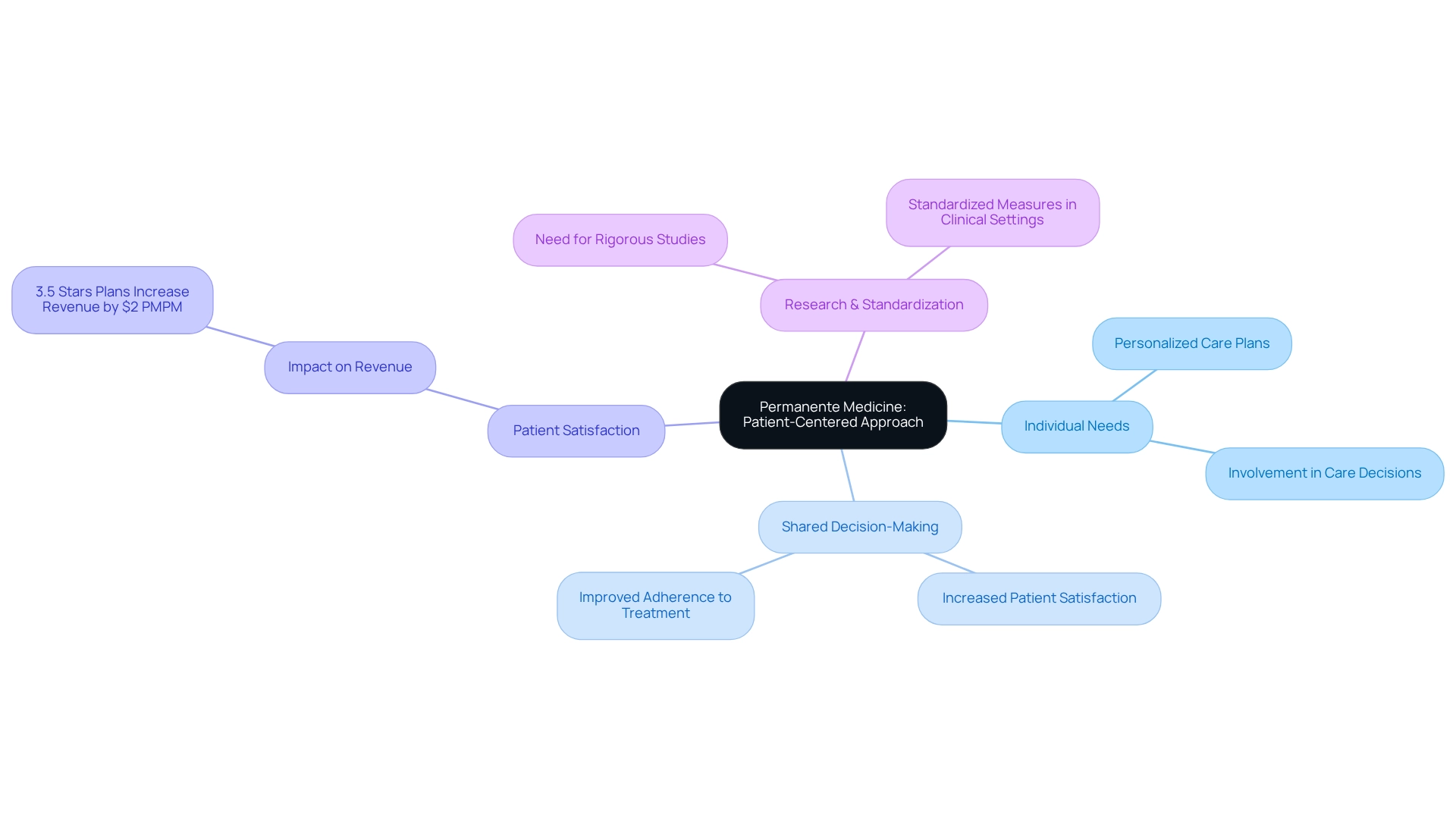
Permanente Medicine exemplifies the critical role of a patient-centered approach in achieving quality care. By prioritizing individual needs and preferences, healthcare providers significantly enhance the overall experience and improve health outcomes. This methodology actively involves individuals in their care decisions, ensuring that treatment plans align with their values and goals.
Notably, the emphasis on shared decision-making and personalized care plans has been linked to increased patient satisfaction and improved adherence to treatment regimens. For instance, statistics indicate that plans with 3.5 stars can boost revenue by an average of $2 PMPM by enhancing just one quality measure.
Furthermore, expert opinions underscore the necessity of rigorous research to validate the benefits of shared decision-making, as highlighted in recent studies calling for standardized measures in clinical settings. The integration of patient-centered care not only fosters better health outcomes but also aligns with the growing advocacy for a more caring and integrated healthcare approach.
Conclusion
The exploration of quality improvement initiatives within healthcare reveals a multifaceted approach essential for enhancing patient outcomes and operational efficiency. Organizations such as CareSet utilize comprehensive Medicare data to identify treatment patterns and gaps in care, enabling targeted interventions that directly address prevalent health conditions. Their commitment to transparency and strategic growth significantly contributes to optimizing healthcare delivery.
Similarly, the Institute for Healthcare Improvement emphasizes the Model for Improvement, promoting a culture of continuous enhancement within healthcare organizations. By fostering collaboration and systematic inquiry, this model has proven effective in driving meaningful changes that elevate patient care. The integration of advanced analytical tools further supports the evolution of these strategies, paving the way for innovative healthcare solutions.
Benchmarking, as highlighted by BMC Health Services Research, serves as a critical tool for healthcare organizations to assess their performance against industry standards. This data-driven approach fosters accountability and motivates the adoption of best practices that enhance patient care. Furthermore, the role of education in quality improvement, as demonstrated by institutions like the Harvard School of Public Health and ISQua, equips future leaders with the necessary skills to tackle complex challenges in healthcare.
Ultimately, the collective efforts of these organizations illustrate that quality improvement is an ongoing journey requiring collaboration, data-driven decision-making, and a steadfast commitment to patient-centered care. As the healthcare landscape continues to evolve, these initiatives will play a vital role in shaping a more effective and equitable healthcare delivery system, ensuring that all patients receive the high-quality care they deserve.


