Overview
The primary advantages of clinical trial EDC systems encompass:
- Enhanced data quality
- Streamlined data collection
- Improved regulatory compliance
- Cost efficiency
These factors collectively contribute to increased efficiency in clinical trials. This article elaborates on these benefits by illustrating how EDC systems:
- Automate data entry processes
- Minimize errors
- Provide real-time access to critical information
- Ensure adherence to industry standards
Such advancements ultimately lead to expedited and more reliable research outcomes.
Introduction
In the rapidly evolving landscape of clinical research, the integration of advanced technologies is fundamentally transforming the design and execution of trials. At the forefront of this transformation is the adoption of Electronic Data Capture (EDC) systems, which not only streamline data collection but also enhance accuracy, ultimately driving improved patient outcomes.
As organizations increasingly acknowledge the critical importance of real-time data access and robust regulatory compliance, EDC systems emerge as essential tools that significantly reduce operational costs while fostering patient engagement and retention.
This article explores the multifaceted advantages of EDC systems, examining their pivotal role in enhancing data quality, accelerating trial timelines, and paving the way for future innovations in clinical trials.
CareSet: Empowering Clinical Trials with Comprehensive Medicare Data Insights
CareSet excels in extracting and interpreting intricate Medicare claims information, a vital component in the success of medical studies. By delivering insights into patient demographics, treatment patterns, and provider networks, CareSet equips stakeholders with essential information for informed decision-making. This data-focused approach not only enhances the design and implementation of clinical trial EDC studies but also aligns them with actual patient requirements and behaviors.
In 2025, the impact of Medicare claims information on clinical trial EDC design is more pronounced than ever. Cutting-edge technologies and strategic assets provided by CareSet—including pioneering analytics solutions like predictive insights and real-time information integration—are anticipated to refine study designs and improve recruitment techniques, ultimately lowering overall research expenses. Healthcare analysts emphasize the importance of understanding patient demographics in study design, as this knowledge significantly influences outcomes and patient engagement.
CareSet’s insights into Medicare information are particularly valuable for research studies involving clinical trial EDC, offering a comprehensive perspective on treatment trends and patient experiences. This is illustrated by the case study of an oncology treatment producer focusing on the 4th line of therapy for GIST. The implementation of predictive analytics frameworks in healthcare organizations has proven effective in identifying health risks and predicting readmission rates, thereby enhancing overall healthcare delivery. This method underscores the necessity of utilizing Medicare information to boost research efficiency and effectiveness within a clinical trial EDC. As Markus Draguns, Director of Nursing, states, “I no longer need to double check that everything has been correctly submitted to Medicare; I can just push a button and forget about it.”
As the landscape of medical studies evolves, CareSet remains at the forefront, ensuring that its clients benefit from timely and relevant insights. By addressing urgent information needs and fostering sustained strategic development, CareSet empowers pharmaceutical firms and healthcare entities to enhance their research processes and improve patient outcomes.
Enhanced Data Quality and Accuracy: The Core Advantage of EDC Systems
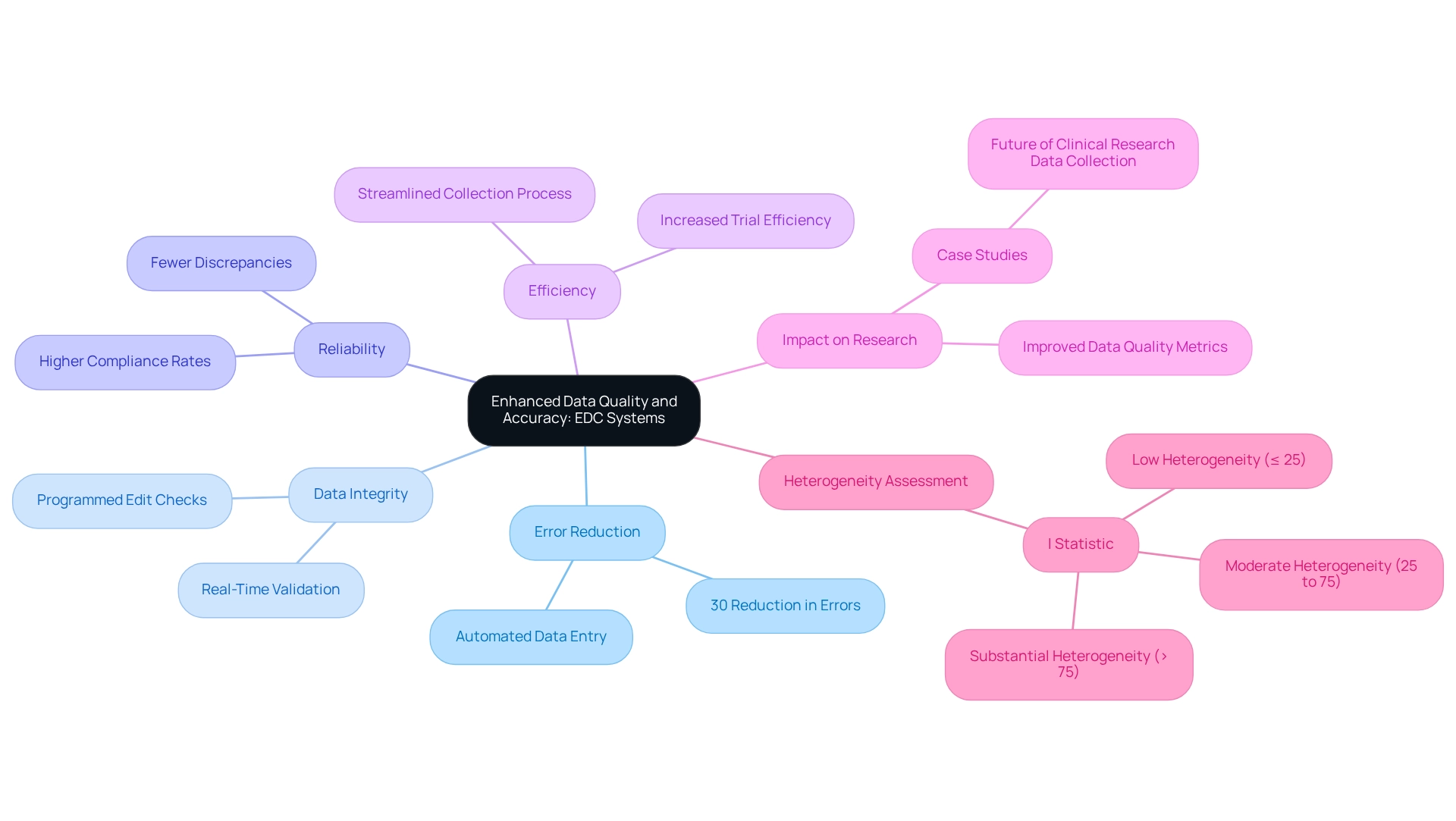
Clinical trial EDC platforms play a pivotal role in enhancing information quality by automating data input and integrating programmed edit checks. These systems significantly reduce human errors, with research indicating a decrease in mistakes by up to 30% in medical trials. By facilitating real-time information validation, EDC systems ensure that the data collected is both accurate and reliable, a fundamental requirement for the integrity of research outcomes.
The benefits of EDC systems extend beyond mere error reduction. They improve data accuracy and reliability, empowering researchers to maintain high standards of information integrity. A recent study highlighted that the shift to web-based EDC has become the predominant method for research data collection, underscoring the growing reliance on these technologies.
Moreover, research managers have noted that automated data entry not only streamlines the collection process but also enhances the overall quality of the information obtained. The implementation of clinical trial EDC systems has demonstrated a significant improvement in data quality metrics, with many organizations reporting increased efficiency in their trials. Case studies further illustrate the effectiveness of clinical trial EDC systems in enhancing data quality. For example, a recent analysis revealed that trials utilizing EDC technologies encountered fewer discrepancies and achieved higher compliance rates, ultimately resulting in more valid trial outcomes.
As the landscape of medical research evolves, the adoption of clinical trial EDC technologies is increasingly recognized as a critical component for achieving favorable results. Additionally, the variability in data quality across different studies can be assessed using the I statistic, indicating low heterogeneity at ≤ 25%, moderate heterogeneity at 25% to 75%, and substantial heterogeneity at > 75%. This context underscores the importance of clinical trial EDC technologies in minimizing discrepancies in data collection.
As Lori A Devlin, DO, MHA, emphasized, the integration of EDC technologies is essential for maintaining the integrity of medical evaluations. Furthermore, the choice of data processing techniques in clinical trial EDC can significantly impact the validity of trial outcomes, reinforcing the crucial role of clinical trial EDC platforms in ensuring accurate and reliable data collection.
In summary, the implementation of clinical trial EDC platforms is increasingly recognized as an indispensable factor in achieving successful outcomes in medical research.
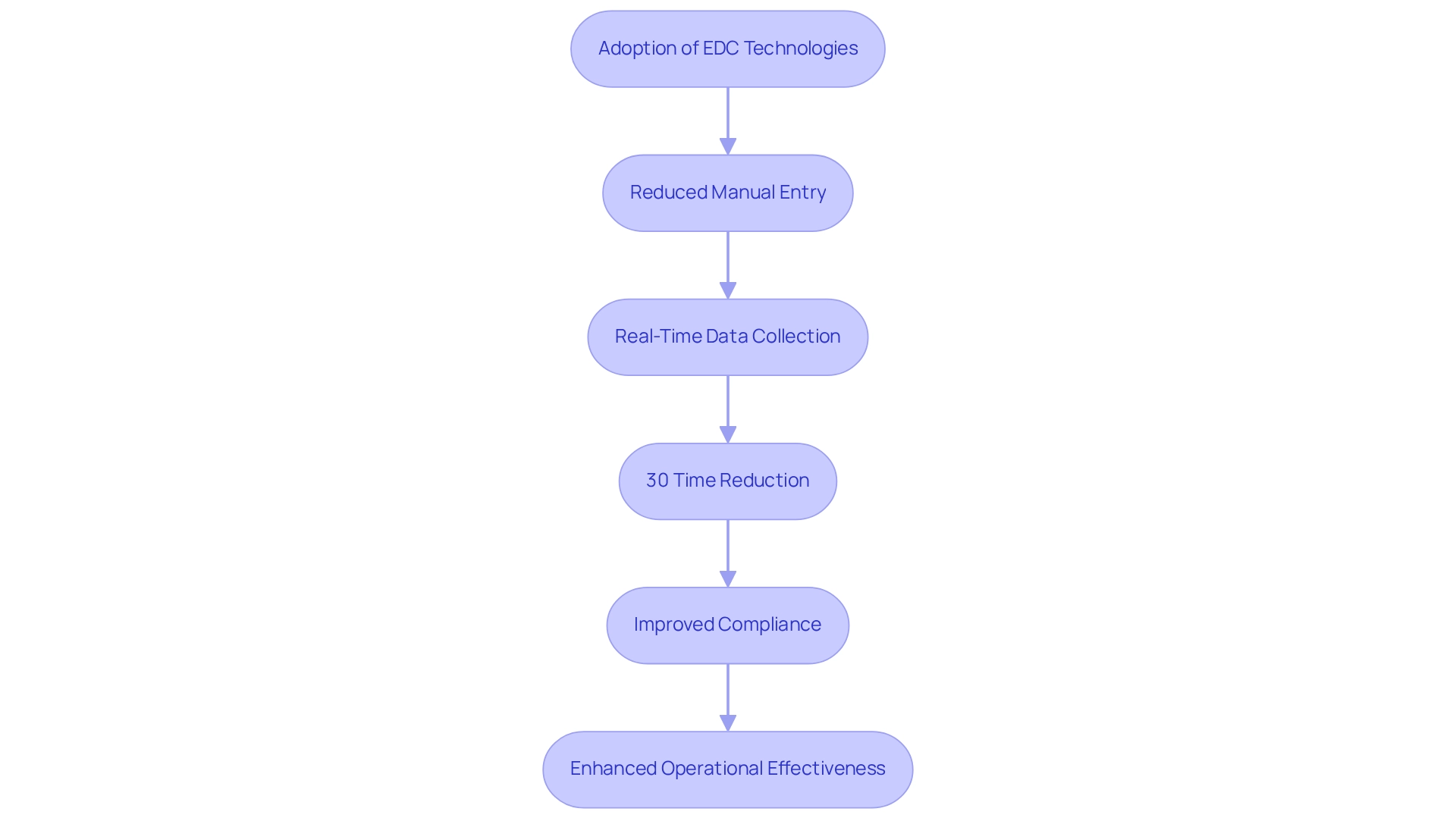
Streamlined Data Collection: Accelerating Clinical Trial Timelines with EDC
EDC frameworks significantly enhance the information gathering process by facilitating direct input from medical locations. This innovation drastically reduces the time spent on manual information entry, which is often plagued by delays inherent in paper-based methods. Consequently, studies can advance more swiftly, allowing researchers to collect and assess information in real-time. This acceleration not only streamlines the overall evaluation timeline but also bolsters compliance with regulatory requirements by maintaining an audit trail that ensures transparency and integrity throughout the process, especially with the remarkable growth and utilization of clinical trial EDC platforms that highlight their effectiveness in supporting research and translational studies.
For instance, organizations employing clinical trial EDC technologies have reported average time reductions of up to 30% in clinical trial timelines compared to traditional methods. Additionally, features like the Slider Bar or Visual Analog Scale in REDCap demonstrate how EDC platforms facilitate efficient data collection. This efficiency is crucial, especially in an environment where timely information can significantly influence patient outcomes and market access strategies.
Expert insights underscore that the streamlined data gathering enabled by EDC solutions not only enhances operational effectiveness but also fosters a more agile response to emerging challenges in data management. As Jerry C Parker, Associate Dean for Research at MU School of Medicine, notes, the adoption of EDC technologies is transforming the landscape of medical studies. As medical researchers increasingly recognize these advantages, the shift towards clinical trial EDC is expected to continue, further enhancing the efficacy of medical research.
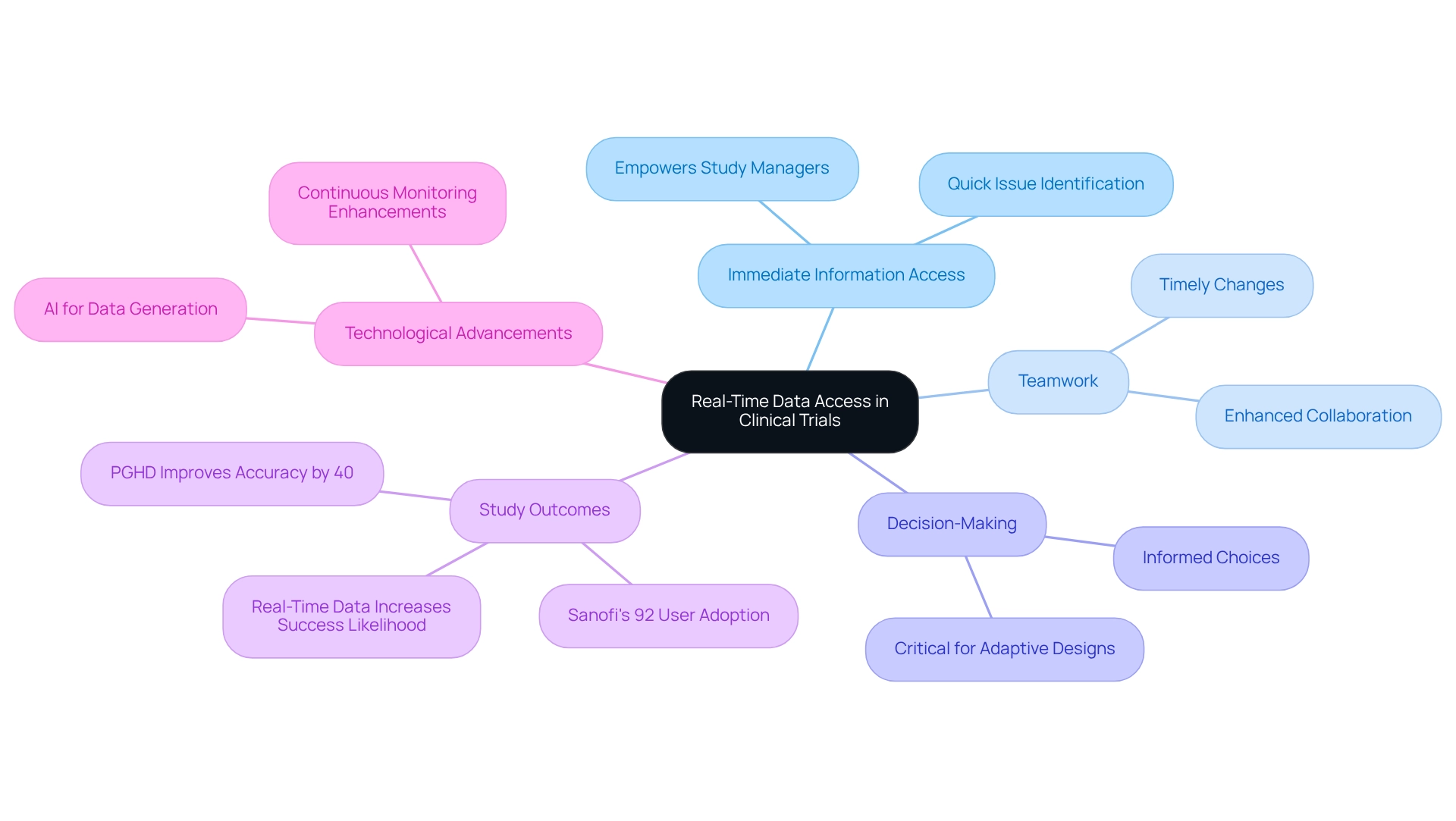
Real-Time Data Access: Facilitating Immediate Decision-Making in Trials
A notable benefit of clinical trial EDC systems is their provision of immediate information access, which empowers study managers to oversee progress, quickly identify issues, and make informed choices. This promptness in information availability fosters improved teamwork among stakeholders, facilitating timely changes that can significantly enhance study results.
For instance, studies have shown that patient-generated health information (PGHD) can improve outcome assessment accuracy by 40%, underscoring the critical role of real-time insights in clinical environments. Furthermore, the ability to obtain reliable information in real-time is essential for informed decision-making, particularly in flexible study designs where rapid modifications are crucial for success.
A case study illustrates that real-time information access enables swift decision-making, ultimately increasing the likelihood of successful outcomes. As emphasized by industry experts, the integration of real-time information in clinical trial EDC not only streamlines operations but also enhances the overall effectiveness of medical studies, making it a vital component of contemporary research management.
Additionally, Sanofi’s ‘Digital Clinical Trials’ initiative achieved an impressive 92% user adoption of new digital tools within six months, showcasing the efficacy of clinical trial EDC in boosting user engagement and operational efficiency. The ongoing advancements in research study information management further enhance precision, ensuring stakeholders can rely on the information they receive.
As Ibrahim Kamstrup-Akkaoui, Vice President of Data Systems Innovation, stated, “We conducted a small AI project to determine if we can create significant test information for establishing and verifying our frameworks. It turns out we can.” This highlights how cutting-edge technologies are being employed to improve information generation and verification in clinical studies.
Improved Regulatory Compliance: Meeting Industry Standards with EDC
Clinical trial EDC systems are meticulously crafted to meet stringent regulatory requirements, ensuring that information collection and management align with industry standards. Essential features such as audit trails, information encryption, and secure access controls are vital for maintaining the integrity and confidentiality of experimental data. For instance, audit trails provide a comprehensive record of all information modifications, fostering transparency and accountability throughout the process. This capability is crucial, as compliance officers stress that robust audit trails are indispensable for effective information management and regulatory adherence.
Moreover, the implementation of clinical trial EDC technologies significantly mitigates the risk of regulatory issues that could hinder study approval. The FDA’s updated guidance underscores the necessity of safeguarding digital health technology (DHT) information from unauthorized alterations, a challenge that EDC frameworks adeptly address through their advanced security measures. By preserving information integrity, clinical trial EDC platforms not only facilitate compliance but also enhance the overall efficacy of research studies.
Recent statistics indicate that concerns regarding regulatory compliance remain a substantial barrier in clinical studies, with many investigations facing delays due to inadequate information management practices. As Infonetica articulates, “As you move forward, remember that your commitment to compliance directly impacts the lives of countless individuals relying on medical breakthroughs.” Clinical trial EDC frameworks have proven to be transformative in this regard, providing a structured approach to data capture that aligns with contemporary regulatory standards. Case studies reveal that organizations employing EDC solutions have successfully navigated complex compliance landscapes, resulting in expedited timelines and improved outcomes. For example, the case study titled “Leveraging Technology for Continuous Learning” demonstrates how technology enhances compliance training and engagement, reinforcing the overarching message about the significance of regulatory compliance.
In conclusion, the regulatory compliance advantages of clinical trial EDC solutions are evident. They empower research study sponsors to efficiently meet industry standards by utilizing clinical trial EDC, ensuring that the information collected is not only reliable but also compliant with regulatory expectations. As the landscape of medical research evolves, particularly in light of the COVID-19 pandemic’s influence on remote technologies, the role of EDC frameworks in safeguarding information integrity and fostering compliance will remain paramount.

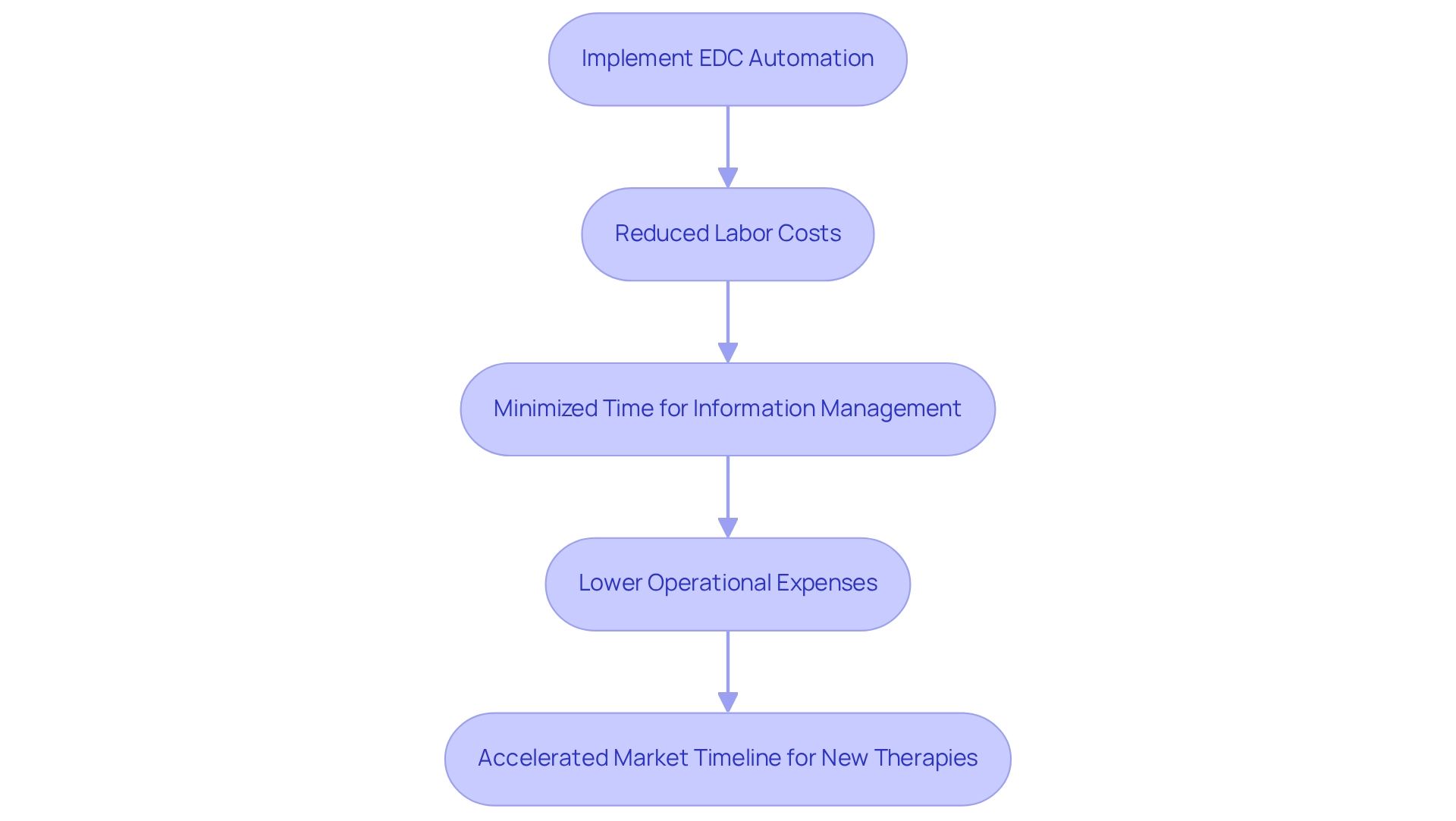
Cost Efficiency: Reducing Clinical Trial Expenses with EDC Automation
Introducing clinical trial edc solutions yields substantial financial advantages in research studies. By automating information gathering and diminishing the reliance on paper-based processes, clinical trial edc solutions significantly reduce labor costs and minimize the time required for information management. This heightened efficiency not only cuts operational expenses but also accelerates the timeline for bringing new therapies to market. Such advancements position organizations to capitalize on emerging opportunities in the healthcare landscape.
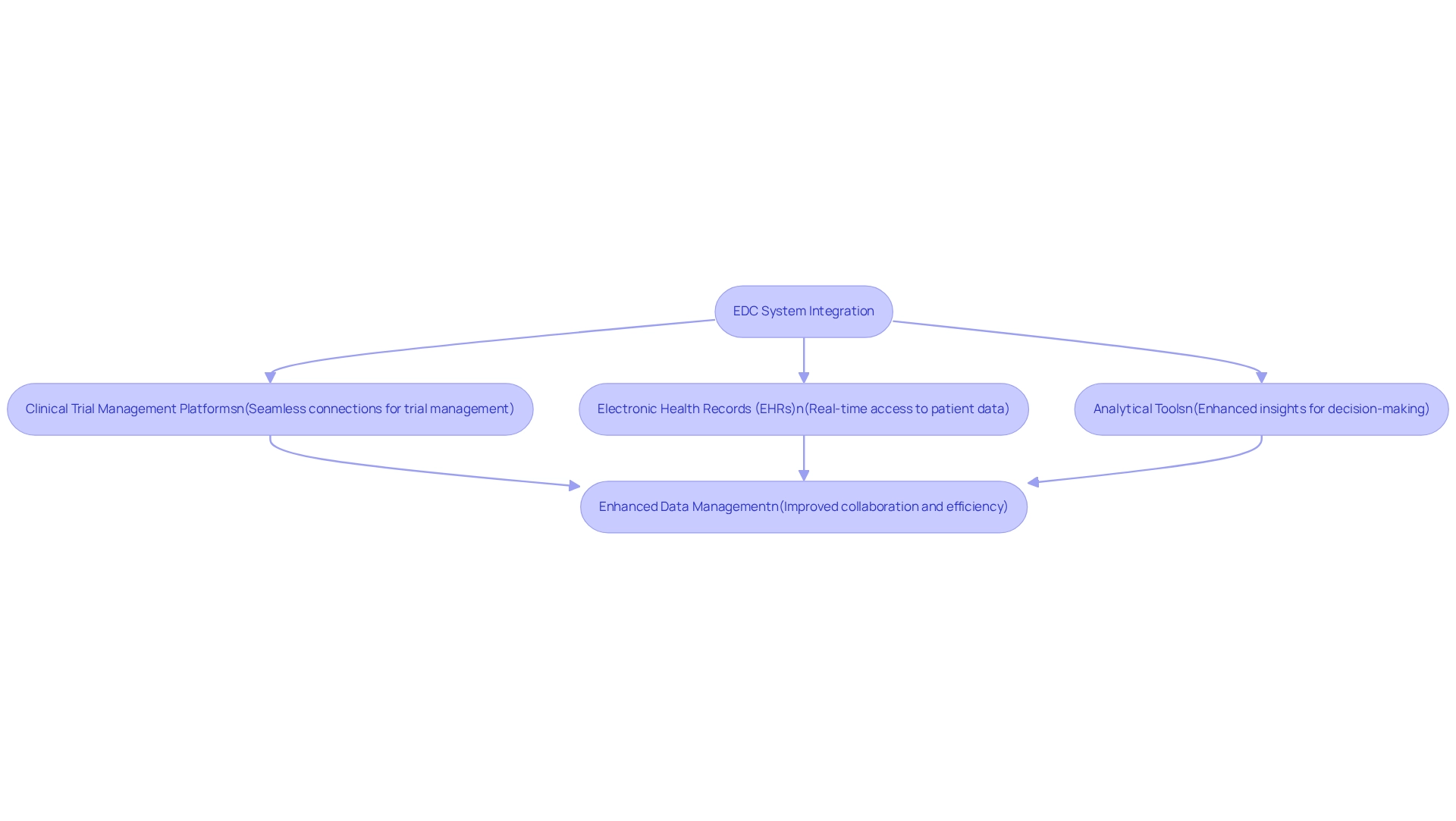
Integration Capabilities: Enhancing Data Management through EDC System Interoperability
EDC frameworks are designed with robust integration features, facilitating seamless connections with various clinical trial management platforms, electronic health records (EHRs), and analytical tools. This interoperability is crucial for enhancing information management, as it consolidates all relevant details onto a single platform. By optimizing the exchange of information between systems, EDC solutions foster improved collaboration among stakeholders and significantly reduce the risk of information silos.
For example, CareSet’s innovative Medicare information solutions exemplify this integration potential. By leveraging comprehensive insights from Medicare claims, including Parts A, B, and D, CareSet enhances the management process, enabling a deeper understanding of patient journeys and therapeutic treatments. This capability not only supports straightforward integration with existing systems but also facilitates targeted source information verification, thereby improving overall management efficiency and quality in research studies. For pharmaceutical market access managers, such features are essential for ensuring that information is accurate and readily accessible for strategic decision-making.
The impact of interoperability on information management in clinical trials is profound. It enables real-time access to and sharing of information, which is vital for timely decision-making and monitoring. Current statistics indicate that EDC systems can connect with over 100 external information sources, providing comprehensive insights that inform strategic initiatives. This level of integration directly enhances research efficiency by ensuring that all relevant information is accessible and actionable.
Experts in the field emphasize the importance of interoperability in studies, noting that it significantly improves the quality of information collected and analyzed. Jay Holmgren, PhD, MHI, underscores that overcoming challenges in research studies is critical for success. As clinical trials become increasingly complex, the ability to link EDC networks with EHRs and other analytical tools will be essential for improving trial outcomes and ensuring regulatory compliance. To effectively evaluate EDC solutions, pharmaceutical market access managers should prioritize options that demonstrate strong integration capabilities, ensuring they can leverage extensive information for enhanced decision-making. Additionally, consider implementing regular training sessions for your team to maximize the benefits of these integrated solutions.
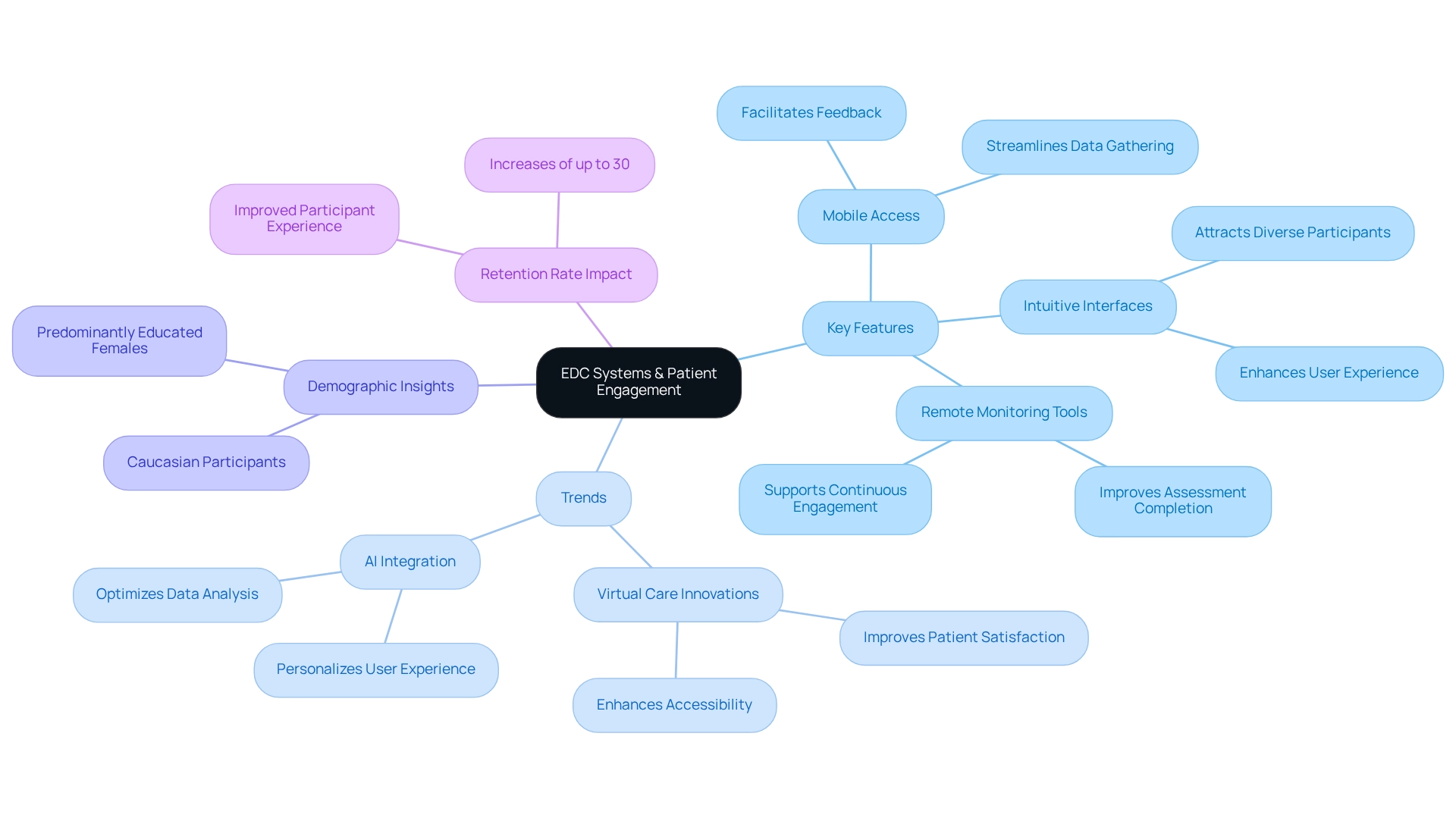
Improved Patient Engagement: Enhancing Participant Retention with EDC Systems
EDC frameworks significantly enhance patient involvement by streamlining the data gathering process for participants. Features such as mobile access, intuitive interfaces, and remote monitoring tools facilitate easier feedback and assessment completion. This improved participant experience is crucial; research indicates that effective engagement strategies can lead to retention rate increases of up to 30% in research studies.
Furthermore, the latest trends in patient experience, including virtual care innovations and the integration of AI, are pivotal in enhancing the effectiveness of EDC platforms. For instance, a demographic analysis of PRE-ACT users highlighted that a user-friendly interface was vital in attracting a diverse participant base, predominantly educated females and Caucasian participants.
By prioritizing patient experience and leveraging these trends, EDC frameworks not only foster higher retention rates but also contribute to the overall success of medical studies, ensuring that vital information is collected both efficiently and effectively.
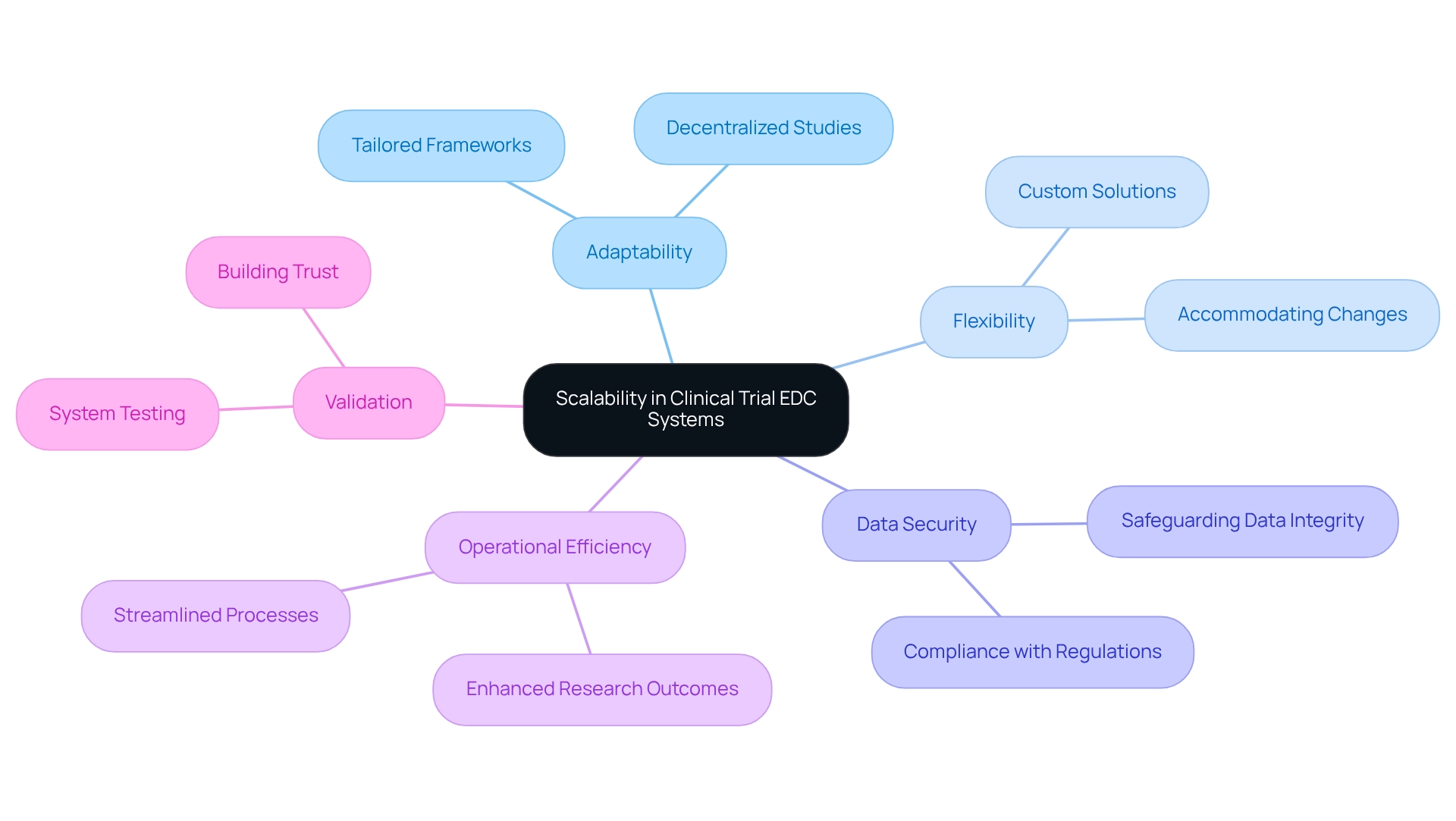
Scalability: Adapting EDC Systems to Diverse Clinical Trial Needs
The scalable nature of clinical trial EDC frameworks makes them ideal for research of all sizes, from small pilot studies to extensive multi-site studies. This scalability empowers researchers to tailor the framework to their specific needs, effectively managing various volumes and complexities of information. As research experiments evolve, EDC platforms can be seamlessly modified to accommodate changing requirements, minimizing disruptions and preserving data integrity.
The COVID-19 pandemic has accelerated the adoption of decentralized and remote studies, underscoring the necessity for adaptable clinical trial EDC solutions capable of addressing these emerging challenges. A robust clinical trial EDC solution not only ensures data security and user-friendliness but also enhances operational efficiency, ultimately leading to more successful clinical research outcomes.
Comprehensive testing and validation of clinical trial EDC systems are essential prior to deployment, ensuring compliance with industry regulations and safeguarding data integrity. Efficient validation fosters trust among research teams in the clinical trial EDC, confirming the reliability of the platform throughout the study. As Meri Beckwith, Co-Founder, notes, “By utilizing the knowledge of organizations such as Lindus Health, CROs can improve their operational efficiency and ultimately provide more effective research outcomes.”
Moreover, as experiments vary in size and scope, the clinical trial EDC platforms can adapt to these differences, providing customized solutions that meet specific research needs. This flexibility is vital for optimizing the research process and achieving favorable outcomes.
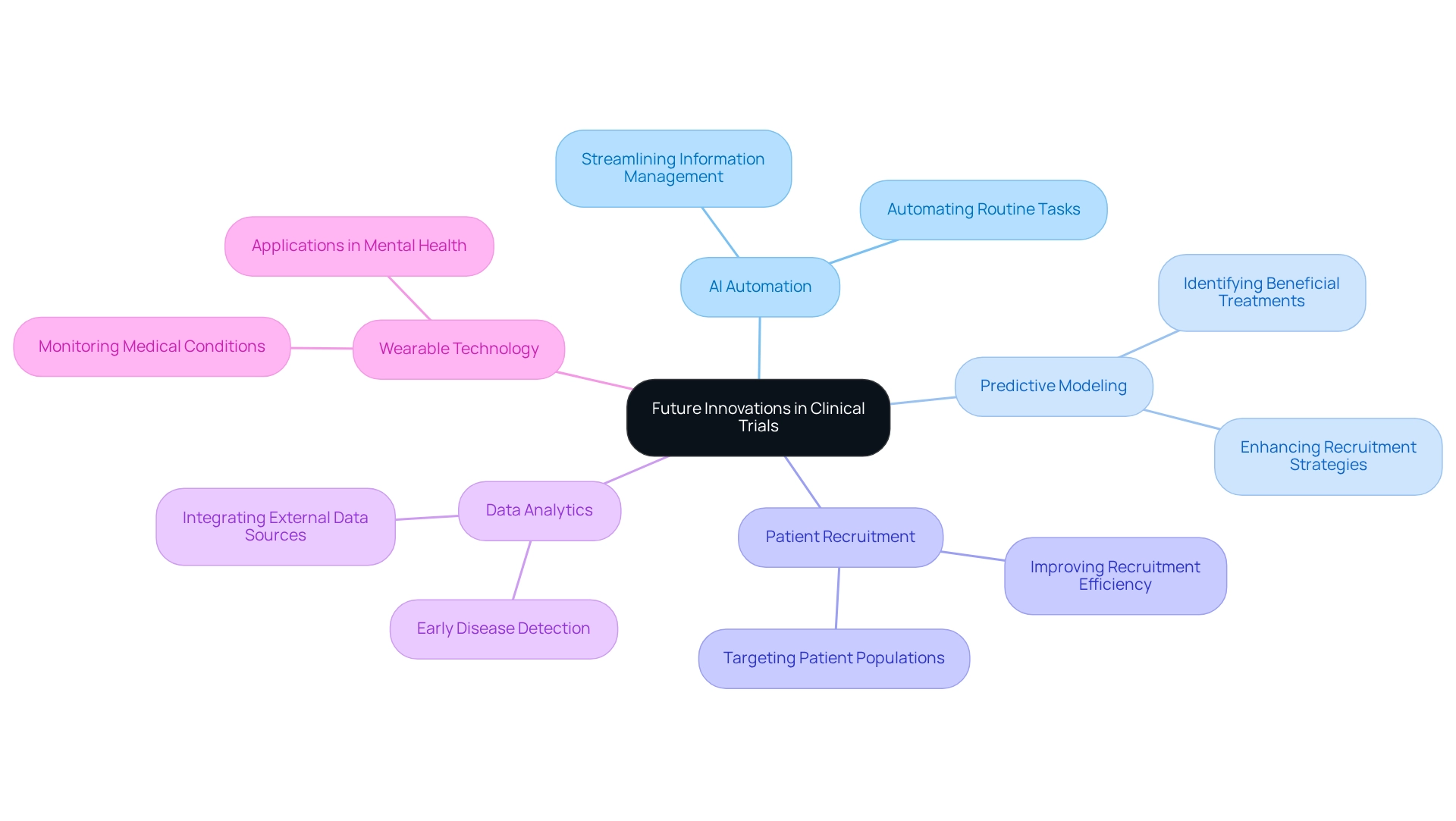
Future Innovations: Leveraging AI and Machine Learning in EDC Systems
The incorporation of artificial intelligence (AI) and machine learning into clinical trial EDC systems is poised to revolutionize clinical studies significantly. These advanced technologies automate routine tasks, streamline information management, and enhance the precision of predictive modeling for outcomes. By harnessing AI, researchers can extract deeper insights from complex datasets, optimize trial designs, and expedite the development of innovative therapies.
For instance, improvements in predictive modeling have shown promise in identifying patient populations more likely to benefit from specific treatments, thereby increasing the efficiency of recruitment strategies. Furthermore, the application of AI in information analysis can lead to earlier disease detection, which is crucial for preventive medicine and nursing care. CareSet’s groundbreaking analytics products, including those designed to evaluate Medicare information, position the company to leverage these advancements effectively, providing stakeholders with actionable insights that can enhance patient outcomes and promote business success.
The growing applications of Ethomix technology, which is exploring its wearable devices for various medical conditions, demonstrate how the adaptability of AI tools can significantly improve patient monitoring across numerous areas. This adaptability not only enhances patient care but also supports the broader objectives of medical research. Ethomix’s advancements exemplify how technology can transform patient management, aligning with CareSet’s mission to deliver comprehensive insights into treatment trends and patient experiences, particularly for the 62+ million Medicare beneficiaries and 6 million providers it supports, especially as current statistics reveal that the use of AI and machine learning in clinical trial EDC frameworks is rapidly expanding, with CareSet integrating over 100 external information sources into its analyses. This trend underscores the increasing reliance on advanced data analytics to inform clinical study strategies.
Experts in the field anticipate that these innovations will continue to evolve, further enhancing the capabilities of clinical trial EDC and ultimately leading to improved patient outcomes and more efficient trial processes. As Dr. Kei Adachi, an in-house physician overseeing policy underwriting assessments, noted, ‘In a year or so, we look to provide coverage to an additional 2,000 people who previously found it hard to get insurance.’ This perspective underscores the critical role of data-driven decision-making in enhancing healthcare access and outcomes.
Conclusion
The integration of Electronic Data Capture (EDC) systems into clinical trials represents a significant advancement in clinical research. By automating data collection, EDC systems enhance data quality and accuracy, which substantially reduces human error and bolsters the integrity of trial outcomes. The capacity to access real-time data empowers trial managers to make informed decisions swiftly, fostering collaboration and optimizing trial results.
Furthermore, EDC systems streamline data collection processes, thereby accelerating trial timelines and ensuring compliance with regulatory standards. Their robust integration capabilities facilitate seamless connections with various data sources, enhancing data management and supporting informed decision-making. This interoperability is essential for improving clinical trial efficiency, as it enables stakeholders to access comprehensive insights that drive strategic actions.
Patient engagement emerges as another critical advantage of EDC systems, as they enhance the participant experience through user-friendly interfaces and mobile access, resulting in higher retention rates in trials. Additionally, the scalability of EDC systems renders them adaptable to trials of all sizes, accommodating evolving needs without compromising data integrity.
Looking ahead, the incorporation of artificial intelligence and machine learning into EDC systems is poised to further revolutionize clinical trials. These technologies promise to automate routine tasks, enhance predictive modeling, and ultimately improve patient outcomes. As the clinical research landscape continues to evolve, the role of EDC systems in driving efficiency, compliance, and innovation will remain paramount, ensuring that trials meet the demands of modern healthcare and deliver meaningful results.


